Background
Conventional laparoscopic fundoplications (CLF) have been the gold standard for Nissen fundoplications (NFs) for two decades. The advent of a robotic approach for fundoplication procedures creates a potential alternative. Thus, we used a national database to examine perioperative outcomes with respect to open, laparoscopic, and robotic approaches.
Methods
The University Health System Consortium is an alliance of medical centers, numbering over 115 academic institutions and their 271 affiliated hospitals. We used International Classification of Diseases codes to elicit patients over the age of 18 years who received NF procedures.
Results
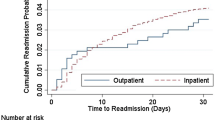
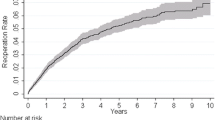
A total of 12,079 patients of similar demographic background received fundoplication procedures from October 2008 to June 2012. Of those, 2,168 were open fundoplications (OF), 9,572 were CLF, and 339 were robot-assisted laparoscopic fundoplications (RLF). CLF and RLF displayed no significance in mortality (0.1 vs. 0 %; p = 0.5489), morbidity (4.0 vs. 5.6 %; p = 0.1744), length of stay (2.8 ± 3.6 vs. 3.0 ± 3.5; p = 0.3242), and intensive care unit (ICU) cases (8.4 vs. 11.5 %; p = 0.051). However, CLF remained superior, with a lower 30-day re-admission rate (1.8 vs. 3.6 %; p < 0.05) and cost (US$7,968 ± 6,969 vs. US$10,644 ± 6,041; p < 0.05). When RLF was compared with OF, RLF had significantly improved morbidity (5.6 vs. 11 %; p < 0.05), length of stay (6.1 ± 7.2 vs. 3.0 ± 3.5 days; p < 0.05), less ICU admission (11.5 vs. 23.1 %; p <0.05) and less cost (US$10,644 ± 6,041 vs. US$12,766 ± 13,982; p < 0.05).
Conclusions
Current data suggests that robot-assisted NF procedures have similar patient outcomes to conventional laparoscopic NF, with the exception of added cost and higher re-admission rate. While the higher costs are expected given the new technology, increasing re-admission rates are concerning and may represent the level of experience of the surgeon as well as the robotic learning curve.
Similar content being viewed by others
References
Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R (1991) Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc 1:138–143
Eshraghi N, Farahmand M, Soot SJ, Rand-Luby L, Deveney CW, Sheppard BC (1998) Comparison of outcomes of open versus laparoscopic Nissen fundoplication performed in a single practice. Am J Surg 175:371–374
Hinder RA, Filipi CJ, Wetscher G, Neary P, DeMeester TR, Perdikis G (1994) Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg 220:472–481
Laine S, Rantala A, Gullichsen R, Ovaska J (1997) Laparoscopic vs conventional Nissen fundoplication: a prospective randomized study. Surg Endosc 11:441–444
Landreneau RJ, Wichmann RJ, Hazelrigg SR, Santucci TS, Boley TM, Magee MJ, Naunheim KS (1998) Success of laparoscopic fundoplication for gastroesophageal reflux disease. Ann Thorac Surg 66:1886–1983
Peters JH, DeMeester TR, Crookes P, Oberg S, de Vos Shoop M, Hagan JA, Bremner CG (1998) The treatment of gastroesophageal reflux disease with laparoscopic Nissen fundoplication: prospective evaluation of 100 patients with “typical” symptoms. Ann Surg 228:40–50
Watson DI, Jamieson GG (1999) Antireflux surgery in the laparoscopic era. Br J Surg 85:1173–1184
Niebisch S, Fleming FJ, Galey KM, Wilshire CL, Jones CE, Litle VR, Watson TJ, Peters JH (2012) Perioperative risk of laparoscopic fundoplication: safer than previously reported. Analysis of the American College of Surgeons National Surgical Quality Improvement Program 2005–2009. J Am Coll Surg 215(1):61–68
Jun M, Yingxin K, Xiao C, Wang B, Wang Z (2010) Whether robot-assisted laparoscopic fundoplication is better for gastroesophageal reflux disease in adults: a systematic review and meta-analysis. Surg Endosc 24:1803–1814
Muller-Stich BP, Reiter MA, Wente MN, Bintintan VV, Koninger J, Buchler MW, Gutt CN (2007) Robot-assisted versus conventional laparoscopic fundoplication: short-term outcome of a pilot randomized controlled trial. Surg Endosc 21:1800–1805
Nguyen NT, Hinojosa M, Fayad C, Varela E, Wilson SE (2007) Use and outcomes of laparoscopic versus open gastric bypass at academic medical centers. J Am Coll Surg 205:248–255
Hinojosa MW, Murrell ZA, Konyalian VR, Mills S, Nguyen NT, Stamos MJ (2007) Comparison of laparoscopic vs. open sigmoid colectomy for benign and malignant disease at academic medical centers. J Gastrointest Surg 11:1423–1429 (discussion 1429–1430)
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27
Ballantyne GH (2002) Robotic surgery, telerobotic surgery, telepresence, and telementoring: review of early clinical results. Surg Endosc 16:1389–1402
Shaligram A, Unnirevi J, Simorov A, Kothari VM, Oleynikov D (2012) How does the robot affect outcomes? A retrospective review of open, laparoscopic, and robotic Heller myotomy for achalasia. Surg Endosc 26:1047–1050
Disclosures
Benjamin Owen, Anton Simorov, Andy Siref, and Valerie Shostrom have nothing to disclose. Dmitry Oleynikov is a founder and board member of Virtual Incision Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Owen, B., Simorov, A., Siref, A. et al. How does robotic anti-reflux surgery compare with traditional open and laparoscopic techniques: a cost and outcomes analysis . Surg Endosc 28, 1686–1690 (2014). https://doi.org/10.1007/s00464-013-3372-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3372-y