Abstract
Background
Laparoscopic resection for colorectal cancer is increasingly being performed worldwide. Although learning standardized procedures under the supervision of an experienced surgeon may be effective, there is currently no information on the learning curve under such circumstances. This single-center study aimed to evaluate the learning curve for laparoscopic resection for colorectal cancer of one surgical fellow with no previous experience with laparoscopic colectomy.
Methods
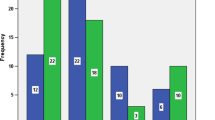
Data were analyzed for 108 consecutive patients who underwent laparoscopic resection for colorectal cancer between July 2007 and October 2009. Surgery was performed by a single fellow with no prior experience with laparoscopic colorectal resection. The learning effect was evaluated by dividing the patients into two groups: group 1 consisted of the first 50 patients and group 2 included the last 58 patients. Short-term outcomes were compared between groups.
Results
More complex procedures were performed more frequently in group 2 than in group 1 (p = 0.0086). A significantly greater percentage of cases was completed by the trainee in group 2 than in group 1 (91% vs. 68%; p = 0.0030) and were performed independent of the supervisor (81% vs. 38%; p < 0.0001). All procedures after the 65th case were completed by the trainee. Mean number of lymph nodes harvested (15 vs. 16), conversion to open surgery (0% vs. 2%), and postoperative complications (4% vs. 12%) did not differ significantly between groups. There were no intraoperative complications or mortality. Operating time for sigmoidectomy/high anterior resection reached a steady state after 35 cases.
Conclusions
The present study shows that training in laparoscopic surgery for colorectal cancer under the supervision of an experienced surgeon can be performed safely without jeopardizing the short-term outcomes. More complex procedures were performed successfully by the trainee during the later period, even though he was more independent of the supervisor.


Similar content being viewed by others
References
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246:655–662; discussion 662–664
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44:217–222
Wishner JD, Baker JW Jr, Hoffman GC, Hubbard GW 2nd, Gould RJ, Wohlgemuth SD, Ruffin WK, Melick CF (1995) Laparoscopic-assisted colectomy. The learning curve. Surg Endosc 9:1179–1183
Agachan F, Joo JS, Sher M, Weiss EG, Nogueras JJ, Wexner SD (1997) Laparoscopic colorectal surgery. Do we get faster? Surg Endosc 11:331–335
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum 46:1371–1378; discussion 1378–1379
Champagne BJ, Lee EC, Valerian B, Armstrong D, Ambroze W, Orangio G (2008) A novel end point to assess a resident’s ability to perform hand-assisted versus straight laparoscopy for left colectomy: is there really a difference? J Am Coll Surg 207:554–559
Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Yamaguchi T, Muto T (2008) Standardized technique of laparoscopic intracorporeal rectal transection and anastomosis for low anterior resection. Surg Endosc 22:557–561
Kuroyanagi H, Akiyoshi T, Oya M, Fujimoto Y, Ueno M, Yamaguchi T, Muto T (2009) Laparoscopic-assisted anterior resection with double-stapling technique anastomosis: safe and feasible for lower rectal cancer? Surg Endosc 23:2197–2202
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T (2009) Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 146:483–489
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Yamaguchi T, Muto T (2009) Safety of laparoscopic total mesorectal excision for low rectal cancer with preoperative chemoradiation therapy. J Gastrointest Surg 13:521–525
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2009) Multidimensional analysis of the learning curve for laparoscopic resection in rectal cancer. J Gastrointest Surg 13:275–281
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23:622–628
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Chen W, Sailhamer E, Berger DL, Rattner DW (2007) Operative time is a poor surrogate for the learning curve in laparoscopic colorectal surgery. Surg Endosc 21:238–243
Disclosures
Drs. Akiyoshi, Kuroyanagi, Ueno, Oya, Fujimoto, Konishi, and Yamaguchi have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akiyoshi, T., Kuroyanagi, H., Ueno, M. et al. Learning curve for standardized laparoscopic surgery for colorectal cancer under supervision: a single-center experience. Surg Endosc 25, 1409–1414 (2011). https://doi.org/10.1007/s00464-010-1404-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1404-4