Abstract
Objective
To perform a systematic review of published literature for the factors reported to predict outcomes of enhanced recovery after surgery (ERAS) programmes following laparoscopic colorectal surgery.
Background
ERAS programmes and the use of laparoscopy have been widely adopted in colorectal surgery bringing short-term patient benefit. However, there is a minority of patients that do not benefit from these strategies and their identification is not well characterised. The factors that underpin outcomes from ERAS programmes for laparoscopic patients are not understood.
Methods
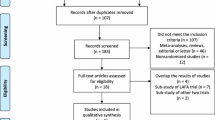
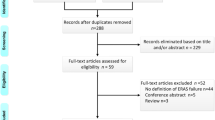
A systematic search of the MEDLINE, Embase and Cochrane databases was conducted to identify suitable articles published between 2000 and 2015. The search strategy captured terms for ERAS, colorectal resection, prediction and outcome measures.
Results
Thirty-four studies containing 10,861 laparoscopic resections were included. Thirty-one (91 %) studies were confined to elective cases. Predictive analysis of outcome was most frequently based on length of stay (LOS), morbidity and readmission which were the main outcome measures of 29 (85 %), 26 (76 %) and 18 (53 %) of the included studies, respectively. Forty-seven percentage of included studies investigated the impact of ERAS programme compliance on these outcomes. Reduced protocol compliance was the most frequently identified modifiable predictive factor for adverse LOS, morbidity and readmission.
Conclusion
Protocol compliance is the most frequently reported predictive factor for outcomes of ERAS programmes following laparoscopic colorectal resection. Reduced compliance increases LOS, morbidity and readmission to hospital. The impact of compliance with individual ERAS protocol elements is insufficiently studied, and the lack of a standardised framework for evaluating ERAS programmes makes it difficult to draw definite conclusions about which factors exert the greatest impact on outcome after laparoscopic colorectal resection.

Similar content being viewed by others
References
Senagore AJ (2015) Adoption of laparoscopic colorectal surgery: it was quite a journey. Clin Colon Rectal Surg 28(3):131–134
The UK National Bowel Cancer Audit Project 2015 (2015) Health and Social Care Information Centre
ERAS Society—Reference Centres Interactive Audit. 2016. 14-7-2016. Ref Type: Online Source
Basse L, Hjort JD, Billesbolle P, Werner M, Kehlet H (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232(1):51–57
Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW (2003) Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum 46(7):851–859
Anderson AD, McNaught CE, MacFie J, Tring I, Barker P, Mitchell CJ (2003) Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg 90(12):1497–1504
Gatt M, Anderson AD, Reddy BS, Hayward-Sampson P, Tring IC, MacFie J (2005) Randomized clinical trial of multimodal optimization of surgical care in patients undergoing major colonic resection. Br J Surg 92(11):1354–1362
Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA (2007) A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg 245(6):867–872
Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N (2009) A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology 136(3):842–847
Serclova Z, Dytrych P, Marvan J, Nova K, Hankeova Z, Ryska O et al (2009) Fast-track in open intestinal surgery: prospective randomized study (Clinical Trials Gov Identifier no. NCT00123456). Clin Nutr 28(6):618–624
Garcia-Botello S, de Canovas LR, Tornero C, Escamilla B, Espi-Macias A, Esclapez-Valero P et al (2011) Implementation of a perioperative multimodal rehabilitation protocol in elective colorectal surgery. A prospective randomised controlled study. Cir Esp 89(3):159–166
Ionescu D, Iancu C, Ion D, Al-Hajjar N, Margarit S, Mocan L et al (2009) Implementing fast-track protocol for colorectal surgery: a prospective randomized clinical trial. World J Surg 33(11):2433–2438
Lee TG, Kang SB, Kim DW, Hong S, Heo SC, Park KJ (2011) Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 54(1):21–28
Ren L, Zhu D, Wei Y, Pan X, Liang L, Xu J et al (2012) Enhanced Recovery After Surgery (ERAS) program attenuates stress and accelerates recovery in patients after radical resection for colorectal cancer: a prospective randomized controlled trial. World J Surg 36(2):407–414
