Abstract
Aim
The aim of this study was to evaluate the issue of improvement of disadvantages of different type meshes.
Methods
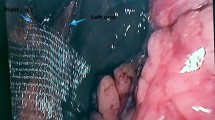
A retrospective analysis was performed on 101 gastroesophageal reflux disease patients who underwent reinforcement of crura with or without prosthetic mesh. Three types of mesh, 4-ply biologic small intestine submucosa (SIS, Surgisis®, since November 2010), 6-ply SIS (Biodesign™ Surgisis®, since March 2011), and composite synthetic mesh (Crurasoft®, since May 2010), were used. All patients were assigned to simple suture group (n = 35), 4-ply SIS group (n = 13), 6-ply Biodesign™ group (n = 26) or Crurasoft® group (n = 27). Postoperative follow-up was performed via clinical visit or phone call contact. Subjective assessment included dysphagia, patients’ symptomatic outcome judgment according to Visick and patients’ satisfaction. Objective evaluation included hiatal hernia recurrence according to upper endoscopy and barium contrast swallow. Follow-up was completed in 83 patients with a mean duration of 45 months (range 16–149 months).
Results
For the objective outcomes, although anatomic recurrence of hiatal hernia did not significantly differ between groups at 6 months postoperatively, long-term results showed a protective effect of mesh implantation on hernia recurrence (p = 0.047). For the subjective outcomes, the mesh group had a more significant improvement in Visick score (p = 0.020) compared to the simple suture group. Patient satisfaction was significantly higher in the mesh group (p = 0.014), and subgroup analysis showed a clear trend as follows: Crurasoft® ≈ Biodesign® > SIS®. A higher frequency of postoperative dysphagia was presented in the Crurasoft group compared with other two groups at 6 months postoperatively, but the difference was not significant over time (p = 0.227).
Conclusion
Mesh cruroplasty results in satisfactory symptom control with a low recurrence rate. 6-ply biologic mesh is promising with respect to the reduction in anatomic recurrences. Postoperative dysphagia does not occur commonly following mesh cruroplasty with PTFE/ePTFE mesh.
Similar content being viewed by others
References
Antoniou SA, Pointner R, Granderath FA (2011) Hiatal hernia repair with the use of biologic meshes: a literature review. Surg Laparosc Endosc Percutan Tech 21:1–9
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG, Demeester TR, Swanstrom LL, Daniel Smith C, Filipi CJ (2009) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23:1219–1226
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553–560 (discussion 560–561)
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R, Frantzides CT (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20:367–379
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP (2002) A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch Surg 137:649–652
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R (2005) Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 140:40–48
Trus TL, Bax T, Richardson WS, Branum GD, Mauren SJ, Swanstrom LL, Hunter JG (1997) Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg 1:221–228
Antoniou SA, Koch OO, Kaindlstorfer A, Asche KU, Berger J, Granderath FA, Pointner R (2012) Endoscopic full-thickness plication versus laparoscopic fundoplication: a prospective study on quality of life and symptom control. Surg Endosc 26:1063–1068
Desai KM, Diaz S, Dorward IG, Winslow ER, La Regina MC, Halpin V, Soper NJ (2006) Histologic results 1 year after bioprosthetic repair of paraesophageal hernia in a canine model. Surg Endosc 20:1693–1697
Badylak S, Kokini K, Tullius B, Whitson B (2001) Strength over time of a resorbable bioscaffold for body wall repair in a dog model. J Surg Res 99:282–287
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Wassenaar EB, Mier F, Sinan H, Petersen RP, Martin AV, Pellegrini CA, Oelschlager BK (2012) The safety of biologic mesh for laparoscopic repair of large, complicated hiatal hernia. Surg Endosc 26:1390–1396
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468
Oelschlager BK, Barreca M, Chang L, Pellegrini CA (2003) The use of small intestine submucosa in the repair of paraesophageal hernias: initial observations of a new technique. Am J Surg 186:4–8
Frantzides CT, Carlson MA, Loizides S, Papafili A, Luu M, Roberts J, Zeni T, Frantzides A (2010) Hiatal hernia repair with mesh: a survey of SAGES members. Surg Endosc 24:1017–1024
Zhang W, Tang W, Shan CX, Liu S, Jiang ZG, Jiang DZ, Zheng XM, Qiu M (2013) Dual-sided composite mesh repair of hiatal hernia: our experience and a review of the Chinese literature. World J Gastroenterol 19:5528–5533
Genta RM, Spechler SJ, Kielhorn AF (2011) The Los Angeles and Savary–Miller systems for grading esophagitis: utilization and correlation with histology. Dis Esophagus 24:10–17
