Abstract
Background
There is increasing interest in using simulators for laparoscopic surgery training, and simulators have rapidly become an integral part of surgical education.
Methods
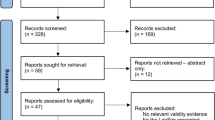
We searched MEDLINE, EMBASE, Cochrane Library, and Google Scholar for randomized controlled studies that compared the use of different types of simulators. The inclusion criteria were peer-reviewed published randomized clinical trials that compared simulators versus standard apprenticeship surgical training of surgical trainees with little or no prior laparoscopic experience. Of the 551 relevant studies found, 17 trials fulfilled all inclusion criteria. The effect sizes (ES) with 95 % confidence intervals [CI] were calculated for multiple psychometric skill outcome measures.
Results
Data were combined by means of both fixed- and random-effects models. Meta-analytic combined effect size estimates showed that novice students who trained on simulators were superior in their performance and skill scores (d = 1.98, 95 % CI: 1.20–2.77; P < 0.01), were more careful in handling various body tissue (d = 1.08, 95 % CI: 0.36–1.80; P < 0.01), and had a higher accuracy score in conducting laparoscopic tasks (d = 1.38, 95 % CI: 0.30–2.47; P < 0.05).
Conclusion
Simulators have been shown to provide better laparoscopic surgery skills training for trainees than the traditional standard apprenticeship approach to skill development. Surgical residency programs are highly encouraged to adopt the use of simulators in teaching laparoscopic surgery skills to novice students.

Similar content being viewed by others
References
Ostergaard D (2004) National Medical Simulation training program in Denmark. Crit Care Med 32(2 Suppl):S58–S60
Berkenstadt H et al (2006) Incorporating simulation-based objective structured clinical examination into the Israeli National Board Examination in Anesthesiology. Anesth Analg 102(3):853–858
Satava RM (2001) Surgical education and surgical simulation. World J Surg 25(11):1484–1489
Mann DD, Eland DC (2005) Self-efficacy in mastery learning to apply a therapeutic psychomotor skill. Percept Mot Skills 100(1):77–84
American College of Surgeons (2008) Advanced Trauma Life Support (ATLS) course coordinator and director manual, 8th edn. American College of Surgeons, Chicago
Gaba DM (2004) The future vision of simulation in health care. Qual Saf Health Care 13(Suppl 1):i2–i10
Satava RM (2008) Historical review of surgical simulation—a personal perspective. World J Surg 32(2):141–148
Holzman RS et al (1995) Anesthesia crisis resource management: real-life simulation training in operating room crises. J Clin Anesth 7(8):675–687
Chopra V et al (1994) The Leiden anaesthesia simulator. Br J Anaesth 73(3):287–292
Rosen KR (2008) The history of medical simulation. J Crit Care 23(2):157–166
Ganai S et al (2007) Virtual-reality training improves angled telescope skills in novice laparoscopists. Am J Surg 193(2):260–265
Madan AK, Frantzides CT (2007) Prospective randomized controlled trial of laparoscopic trainers for basic laparoscopic skills acquisition. Surg Endosc 21(2):209–213
Torkington J et al (2001) Skill transfer from virtual reality to a real laparoscopic task. Surg Endosc 15(10):1076–1079
Devitt JH et al (1997) Testing the raters: inter-rater reliability of standardized anaesthesia simulator performance. Can J Anaesth 44(9):924–928
Devitt JH et al (1998) Testing internal consistency and construct validity during evaluation of performance in a patient simulator. Anesth Analg 86(6):1160–1164
Botden SM et al (2008) Face validity study of the ProMIS augmented reality laparoscopic suturing simulator. Surg Technol Int 17:26–32
Zhang A et al (2008) Construct validity testing of a laparoscopic surgery simulator (LapMentor): evaluation of surgical skill with a virtual laparoscopic training simulator. Surg Endosc 22(6):1440–1444
Sankaranarayanan G et al (2011) Validation of a novel laparoscopic adjustable gastric band simulator. Surg Endosc 25(4):1012–1018
Duffy AJ et al (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19(3):401–405
Maran NJ, Glavin RJ (2003) Low- to high-fidelity simulation - a continuum of medical education? Med Educ 37(Suppl 1):22–28
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. L. Erlbaum Associates, Hillsdale, xxi, 567 pp
Hogle NJ et al (2009) Validation of laparoscopic surgical skills training outside the operating room: a long road. Surg Endosc 23(7):1476–1482
Aggarwal R et al (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246(5):771–779
Grantcharov TP et al (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91(2):146–150
Clevin L, Grantcharov TP (2008) Does box model training improve surgical dexterity and economy of movement during virtual reality laparoscopy? A randomised trial. Acta Obstet Gynecol Scand 87(1):99–103
Banks EH et al (2007) Does a surgical simulator improve resident operative performance of laparoscopic tubal ligation? Am J Obstet Gynecol 197(5):541.e1-5
Ahlberg G et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193(6):797–804
Andreatta PB et al (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243(6):854–860 discussion 860-863
Seymour NE et al (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236(4):458–463 discussion 463-464
Scott DJ et al (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191(3):272–283
Lucas S et al (2008) Virtual reality training improves simulated laparoscopic surgery performance in laparoscopy naive medical students. J Endourol 22(5):1047–1051
Jordan JA et al (2001) Virtual reality training leads to faster adaptation to the novel psychomotor restrictions encountered by laparoscopic surgeons. Surg Endosc 15(10):1080–1084
Ahlberg G et al (2002) Does training in a virtual reality simulator improve surgical performance? Surg Endosc 16(1):126–129
Hyltander A et al (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16(9):1324–1328
Korndorffer JR Jr et al (2005) Development and transferability of a cost-effective laparoscopic camera navigation simulator. Surg Endosc 19(2):161–167
Sroka G et al (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199(1):115–120
Botden SM, Jakimowicz JJ (2009) What is going on in augmented reality simulation in laparoscopic surgery? Surg Endosc 23(8):1693–1700
Fried GM et al (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240(3):518–525 discussion 525-528
Lamata P et al (2006) Conceptual framework for laparoscopic VR simulators. IEEE Comput Graph Appl 26(6):69–79
Szekely G et al (1999) Virtual reality based surgery simulation for endoscopic gynaecology. Stud Health Technol Inform 62:351–357
Cao CG et al (2007) Can surgeons think and operate with haptics at the same time? J Gastrointest Surg 11(11):1564–1569
Lamata P et al (2006) Study of laparoscopic forces perception for defining simulation fidelity. Stud Health Technol Inform 119:288–292
Disclosures
Drs. Azzam Al-Kadi, Tyrone Donnon, Elizabeth Oddone Paolucci, Philip Mitchell, Estifanos Debru, and Neal Church have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Kadi, A.S., Donnon, T., Oddone Paolucci, E. et al. The effect of simulation in improving students’ performance in laparoscopic surgery: a meta-analysis. Surg Endosc 26, 3215–3224 (2012). https://doi.org/10.1007/s00464-012-2327-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2327-z