Yang D, He W, Zhang S, Chen H, Zhang C, He Y (2012) Fast-track surgery improves postoperative clinical recovery and immunity after elective surgery for colorectal carcinoma: randomized controlled clinical trial. World J Surg 36(8):1874–1880
Walter CJ, Collin J, Dumville JC, Drew PJ, Monson JR (2009) Enhanced recovery in colorectal resections: a systematic review and meta-analysis. Colorectal Dis 11(4):344–353
Eskicioglu C, Forbes SS, Aarts MA, Okrainec A, McLeod RS (2009) Enhanced recovery after surgery (ERAS) programs for patients having colorectal surgery: a meta-analysis of randomized trials. J Gastrointest Surg 13(12):2321–2329
Spanjersberg WR, Reurings J, Keus F, van Laarhoven CJ (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev 2:CD007635
Lv L, Shao YF, Zhou YB (2012) The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Colorectal Dis 27(12):1549–1554
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z (2013) Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 56(5):667–678
Adamina M, Kehlet H, Tomlinson GA, Senagore AJ, Delaney CP (2011) Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 149(6):830–840
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF et al (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254(6):868–875
Lawrence JK, Keller DS, Samia H, Ermlich B, Brady KM, Nobel T et al (2013) Discharge within 24 to 72 hours of colorectal surgery is associated with low readmission rates when using Enhanced Recovery Pathways. J Am Coll Surg 216(3):390–394
Keller DS, Champagne BJ, Reynolds HL Jr, Stein SL, Delaney CP (2014) Cost-effectiveness of laparoscopy in rectal cancer. Dis Colon Rectum 57(5):564–569
Keller DS, Delaney CP, Hashemi L, Haas EM (2015) A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc. doi:10.1007/s00464-015-4732-6
Keller DS, Lawrence JK, Nobel T, Delaney CP (2013) Optimizing cost and short-term outcomes for elderly patients in laparoscopic colonic surgery. Surg Endosc 27(12):4463–4468
Senagore AJ, Whalley D, Delaney CP, Mekhail N, Duepree HJ, Fazio VW (2001) Epidural anesthesia-analgesia shortens length of stay after laparoscopic segmental colectomy for benign pathology. Surgery 129(6):672–676
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM et al (2014) Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg 101(3):159–170
Feldman LS, Lee L, Fiore J Jr (2015) What outcomes are important in the assessment of Enhanced Recovery After Surgery (ERAS) pathways? Can J Anaesth 62(2):120–130
Keller DS, Swendseid B, Khorgami Z, Champagne BJ, Reynolds HL Jr, Stein SL et al (2014) Predicting the unpredictable: comparing readmitted versus non-readmitted colorectal surgery patients. Am J Surg 207(3):346–351
Keller DS, Bankwitz B, Nobel T, Delaney CP (2014) Using frailty to predict who will fail early discharge after laparoscopic colorectal surgery with an established recovery pathway. Dis Colon Rectum 57(3):337–342
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146(5):571–577
Boulind CE, Yeo M, Burkill C, Witt A, James E, Ewings P et al (2012) Factors predicting deviation from an enhanced recovery programme and delayed discharge after laparoscopic colorectal surgery. Colorectal Dis 14(3):e103–e110
ERAS Compliance Group (2015) The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg 261(6):1153–1159
Francis NK, Allison A, Ockrim J (2012) Success and failure in colorectal enhanced recovery. In: Francis NK, Kennedy RH, Ljungqvist O, Mythen MG (eds) Manual of fast track recovery for colorectal surgery. Springer, London, pp 159–170
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Higgins JPT, Altman DG, Stone JAC (2011) Assessing risk of bias in included studies. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions. 5.1.0 ed. The Cochrane Collaboration
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH et al (2006) Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 93(3):300–308
King PM, Blazeby JM, Ewings P, Kennedy RH (2008) Detailed evaluation of functional recovery following laparoscopic or open surgery for colorectal cancer within an enhanced recovery programme. Int J Colorectal Dis 23(8):795–800
Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA (2011) Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg 98(8):1068–1078
Wongyingsinn M, Baldini G, Charlebois P, Liberman S, Stein B, Carli F (2011) Intravenous lidocaine versus thoracic epidural analgesia: a randomized controlled trial in patients undergoing laparoscopic colorectal surgery using an enhanced recovery program. Reg Anesth Pain Med 36(3):241–248
