Abstract
Introduction
Current literature on redo antireflux surgery has limitations due to small sample size or single center experiences. This study aims to evaluate the reoperation rate of laparoscopic fundoplication in a large population database.
Methods
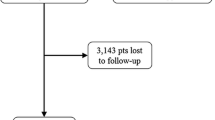
A longitudinal version of the California Office of Statewide Health Planning and Development database from 1995 to 2010 was used. Inclusion criteria were patients who received a laparoscopic fundoplication for uncomplicated gastroesophageal reflux disease (GERD) or hiatal hernia. Patients were excluded if they had complications of GERD, esophageal or gastric cancer, prior esophageal or gastric surgery, vagotomy, esophageal dysmotility, and diaphragmatic hernia with gangrene or obstruction. The outcome was reoperation, specified as another fundoplication or reversal. Analysis was carried out via a Kaplan–Meier plot, hazard curve, and multivariate analysis adjusting for age, race, gender, comorbidities, insurance status, hospital teaching status, and year of procedure.
Results
13,050 patients were included in the study. The 5 and 10-year cumulative reoperation rates were 5.2 % (95 % CI 4.8–5.7%) and 6.9 % (95 % CI 6.1–7.9%), respectively. Of these reoperations, 30 % were performed at a different hospital from that of the initial fundoplication. Reoperation rate was highest at 1 year post-operatively (1.7 % per year), and steadily declined until 4 years post-operatively, after which it remained at approximately 0.5 % per year. Multivariate analysis demonstrated significantly higher rates of reoperation among younger patients (HR = 3.56 for <30yo; HR = 1.89 for 30–50yo; HR = 1.65 for 50–65yo) and female patients (HR = 1.35).
Conclusions
Nearly one third of reoperations after failed laparoscopic fundoplication occur at a hospital different from the initial operation, which raises concern that existing literature does not reflect the true reoperation rate. The reoperation rate is highest in the first year postoperatively. The reasons for the higher rate of reoperation in females and younger patients remain unclear and warrant further study


Similar content being viewed by others
References
Nissen R (1956) A simple operation for control of reflux esophagitis. Schweiz Med Wochenschr 86:590–592
Kahrilas PJ, Shaheen NJ, Vaezi MF et al (2008) American Gastroenterological Association medical position statement on the management of gastroesophageal reflux disease. Gastroenterology 135:1383–1391
Peters JH, DeMeester TR (1996) Indications, benefits and outcome of laparoscopic Nissen fundoplication. Dig Dis 14(3):169–179
Salminen P (2009) The laparoscopic Nissen fundoplication—a better operation? Surgeon. 7(4):224–227
DeMeester TR et al (1986) Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg 204(1):19–20
Grande L et al (1994) Value of Nissen fundoplication in patients with gastroesophageal reflux judged by long-term symptom control. Br J Surg 81(4):548–550
Booth et al (2002) Results of laparoscopic Nissen fundoplication at 2–8 years after surgery. Br J Surg 89(4):476–481
Anvari M, Allen C (2003) Five-year comprehensive outcomes evaluation in 181 patients after laparoscopic Nissen fundoplication. J Am Coll Surg 196(1):51–57
Stein HJ et al (1996) Failure of antireflux surgery: causes and management strategies. Am J Surg 171(1):36–39
Dallemagne B et al (2011) Long-term results after laparoscopic reoperation for failed antireflux procedures. The British Journal of Surgery. 98(11):1581–1587
Horgan et al (1999) Failed antireflux surgery: what have we learned from reoperations? Arch Surg 134(8):809–815
Hatch K et al (2004) Failed fundoplications. Am J Surg 188(6):786–791
Lafullarde T et al (2001) Laparoscopic Nissen Fundoplication: five-year results and beyond. Arch Surg 136(2):180–184
Byrne JP et al (2005) Symptomatic and functional outcome after laparoscopic reoperation for failed antireflux surgery. Br J Surg 92(8):996–1001
Luostarinen ME et al (1993) Refundoplication for recurrent gastroesophageal reflux. World J Surg 17(5):587–593
Dutta et al (2004) Outcome of laparoscopic redo fundoplication. Surg Endosc 18(3):440–443
Mariette C et al (2011) Ambulatory laparoscopic fundoplication for gastroesophageal reflux disease: a systematic review. Surg Endosc 25(9):2859–2864
Funch-Jensen P et al (2008) Complications and frequency of redo antireflux surgery in Denmark: a nationwide study, 1997–2005. Surg Endosc 22(3):627–630
Disclosures
Tianzan Zhou, Cristina Harnsberger, Ryan Broderick, Hans Fuchs, Mark Talamini, Garth Jacobsen, Santiago Horgan, David Chang, and Bryan Sandler have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, T., Harnsberger, C., Broderick, R. et al. Reoperation rates after laparoscopic fundoplication. Surg Endosc 29, 510–514 (2015). https://doi.org/10.1007/s00464-014-3660-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3660-1