Abstract
Background
Conversion from laparoscopic to open cholecystectomy may not be desirable due to the increased complication rate and prolonged convalescence. In Denmark, nationwide data show that 7.7% of the laparoscopic cholecystectomies are converted to open surgery. This article aims to document the relationship of gender to conversion rate and length of hospital stay after laparoscopic cholecystectomy in a national cohort of patients.
Methods
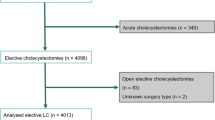
The gender of 5,951 patients from the 2007 National Danish Cholecystectomy Database was compared with conversion rate, length of hospital stay, and various risk factors using multivariate analyses.
Results
The findings showed that 14.3% of the patients had acute cholecystitis and that men had the highest risk (odds ratio [OR], 1.94; 95% confidence interval [CI], 1.66–2.27). The operative findings for the men included sequelae from previous acute cholecystitis more frequently than the findings for the women (OR, 1.89; 95% CI, 1.67–2.15). The rate for conversion from laparoscopic to open surgery was 7.7%, and male sex was highly associated with conversion (OR, 2.48; 95% CI, 2.04–3.01). Thus, 259 (5.8%) of the 4,451 operations for women were converted to laparotomy compared with 199 (13.3%) of the 1,500 operations for men. No significant sex differences were found in the proportion of bile duct lesions (those requiring reconstructive surgery as well as those that could be handled by endoscopy or T-tube drainage, suturing, or both) or in the 30-day mortality rate. The multivariate analyses showed that male sex was a significant factor for conversion but not for length of postoperative stay or readmission.
Conclusion
Men showed a significantly higher risk of the operation being converted from laparoscopic to open cholecystectomy than women (OR, 2.48; 95% CI, 2.04–3.01). The main reason for this may be that men more frequently had acute cholecystitis or sequelae from previous acute cholecystitis. These results can be used to give patients a better basis for their informed consent and better resource management in connection with the operation.
Similar content being viewed by others
References
Ainsworth A, Adamsen S, Rosenberg J (2005) Kolecystektomi i Danmark 1989–2003. Ugeskr Læger 167:2648–2650
Keus F, de Jong JAF, Gooszen HG, van Laarhoven CJHM (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev CD006231
Dansk Galde Database Årsrapport 2006 (2007). Retrieved November 2008 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Giger UF, Michel JM, Opitz I, Inderbitzin DT, Kocher T, Krähenbühl L (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy. J Am Coll Surg 203:723–728
Wolf AS, Nijsse BA, Sokal SM (2009) Surgical outcomes of open cholecystectomy in the laparoscopic era. Am J Surg 197:781–784
Bardram L, Rosenberg J, Kristiansen V (2005) Dansk galde database–DGD. Ugeskr Læger 167:2618–2620
Harboe KM, Anthonsen K, Bardram L (2009) Validation of data and indicators in the Danish Cholecystectomy Database. Int J Qual Health Care 21:160–168
Galde Database Kliniske indikatorer. Retrieved November 2008 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Dansk Galde Database Årsrapport 2007 (2008). Retrieved July 2009 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Botaitis S, Polychronidis A, Pitiakoudis M, Perente S, Simopoulos C (2008) Does gender affect laparoscopic cholecystectomy? Surg Laparosc Endosc Percutan Tech 18:157–161
Russell JC, Walsh SJ, Reed-Fourquet L, Mattie A, Lynch J (1998) Symptomatic cholelithiasis: a different disease in men? Ann Surg 227:195–200
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188:205–211
Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M (2001) A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg 181:520–525
Zisman A, Gold-Deutch R, Zisman E, Negri M, Halpern Z, Lin G, Halevy A (1996) Is male gender a risk factor for conversion of laparoscopic into open cholecystectomy? Surg Endosc 10:892–894
Lipman JM, Claridge JA, Haridas M, Martin MD, Yao DC, Grimes KL, Malangoni MA (2007) Preoperative findings predict conversion from laparoscopic to open cholecystectomy. Surgery 142:556–563
Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH (2006) Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg 30:1698–1704
Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10:1081–1091
Lee HK, Han HS, Min SK, Lee JH (2005) Sex-based analysis of the outcome of laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 92:463–466
Gharaibeh KIA, Qasaimeh GR, Al-Heiss H, Ammari F, Bani-Hani K, Al-Jaberi TM, Al-Natour S (2002) Effect of timing of surgery, tape of inflammation, and sex on outcome of laparoscopic cholecystectomy for acute cholecystitis. J Laparoendosc Adv Surg Tech A 12:193–198
Rosen M, Brody F, Ponsky J (2002) Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 184:254–258
Bingener-Casey J, Richards ML, Strodel WE, Schwesinger WH, Sirinek KR (2002) Reasons for conversion from laparoscopic to open cholecystectomy: a 10-year review. J Gastrointest Surg 6:800–805
Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ (2005) Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc 19:905–909
Bickel A, Rappaport A, Kanievski V, Vaksman I, Haj M, Geron N, Eitan A (1996) Laparoscopic management of acute cholecystitis: prognostic factors for success. Surg Endosc 10:1045–1049
Teixeira JPA, Saraiva AC, Cabral AC, Barros H, Reis JR, Teixeira A (2000) Conversion factors in laparoscopic cholecystectomy for acute cholecystitis. Hepatogastroenterology 47:626–630
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystetomy to open surgery. JSLS 10:359–363
Disclosures
Simon E. Thesbjerg, Kirstine M. Harboe, Linda Bardram, and Jacob Rosenberg have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thesbjerg, S.E., Harboe, K.M., Bardram, L. et al. Sex differences in laparoscopic cholecystectomy. Surg Endosc 24, 3068–3072 (2010). https://doi.org/10.1007/s00464-010-1091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1091-1