Wongyingsinn M, Baldini G, Stein B, Charlebois P, Liberman S, Carli F (2012) Spinal analgesia for laparoscopic colonic resection using an enhanced recovery after surgery programme: better analgesia, but no benefits on postoperative recovery: a randomized controlled trial. Br J Anaesth 108(5):850–856
Zakhaleva J, Tam J, Denoya PI, Bishawi M, Bergamaschi R (2013) The impact of intravenous fluid administration on complication rates in bowel surgery within an enhanced recovery protocol: a randomized controlled trial. Colorectal Dis 15(7):892–899
Ihedioha U, Vaughan S, Mastermann J, Singh B, Chaudhri S (2013) Patient education videos for elective colorectal surgery: results of a randomized controlled trial. Colorectal Dis 15(11):1436–1441
Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP et al (2014) Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol 32(17):1804–1811
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121(5):937–947
Loftus TJ, Stelton S, Efaw BW, Bloomstone J (2015) A system-wide enhanced recovery program focusing on two key process steps reduces complications and readmissions in patients undergoing bowel surgery. J Healthc Qual. doi:10.1111/jhq.12068
Senagore AJ, Madbouly KM, Fazio VW, Duepree HJ, Brady KM, Delaney CP (2003) Advantages of laparoscopic colectomy in older patients. Arch Surg 138(3):252–256
Conaghan P, Maxwell-Armstrong C, Bedforth N, Gornall C, Baxendale B, Hong LL et al (2010) Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc 24(10):2480–2484
Pawa N, Cathcart PL, Arulampalam TH, Tutton MG, Motson RW (2012) Enhanced recovery program following colorectal resection in the elderly patient. World J Surg 36(2):415–423
Gorissen KJ, Benning D, Berghmans T, Snoeijs MG, Sosef MN, Hulsewe KW et al (2012) Risk of anastomotic leakage with non-steroidal anti-inflammatory drugs in colorectal surgery. Br J Surg 99(5):721–727
Zittel TT, Razavi D, Papp A, Lundberg K (2013) Increased risk for complications after colorectal surgery with selective cyclo-oxygenase 2 inhibitor etoricoxib. Dis Colon Rectum 56(6):761–767
Lohsiriwat V (2014) The influence of preoperative nutritional status on the outcomes of an enhanced recovery after surgery (ERAS) programme for colorectal cancer surgery. Tech Coloproctol 18(11):1075–1080
Martin TD, Lorenz T, Ferraro J, Chagin K, Lampman RM, Emery KL et al (2016) Newly implemented enhanced recovery pathway positively impacts hospital length of stay. Surg Endosc 30(9):4019–4028
Chand M, De’Ath HD, Rasheed S, Mehta C, Bromilow J, Qureshi T (2016) The influence of peri-operative factors for accelerated discharge following laparoscopic colorectal surgery when combined with an enhanced recovery after surgery (ERAS) pathway. Int J Surg 25:59–63
Smart NJ, White P, Allison AS, Ockrim JB, Kennedy RH, Francis NK (2012) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 14(10):e727–e734
Walter CJ, Watson JT, Pullan RD, Kenefick NJ, Mitchell SJ, Defriend DJ (2011) Enhanced recovery in major colorectal surgery: safety and efficacy in an unselected surgical population at a UK district general hospital. Surgeon 9(5):259–264
Vlug MS, Bartels SA, Wind J, Ubbink DT, Hollmann MW, Bemelman WA (2012) Which fast track elements predict early recovery after colon cancer surgery? Colorectal Dis 14(8):1001–1008
Aarts MA, Okrainec A, Glicksman A, Pearsall E, Victor JC, McLeod RS (2012) Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc 26(2):442–450
Srinivasa S, Singh SP, Kahokehr AA, Taylor MH, Hill AG (2012) Perioperative fluid therapy in elective colectomy in an enhanced recovery programme. ANZ J Surg 82(7–8):535–540
Lane JC, Wright S, Burch J, Kennedy RH, Jenkins JT (2013) Early prediction of adverse events in enhanced recovery based upon the host systemic inflammatory response. Colorectal Dis 15(2):224–230
Feroci F, Lenzi E, Baraghini M, Garzi A, Vannucchi A, Cantafio S et al (2013) Fast-track colorectal surgery: protocol adherence influences postoperative outcomes. Int J Colorectal Dis 28(1):103–109
Cakir H, van Stijn MF, Lopes Cardozo AM, Langenhorst BL, Schreurs WH, van der Ploeg TJ et al (2013) Adherence to enhanced recovery after surgery and length of stay after colonic resection. Colorectal Dis 15(8):1019–1025
Rossi G, Vaccarezza H, Vaccaro CA, Mentz RE, Im V, Alvarez A et al (2013) Two-day hospital stay after laparoscopic colorectal surgery under an enhanced recovery after surgery (ERAS) pathway. World J Surg 37(10):2483–2489
