Abstract
Background
Laparoscopic cholecystectomy is the standard treatment for symptomatic gallstones. The quality of the procedure frequently is included in quality improvement programs, but outcome values have not been described to define the standard of care for a general population. This study included 20,307 cholecystectomies from a national prospective database that combines administrative data with clinical data. This report states the quality of cholecystectomy in Denmark, establishes benchmarks, and identifies significant risk factors.
Methods
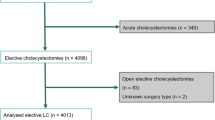
The Danish Cholecystectomy Database was queried for data from 2006 to 2009. The outcome measures included conversion rate, hospital length of stay (LOS), readmission, additional procedures, and 30-day mortality. Patient characteristics and operative findings were analyzed as risk factors using stepwise backward logistic regression.
Results
The study included 20,307 patients (82% of all cholecystectomies). The conversion rate was 7.6%. Male sex, acute cholecystitis, and previous upper abdominal surgery were risk factors for conversion, with respective odds ratios of 1.50, 4.61, and 3.54. The mean LOS was 1.5 days, and 37.3% of the patients had same-day surgery. The readmission rate was 9.6%. Nearly 70% had a LOS of 1 day or less and no readmission; 17.3% had a LOS longer than 3 days and/or readmission; 5.6% had an additional procedure within 30 days; and 0.2% had a bile duct injury requiring reconstructive surgery. The 30-day mortality rate was 0.27%. Age older than 60 years, American Society of Anesthesiology (ASA) score exceeding 1, and open procedure were significant risk factors for all the outcomes. Body mass index (BMI) was not a risk factor for any of the outcomes.
Conclusion
The quality of cholecystectomy is high in Denmark, with a low conversion rate and a high frequency of short admissions without readmission. Acute cholecystitis and open procedure are important risk factors for poorer outcomes.The results of this study analyzing a large, unbiased population can be used to benchmark outcomes of cholecystectomy.



Similar content being viewed by others
References
Jorgensen T (1989) Gallstones in a Danish population: relation to weight, physical activity, smoking, coffee consumption, and diabetes mellitus. Gut 30:528–534
NIH Consensus conference (1993) Gallstones and laparoscopic cholecystectomy. JAMA 269:1018–1024
McMahon AJ, Fischbacher CM, Frame SH, MacLeod MC (2000) Impact of laparoscopic cholecystectomy: a population-based study. Lancet 356:1632–1637
A prospective analysis of 1,518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med 324:1073–1078, 1991
Connor S, Garden OJ (2006) Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg 93:158–168
Harboe KM, Anthonsen K, Bardram L (2009) Validation of data and indicators in the Danish Cholecystectomy Database. Int J Qual Health Care 21:160–168
Mainz J (2003) Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 15:523–530
The Danish National Board of Health (2006) Referenceprogram for behandling af patienter med galdestenssygdomme (Guidelines for treatment of patients with gallstone disease). Retrieved 26 March at http://www.sst.dk/publ/PLAN/SfR/Galdesten/Galdestenssygdomme.pdf
Schmidt CO, Kohlmann T (2008) When to use the odds ratio or the relative risk? Int J Public Health 53:165–167
Bardram L (2008) The annual report of The Danish Cholecystectomy Database 2008. Retrieved 26 March 2010 at http://www.kliniskedatabaser.dk/artikeldataVis.asp?id=27&m
Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC (1993) Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg 165:9–14
Fletcher DR, Hobbs MS, Tan P, Valinsky LJ, Hockey RL, Pikora TJ, Knuiman MW, Sheiner HJ, Edis A (1999) Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg 229:449–457
Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L (2005) Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg 92:44–49
Ros A, Gustafsson L, Krook H, Nordgren CE, Thorell A, Wallin G, Nilsson E (2001) Laparoscopic cholecystectomy versus minilaparotomy cholecystectomy: a prospective, randomized, single-blind study. Ann Surg 234:741–749
Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10:1081–1091
Karayiannakis AJ, Polychronidis A, Perente S, Botaitis S, Simopoulos C (2004) Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc 18:97–101
Lipman JM, Claridge JA, Haridas M, Martin MD, Yao DC, Grimes KL, Malangoni MA (2007) Preoperative findings predict conversion from laparoscopic to open cholecystectomy. Surgery 142:556–565
Rosen M, Brody F, Ponsky J (2002) Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 184:254–258
Veen EJ, Bik M, Janssen-Heijnen ML, De JM, Roukema AJ (2008) Outcome measurement in laparoscopic cholecystectomy by using a prospective complication registry: results of an audit. Int J Qual Health Care 20:144–151
Velanovich V, Morton JM, McDonald M, Orlando R III, Maupin G, Traverso LW (2006) Analysis of the SAGES outcomes initiative cholecystectomy registry. Surg Endosc 20:43–50
Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G (2005) Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg 140:986–992
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188:205–211
Russell JC, Walsh SJ, Mattie AS, Lynch JT (1996) Bile duct injuries, 1989–1993: a statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg 131:382–388
Carbonell AM, Lincourt AE, Kercher KW, Matthews BD, Cobb WS, Sing RF, Heniford BT (2005) Do patient or hospital demographics predict cholecystectomy outcomes? A nationwide study of 93,578 patients. Surg Endosc 19:767–773
Ballal M, David G, Willmott S, Corless DJ, Deakin M, Slavin JP (2009) Conversion after laparoscopic cholecystectomy in England. Surg Endosc 23:2338–2344
Giger UF, Michel JM, Opitz I, Th ID, Kocher T, Krahenbuhl L (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg 203:723–728
Buanes T, Mjaland O, Waage A, Langeggen H, Holmboe J (1998) A population-based survey of biliary surgery in Norway: relationship between patient volume and quality of surgical treatment. Surg Endosc 12:852–855
Orlando R III, Russell JC, Lynch J, Mattie A (1993) Laparoscopic cholecystectomy: a statewide experience. The Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg 128:494–498
Thesbjerg S, Harboe KM, Bardram L, Rosenberg J (2010) Sex differences in laparoscopic cholecystectomy. Surg Endosc 24:3068–3072
Kama NA, Doganay M, Dolapci M, Reis E, Atli M, Kologlu M (2001) Risk factors resulting in conversion of laparoscopic cholecystectomy to open surgery. Surg Endosc 15:965–968
Birkmeyer JD, Hamby LS, Birkmeyer CM, Decker MV, Karon NM, Dow RW (2001) Is unplanned return to the operating room a useful quality indicator in general surgery? Arch Surg 136:405–411
Froschl U, Sengstbratl M, Huber J, Fugger R (2006) Unplanned reoperations for infection complications: a survey for quality control. Surg Infect Larchmt 7:263–268
Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG (2001) Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg 234:549–558
Waage A, Nilsson M (2006) Iatrogenic bile duct injury: a population-based study of 152 776 cholecystectomies in the Swedish Inpatient Registry. Arch Surg 141:1207–1213
Mahatharadol V (2004) Bile duct injuries during laparoscopic cholecystectomy: an audit of 1,522 cases. Hepatogastroenterology 51:12–14
Acknowledgments
The authors appreciate the indispensable help of data manager Susie Lendal Antvorskov from the Quality Unit of The Capital Region of Denmark.
Disclosures
Kirstine M. Harboe and Linda Bardram have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harboe, K.M., Bardram, L. The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc 25, 1630–1641 (2011). https://doi.org/10.1007/s00464-010-1453-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1453-8