Granderath FA (2007) Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why, when, and how? Surg Endosc 21:2224–2225
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548
Chilintseva N, Brigand C, Meyer C, Rohr S (2012) Laparoscopic prosthetic hiatal reinforcement for large hiatal hernia repair. J Visc Surg 149:e215–e220
Carlson MA, Condon RE, Ludwig KA, Schulte WJ (1998) Management of intrathoracic stomach with polypropylene mesh prosthesis reinforced transabdominal hiatal hernia repair. J Am Coll Surg 187:227–230
Edelman DS (1995) Laparoscopic paraesophageal hernia repair with mesh. Surg Laparosc Endosc 5:32–37
Frantzides CT, Richards CG, Carlson MA (1999) Laparoscopic repair of large hiatal hernia with polytetrafluoroethylene. Surg Endosc 13:906–908
Paul MG, DeRosa RP, Petrucci PE, Palmer ML, Danovitch SH (1997) Laparoscopic tension free repair of large paraesophageal hernia. Surg Endosc 1:303–307
Müller-Stich BP, Linke GR, Borovicka J, Marra F, Warschkow R, Lange J, Mehrabi A, Köninger J, Gutt CN, Zerz A (2008) Laparoscopic mesh-augmented hiatoplasty as a treatment of gastroesophageal reflux disease and hiatal hernias-preliminary clinical and functional results of a prospective case series. Am J Surg 195:749–756
Granderath FA, Schweiger UM, Kamolz T, Pasiut M, Haas CF, Pointner R (2002) Laparoscopic antireflux surgery with routine mesh-hiatoplasty in the treatment of gastroesophageal reflux disease. J Gastrointest Surg 6:347–353
Basso N, De Leo A, Genco A, Rosato P, Rea S, Spaziani E, Primavera A (2000) 360° laparoscopic fundoplication with tension free hiatoplasty in the treatment of symptom gastroesophageal reflux disease. Surg Endosc 14:164–169
Granderath FA, Kamolz T, Schweiger UM, Pasiut M, Haas CF, Wykypiel H, Pointner R (2002) Surgical outcome and analysis of failure after 500 laparoscopic antireflux procedures. Surg Endosc 16:753–757
Tatum RP, Shalhub S, Pellegrini CA, Pellegrini CA (2008) Complications of PTFE mesh at the diaphragmatic hiatus. J Gastrointest Surg 12:953–957
Hui TT, David T, Spyrou M, Phillips EH (2001) Mesh crural repair of large paraesophageal hiatal hernias. Am Surg 67:987–991
Keidar A, Szold A (2003) Laparoscopic repair of paraesophageal hernia with selective use of mesh. Surg Laparosc Endosc Percutan Tech 13:149–154
Schauer PR, Ikramuddin S, McLaughlin RH, Graham TO, Slivka A, Lee KK, Schraut WH, Luketich JD (2005) Comparison of laparoscopic versus open repair of paraesophageal hernia. Am J Surg 18:166–169
Lee E, Frisella MM, Matthews BD, Brunt LM (2007) Evaluation of acellular human dermis reinforcement of the crural closure in patients with difficult hiatal hernias. Surg Endosc 21:641–645
Zilberstein B, Eshkenazy R, Pajecki D, Granja C, Brito AC (2005) Laparoscopic mesh repair antireflux surgery for treatment of large hiatal hernia. Dis Esophagus 18:166–169
Willekes CL, Edoga JK, Frezza EE (1997) Laparoscopic repair of paraesophageal hernia. Ann Surg 225:31–38
Kohn GP, Price RR, DeMeester SR, Zehetner J, Muensterer OJ, Awad Z, Mittal SK, Richardson WS, Stefanidis D, Fanelli RD, Guidelines Committee SAGES (2013) Guidelines for the management of hiatal hernia. Surg Endosc 27:4409–4428
Pointer R, Granderath FA (2008) Laparoscopic fundoplication: when, how, and what to do it when it fails? Eur Surg 40:261–269
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10, 735 reported cases. J Am Coll Surg 193:428–439
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468
Abraham GA, Murray J, Billiar K, Sullivan SJ (2000) Evaluation of the porcine intestinal collagen layer as a biomaterial. J Biomed Mater Res 51:442
Gloeckner DC, Sacks MS, Billiar KL, Bachrach N (2000) Mechanical evaluation and design of a multilayered collagenous repair biomaterial. J Biomed Mater Res 52:365
Korolija D, Sauerland S, Wood-Dauphinee S, Abbou CC, Eypasch E (2004) Evaluation of quality of life after laparoscopic surgery. Surg Endosc 18:879–897
Korolija D, Wood-Dauphinee S, Pointner R (2007) Patient-reported outcomes: how important are they? Surg Endosc 21:503–507
Acknowledgments
We gratefully thank Xin Song for data collection and Nian-cun Qiu for his help in the follow-up period.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Bin Wang, Wei Zhang, Cheng-xiang Shan, Sheng Liu, Zhi-guo Jiang, and Ming Qiu have no conflicts of interest or financial ties to disclose.
Additional information
Bin Wang and Wei Zhang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, B., Zhang, W., Shan, Cx. et al. Long-term outcomes of cruroplasty reinforcement with composite versus biologic mesh for gastroesophageal reflux disease. Surg Endosc 30, 2865–2872 (2016). https://doi.org/10.1007/s00464-015-4570-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4570-6