Keller DS, Bankwitz B, Woconish D, Champagne BJ, Reynolds HL Jr, Stein SL et al (2014) Predicting who will fail early discharge after laparoscopic colorectal surgery with an established enhanced recovery pathway. Surg Endosc 28(1):74–79
Agrafiotis AC, Corbeau M, Buggenhout A, Katsanos G, Ickx B, Van de Stadt J (2014) Enhanced recovery after elective colorectal resection outside a strict fast-track protocol. A single centre experience. Int J Colorectal Dis 29(1):99–104
Larson DW, Lovely JK, Cima RR, Dozois EJ, Chua H, Wolff BG et al (2014) Outcomes after implementation of a multimodal standard care pathway for laparoscopic colorectal surgery. Br J Surg 101(8):1023–1030
Oh HK, Ihn MH, Son IT, Park JT, Lee J, Kim DW et al (2016) Factors associated with failure of enhanced recovery programs after laparoscopic colon cancer surgery: a single-center retrospective study. Surg Endosc 30(3):1086–1093
Bakker N, Cakir H, Doodeman HJ, Houdijk AP (2015) Eight years of experience with enhanced recovery after surgery in patients with colon cancer: impact of measures to improve adherence. Surgery 157(6):1130–1136
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N et al (2012) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS(R)) Society recommendations. Clin Nutr 31(6):783–800
Whistance RN, Forsythe RO, McNair AG, Brookes ST, Avery KN, Pullyblank AM et al (2013) A systematic review of outcome reporting in colorectal cancer surgery. Colorectal Dis 15(10):e548–e560
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 3:CD003145
Shandall A, Lowndes R, Young HL (1985) Colonic anastomotic healing and oxygen tension. Br J Surg 72(8):606–609
Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP (2002) Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet 359(9320):1812–1818
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Allvin R, Berg K, Idvall E, Nilsson U (2007) Postoperative recovery: a concept analysis. J Adv Nurs 57(5):552–558
Maessen JM, Dejong CH, Kessels AG, von Meyenfeldt MF (2008) Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg 32(6):971–975
OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. 4-3-2015. University of Oxford. Ref Type: Online Source
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
David E. Messenger, Nathan J. Curtis, Adam Jones, Emma L. Jones, Neil J. Smart and Nader K. Francis have no conflicts of interest or financial ties to disclose.
Additional information
David E. Messenger and Nathan J. Curtis have contributed equally to this manuscript and share first authorship.
Appendices
Appendix 1
Search terms used to identify studies for inclusion in the review. Four sets of search criteria were used and were combined using the Boolean operator ‘AND’
Enhanced recovery after surgery |
enhanced recovery.tw. OR eras.tw. OR rapid recovery.tw. OR (fast and track).tw. OR multimodal.tw. OR multi-modal.tw. OR accelerated discharge.tw. OR early discharge.tw. OR early rehabilitation.tw OR clinical pathway.tw. OR accelerated pathway.tw. OR integrated care pathway.tw |
Colorectal resection |
colorectal.tw. OR colo-rectal.tw. OR colo-rectal cancer.tw. OR colorectal cancer.tw. OR CRC.tw. OR bowel.tw. OR bowel resect$.tw. OR bowel surg$.tw. OR colon$.tw. OR rect$.tw. OR proctectomy.tw. OR colectomy.tw. OR segmental colectomy.tw. |
Prediction |
Prognostic.tw. OR prognosis.tw. OR predictive.tw. OR predict$.tw. OR risk.tw. OR risk factor.tw. OR risk factors.tw. OR early detection.tw. OR early warning.tw. OR risk.mp OR predict$.mp. OR impact.tw. |
Outcome measures |
length of stay.tw. OR exp ‘Length of Stay’/OR hospital stay.tw. OR length of hospital stay.tw. OR Patient Discharge.tw. OR patient stay.mp. OR discharge.mp. OR re-admission.tw. OR readmission.tw. OR morbid$.tw OR Postoperative Complications/co, me, mi, mo, ph, pp, su, ur, vi OR (return and to).mp. and theatre.tw. OR complication$.tw. OR mortal$.tw. OR *Neoplasms/OR *Aged/OR *Opportunistic Infections/OR success$.mp. OR failure$.mp. OR Quality of Life.tw. OR qol.tw. OR hrql.tw. OR hrqol.tw. OR patient reported outcome.tw. OR patient-reported outcome.tw. OR patient reported outcome measure.tw. OR patient-reported outcome measure.tw. OR health stat$.tw. OR health stat*.tw. OR PRO.mp. OR PROM.mp. OR pain.mp. OR Pain/cl, co, di, dt, et, hi, im, me, mi, mo, nu, pa, ph, pp, pc, px, rt, st, su OR physical function.tw. OR fatigue.tw. OR well being.tw. OR well-being.tw. OR Euroqol.tw. OR EQ-5D.tw. OR EQ-3D.tw. OR Gastrointestinal quality of life index.tw. OR GIQLI.tw. OR SF-36.tw |
