Abstract
Background
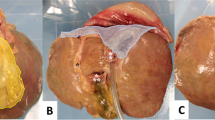
Suture skills are essential to laparoscopic liver resection. The current suture training models are not ideal enough. The aim of this study is to develop and verify a highly simulated-bleeding continuously perfused training model (CPTM) and to evaluate its training efficacy.
Methods
CPTM was constructed using fresh lamb liver whose portal veins were perfused with red-dyed liquid gelatin. Construct validity of CPTMs was tested in 33 participants with three levels of laparoscopic experience (experts, intermediates, and novices) who were demanded to finish one superficial stitch and one deep stitch for suture hemostasis on CPTMs. The CPTMs were also evaluated by the experts. CPTMs were compared with dry box training models (DBTMs) regarding training efficacy among the novices who were assigned to DBTM and CPTM groups to, respectively, complete a 10-day training on CPTMs or DBTMs. Before and after their assignments, their superficial stitches were assessed by completion time, suture accuracy, and suture knot performance while their deep stitches by completion time and bleeding control.
Results
CPTM proved to be construct valid by both superficial and deep stitches. Significant differences were found regarding completion time (763, 271, 174 s), suture accuracy (4.4, 1.8, 0.2 mm), and suturing knot performance (12.1, 21.5, 22.0) for superficial stitches (p < 0.001), as well as regarding completion time (807, 423, 277 s) for deep stitches (p < 0.001). Positive comments were given by all experts. CPTMs helped novices to acquire laparoscopic suture skills. Their training efficacy was significantly better than that of DBTMs (p < 0.05). Learning curves of CPTM group plateaued at the sixth round for superficial stitches and at the seventh round for deep stitches.
Conclusion
CPTM offers trainees a highly simulated-bleeding means to acquire advanced laparoscopic suture skills. The suture skills learned on CPTMs may improve significantly at the seventh round.







Similar content being viewed by others
References
Chang SK, Lee CS, Hlaing WW et al (2011) Vascularised porcine liver model for surgical training. Med Educ 45:520
Otsuka Y, Kaneko H, Cleary SP et al (2015) What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd international consensus conference on laparoscopic liver resection. J Hepatobiliary Pancreat Sci 22:363–370
Sarpel U, Ayo DM, Newman E (2012) Choice of device for parenchymal transection in laparoscopic hepatectomy. Surg Technol Int 22:33–38
Ieiri S, Ishii H, Souzaki R et al (2013) Development of an objective endoscopic surgical skill assessment system for pediatric surgeons: suture ligature model of the crura of the diaphragm in infant fundoplication. Pediatr Surg Int 29:501–504
Romero P, Brands O, Nickel F et al (2014) Intracorporal suturing—driving license necessary? J Pediatr Surg 49:1138–1141
Gomez PP, Willis RE, Schiffer BL et al (2014) External validation and evaluation of an intermediate proficiency-based knot-tying and suturing curriculum. J Surg Educ 71:839–845
Scott DJ, Goova MT, Tesfay ST (2007) A cost-effective proficiency-based knot-tying and suturing curriculum for residency programs. J Surg Res 141:7–15
Huang E, Chern H, O’Sullivan P et al (2014) A better way to teach knot tying: a randomized controlled trial comparing the kinesthetic and traditional methods. Am J Surg 208:690–694
Goova MT, Hollett LA, Tesfay ST et al (2008) Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ 65:309–315
Causer J, Vickers JN, Snelgrove R et al (2014) Performing under pressure: quiet eye training improves surgical knot-tying performance. Surgery 156:1089–1096
Rodrigues SP, Horeman T, Blomjous MS et al (2015) Laparoscopic suturing learning curve in an open versus closed box trainer. Surg Endosc 30:315–322
Wang H, Yang B, Xu C et al (2009) New practical course for laparoscopy training: anatomizing the orange. Eur Surg Res 42:106–108
Wong IH, Denkers M, Urquhart N et al (2013) Construct validity testing of the Arthroscopic Knot Trainer (ArK). Knee Surg Sports Traumatol Arthrosc 23:906–911
Wong J, Bhattacharya G, Vance SJ et al (2013) Construction and validation of a low-cost laparoscopic simulator for surgical education. J Surg Educ 70:443–450
