Abstract
Background
Robotic laparoscopic surgery has been shown to decrease task completion time, reduce errors, and decrease training time, as compared with manual laparoscopic surgery. However, current literature has not addressed the physiologic effects, in particular muscle responses, to training with a robotic surgical system. The authors seek to determine the frequency response of electromyographic (EMG) signals of specific arm and hand muscles with training using the da Vinci Surgical System.
Methods
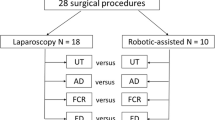
Seven right-handed medical students were trained in three tasks with the da Vinci Surgical System over 4 weeks. These subjects, along with eight control subjects, were tested before and after training. Electromyographic (EMG) signals were collected from four arm and hand muscles during the testing sessions, and the median EMG frequency and bandwidth were computed.
Results
The median frequency and frequency bandwidth both were increased after training for two of the three tasks.
Conclusion
The results suggest that training reduces muscle fatigue as a result of faster and more deliberate movements. These changes occurred predominantly in muscles that were the dominant muscles for each task, whereas the more demanding task recruited more diverse motor units. An evaluation of the physiologic demands of robotic laparoscopic surgery using electromyography can provide us with a meaningful quantitative way to examine performance and skill acquisition.





Similar content being viewed by others
References
Basmajian JV, De Luca CJ (1985) Muscles alive, their functions revealed by electromyography. Williams & Wilkins, Baltimore, MD
Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J (1997) A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc 11:139–142
Berguer R, Smith WD, Chung YH (2001) Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc 15: 1204–1207
Bonato P, Roy SH, Knaflitz M, Luca CJD (2001) Time-frequency parameters of the surface myoelectric signal for assessing muscle fatigue during cyclic dynamic contractions. IEEE Trans Biomed Eng 48: 745–753
Chang L, Satava RM, Pellegrini CA, Sinanan MN (2003) Robotic surgery: identifying the learning curve through objective measurment of skill. Surg Endosc 17: 1744–1748
D’Annibale AMD, Fiscon VMD, Trevisan PMD, Pozzobon MMD, Gianfreda VMD, Sovernigo GMD, Morpurgo EMD, Orsini CMD, Del Monte DMD (2004) The da Vinci robot in right adrenalectomy: considerations on technique. Surg Laparosc Endosc Percutan Tech 14: 38–41
De Ugarte DA, Etzioni DA, Gracia C, Atkinson JB (2003) Robotic surgery an resident training. Surg Endosc 17: 960–963
Farina D, Fosci M, Merletti R (2002) Motor unit recruitment strategies investigated by surface EMG variables. J Appl Physiol 92: 235–247
Farina D, Merletti R, Enoka RM (2004) The extraction of neural strategies from the surface EMG. J Appl Physiol 96: 1486–1495
Gutt CN, Oniu T, Schemmer P, Mehrabi A, Buchler MW (2004) Fewer adhesions induced by laparoscopic surgery? Surg Endosc 18: 898–906
Hashizume M, Shimada M, Tomikawa M, Ikeda Y, Takahashi I, Abe R, Koga F, Gotoh N, Konish K, Maehara S, Sugimachi K (2002) Early experiences of endoscopic procedures in general surgery assisted by a computer-enhanced surgical system. Surg Endosc 16: 1187–1191
Hernandez JD, Bann SD, Munz Y, Moorthy K, Datta V, Martin S, Dosis A, Bello F, Darzi A, Rockall T (2004) Qualitative and quantitative analysis of the learning curve of a simulated surgical task on the da Vinci system. J Gastrointest Surg 18: 372–378
Hubens G, Coveliers H, Balliu L, Ruppert M, Vaneerdeweg W (2003) A performance study comparing manual and robotic-assisted laparoscopic surgery using the da Vinci system. Surg Endosc 17: 1595–1599
Korolija D, Sauerland S, Wood-Dauphinee S, Abbou CC, Eypasch E, Garcia Caballero M, Lumsden MA, Millat B, Monson JRT, Nilsson G, Pointner R, Schwenk W, Shamiyeh A, Szold A, Targarona E, Ure B, Neugebauer E (2004) Evaluation of quality of life after laparoscopic surgery. Surg Endosc 18: 879–897
McClure N, Gallagher AG, McGuigan J, Ritchie K, Sheehy NP (1997) An ergonomic analysis of the fulcrum effect in endoscopic skill acquisition. Gynaecol Endosc 6: 90
Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A (2004) Dexterity enhancement with robotic surgery. Surg Endosc 18: 790–795
Munz Y, Moorthy K, Dosis A, Hernandez J, Bann SD, Bello F, Martin S, Darzi A, Rockall T (2004) The benefits of stereoscopic vision in robotic-assisted performance on bench models. Surg Endosc 18: 611–616
Narazaki K, Oleynikov D, Stergiou N (in review) Robotic laparoscopy: objective assessment of proficiency with bimanual inanimate tasks. J Laparoendosc Adv Surg Tech A
Narazaki K, Oleynikov D, Stergiou N (2006) Robotic surgery training and performance: identifying objective variables for quantifying the extent of proficiency. Surg Endosc 20: 96–103
Prasad SM, Maniar HS, Soper NJ, Damiano RJ, Klingensmith ME (2002) The effect of robotic assistance on learning curves for basic laparoscopic skills. Am J Surg 183: 702–707
Quick NE, Gillete JC, Shapiro R, Adrales GL, Gerlach D, Park AE (2003) The effect of using laparoscopic instruments on muscle activation patterns during minimally invasive surgery. Surg Endosc 17: 462–465
Sarle R, Tewari A, Shrivastava A, Peabody J, Menon M (2004) Surgical robotics and laparoscopic training drills. J Endourol 18: 63–67
Talamini MA, Stanfield CL, Chang DC, Wu AW (2004) The surgical recovery index. Surg Endosc 18: 596–600
Acknowledgments
This research was funded by a grant awarded to Drs. Stergiou and Oleynikov by the Nebraska Research Initiative.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Judkins, T.N., Oleynikov, D., Narazaki, K. et al. Robotic surgery and training: electromyographic correlates of robotic laparoscopic training. Surg Endosc 20, 824–829 (2006). https://doi.org/10.1007/s00464-005-0334-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0334-z