Appendix 2: Data extraction form

Appendix 3
Cochrane Collaboration’s tool for assessing risk of bias in randomised studies 28 included in the review
Author, journal | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | |
|---|---|---|---|---|---|---|---|
Random sequence generation | Allocation concealment | ||||||
King et al., Br J Surg [39] (and King et al., Int J Col Dis [40]) | + | ? | − | − | + | + | + |
Levy et al., Br J Surg [41] | + | + | − | − | + | + | + |
Wongyingsinn et al., Reg Anesth Pain Med [42] | + | + | − | + | + | + | + |
Wongyingsinn et al., Br J Anaesth [43] | + | + | − | − | + | + | + |
Zakhaleva et al., Colorectal Dis [44] | + | + | − | − | − | + | − |
Ihedioha et al., Colorectal Dis [45] | + | ? | ? | ? | + | ? | ? |
Kennedy et al., J Clin Onc [46] | + | + | + | ? | + | + | + |
Gillis et al., Anesthesiology [47] | + | + | − | + | + | + | + |
Appendix 4
The MINORS criteria [29] and scores applied to non-randomised studies included in the review
Author, journal | A clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | Endpoints appropriate to the aim of the study | Unbiased assessment of the study endpoint | Follow-up period appropriate to the aim of the study | Loss to follow-up of less than 5 % | Prospective calculation of the study size | Additional criteria for comparative studies | Total | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
An adequate control group | Contemporary groups | Baseline equivalence of groups | Adequate statistical analyses | ||||||||||
Loftus, J Healthcare Qual [48] | 2 | 1 | 0 | 2 | 1 | 2 | 2 | 0 | 1 | 0 | 1 | 2 | 14 |
Senagore, Arch Surg [49] | 1 | 2 | 1 | 1 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 1 | 14 |
Conaghan, Surg Endosc [50] | 1 | 2 | 2 | 0 | 0 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 13 |
Pawa, World J Surg [51] | 1 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | 1 | 2 | 0 | 1 | 14 |
Gorissen, Br J Surg [52] | 1 | 2 | 0 | 2 | 0 | 1 | 1 | 0 | 1 | 2 | 1 | 2 | 13 |
Zittel, Dis Colon Rectum [53] | 2 | 0 | 1 | 2 | 0 | 1 | 1 | 0 | 1 | 2 | 2 | 2 | 14 |
Lohsiriwat, Tech Coloproctol [54] | 1 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 1 | 16 |
Martin, Surg Endosc [55] | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | 1 | 0 | 1 | 2 | 15 |
Walter, Surgeon [58] | 2 | 1 | 2 | 2 | 0 | 1 | 1 | 0 | NA | NA | NA | NA | 9 |
Gustafsson et al., Arch Surg [32] | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | NA | NA | NA | NA | 12 |
ERAS Compliance Group, Ann Surg [34] | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | NA | NA | NA | NA | 14 |
Smart et al., Colorectal Dis [57] | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
Chand, Int J Surg [56] | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
Vlug et al., Colorectal Dis [59] | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | NA | NA | NA | NA | 15 |
Aarts et al., Surg Endosc [60] | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 12 |
Srinivasa et al., ANZ J Surg [61] | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 9 |
Lane et al., Colorectal Dis [62] | 1 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 11 |
Feroci et al., Int J Colorectal Dis [63] | 1 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 11 |
Cakir et al., Colorectal Dis [64] | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 9 |
Rossi et al., World J Surg [65] | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 12 |
Keller et al., Surg Endosc [66] | 1 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
Agrafiotis et al., Int J Colorectal Dis [67] | 1 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | NA | NA | NA | NA | 7 |
Larson et al., Br J Surg [68] | 2 | 2 | 1 | 2 | 0 | 1 | 2 | 0 | NA | NA | NA | NA | 10 |
Oh, Surg Endosc [69] | 1 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
Bakker, Surgery [70] | 1 | 2 | 2 | 1 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
Rights and permissions
About this article
Cite this article
Messenger, D.E., Curtis, N.J., Jones, A. et al. Factors predicting outcome from enhanced recovery programmes in laparoscopic colorectal surgery: a systematic review. Surg Endosc 31, 2050–2071 (2017). https://doi.org/10.1007/s00464-016-5205-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5205-2