Santos BF, Reif TJ, Soper NJ et al (2012) Development and evaluation of a laparoscopic common bile duct exploration simulator and procedural rating scale. Surg Endosc 26:2403–2415
Van Sickle KR, Ritter EM, Baghai M et al (2008) Prospective, randomized, double-blind trial of curriculum-based training for intracorporeal suturing and knot tying. J Am Coll Surg 207:560–568
Dehabadi M, Fernando B, Berlingieri P (2014) The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg 12:258–268
Korndorffer JJ, Dunne JB, Sierra R et al (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Strickland A, Fairhurst K, Lauder C et al (2011) Development of an ex vivo simulated training model for laparoscopic liver resection. Surg Endosc 25:1677–1682
Munz Y, Almoudaris AM, Moorthy K et al (2007) Curriculum-based solo virtual reality training for laparoscopic intracorporeal knot tying: objective assessment of the transfer of skill from virtual reality to reality. Am J Surg 193:774–783
Laird A, Stewart GD, Hou S et al (2011) A novel bovine model for training urological surgeons in laparoscopic radical nephrectomy. J Endourol 25:1377–1383
Stolzenburg J, Truss MC, Rabenalt R et al (2007) Training in laparoscopy. EAU-EBU Update Ser 5:53–62
Aggarwal R, Crochet P, Dias A et al (2009) Development of a virtual reality training curriculum for laparoscopic cholecystectomy. Br J Surg 96:1086–1093
Teh SH, Hunter JG, Sheppard BC (2007) A suitable animal model for laparoscopic hepatic resection training. Surg Endosc 21:1738–1744
Szinicz G, Beller S, Bodner W et al (1993) Simulated operations by pulsatile organ-perfusion in minimally invasive surgery. Surg Laparosc Endosc 3:315–317
Yang B, Zeng Q, Yinghao S et al (2009) A novel training model for laparoscopic partial nephrectomy using porcine kidney. J Endourol 23:2029–2033
Nam SM, Shin HS, Kim YB et al (2013) Microsurgical training with porcine thigh infusion model. J Reconstr Microsurg 29:303–306
Tang B, Tait I, Ross G et al (2011) Development and use of a restructured animal tissue model for training in laparoscopic salpingostomy and salpingectomy. J Minim Invasive Gynecol 18:785–791
Cheung CL, Looi T, Lendvay TS et al (2014) Use of 3-dimensional printing technology and silicone modeling in surgical simulation: development and face validation in pediatric laparoscopic pyeloplasty. J Surg Educ 71:762–767
Zhang A, Hunerbein M, Dai Y et al (2008) Construct validity testing of a laparoscopic surgery simulator (Lap Mentor): evaluation of surgical skill with a virtual laparoscopic training simulator. Surg Endosc 22:1440–1444
McDougall EM, Corica FA, Boker JR et al (2006) Construct validity testing of a laparoscopic surgical simulator. J Am Coll Surg 202:779–787
Shanmugan S, Leblanc F, Senagore AJ et al (2014) Virtual reality simulator training for laparoscopic colectomy: what metrics have construct validity? Dis Colon Rectum 57:210–214
Sanchez-Peralta LF, Sanchez-Margallo FM, Moyano-Cuevas JL et al (2010) Construct and face validity of SINERGIA laparoscopic virtual reality simulator. Int J Comput Assist Radiol Surg 5:307–315
Acknowledgments
We thank all the volunteers involved in this study. We also thank Professor Liang Allen Ping from School of Foreign Studies of Southern Medical University for revising the manuscript.
Funding
This work was supported by National Natural Science Foundation of China (61190122, 61190123) and Science and Technology Research Program of Guangzhou and Guangdong ([2011]233-39, 2013B021800179).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Jujiao Xiao, Zhonglin Cui, Maoqing Fu, Xiangxue Kong, Lei Tang, Zhanglin Wang, Fuyu You, Qingfeng Du, and Jianyi Li have no conflicts of interest or financial ties to disclose.
Additional information
Jujiao Xiao and Zhonglin Cui have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xiao, J., Cui, Z., Fu, M. et al. An ex vivo liver training model continuously perfused to simulate bleeding for suture skills involved in laparoscopic liver resection: development and validity. Surg Endosc 30, 4553–4561 (2016). https://doi.org/10.1007/s00464-016-4792-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4792-2