Abstract
Purpose
In this retrospective study, we evaluated the treatment patterns and survival after positron emission tomography-computed tomography (PET/CT)-guided local consolidation therapy (LCT) for oligometastatic non-small cell lung cancer (NSCLC).
Methods
We reviewed the medical records of Chinese patients with oligometastatic stage IV non-small cell lung cancer (≤ 5 metastases) who had undergone PET/CT and were eligible for systemic therapy at two centers between May 2005 and August 2019. Propensity score matching (1:1) was used to reduce selection bias and imbalanced distribution of confounding factors.
Results
We identified 84 eligible patients and used propensity scores to create well-matched groups of 35 patients who did or did not undergo LCT. Among all patients, the 1-year overall survival (OS) rate was 47.6% and the 2-year OS rate was 22.6%. Relative to the group that did not receive LCT, the LCT group had a significantly higher OS rate (13 months vs. 7 months, p = 0.002). The two groups had similar incidences and classifications of LCT-related side effects. In multivariable analysis, LCT was found to be strongly associated with a favorable OS (hazard ratio: 0.508, 95% confidence interval: 0.311–0.828, p = 0.001).
Conclusion
We concluded that LCT was significantly associated with improved clinical outcomes among the Chinese patients with oligometastatic NSCLC who were eligible for systemic treatment and could undergo PET/CT evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is increasing awareness regarding the concept of oligometastasis, which, relative to extensive metastasis, is thought to involve a milder stage of tumor invasion, with fewer metastases (≤ 3–5 metastases) and localization (Ashworth et al. 2013; De Rose et al. 2016; Mitchell et al. 2019). Multiple studies have shown that patients with stage IV non-small cell lung cancer (NSCLC) generally experience progression of advanced disease at the original sites of gross disease and that patients with oligometastasis may potentially be cured via local treatment (Iyengar et al. 2018). Thus, local consolidation therapy (LCT) involving surgery and radiotherapy (RT) is expected to prolong the survival of patients with oligometastatic NSCLC.
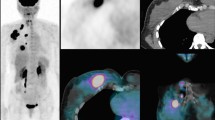
Effective management of patients with oligometastatic lung cancer relies on accurate information regarding tumor size, location, nodal involvement, and distant disease extent, which can be obtained via imaging modalities and tissue sampling. For example, 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) has been recommended for the initial evaluation of all patients with NSCLC, as it is more likely than other staging modalities to detect advanced disease and prevent futile surgery, RT, and/or chemotherapy from being carried out. In addition, FDG-PET can more accurately identify gross tumor deposits in three-dimensional space (Wahl et al. 2011), which provides useful information for RT planning (Bradley et al. 2012; Geiger et al. 2014; Houshmand et al. 2015; Simone et al. 2016), prognostication, and treatment response monitoring in patients with NSCLC (Khiewvan et al. 2016). However, there are insufficient clinical data regarding whether LCT and/or PET/CT have a role in the management of oligometastatic NSCLC, as the existing studies have generally been single-center retrospective studies with small samples, heterogeneous disease stages, and treatments based on conventional imaging. We believe that PET/CT can help characterize a tumor’s biology and potentially help identify resistance to specific treatments, which would facilitate more effective clinical decision making regarding combined and intensified treatments. Therefore, we retrospectively evaluated real-world LCT patterns and outcomes after PET/CT-guided management of patients with oligometastatic stage IV NSCLC on the basis of data from 84 patients who were treated at two Chinese centers.
Methods
Patients and data sources
We retrospectively identified 289 patients with stage IV NSCLC who had undergone systemic therapy (with or without surgery or RT as LCT) at the Liaoning Cancer Hospital and the First Hospital of China Medical University between May 2005 and August 2019. Their electronic medical records were reviewed to collect information regarding age, sex, smoking history, tumor size, histological type, performance status, primary tumor sites, comorbidities, therapeutic regimens, and date of death. The inclusion criteria were stage IV NSCLC with 1–5 concurrent metastases involving the liver, brain, lungs, bones, or other locations, as well as complete records regarding surgery, RT, and/or chemotherapy. Patients at these centers should have undergone multidisciplinary consultation for surgical indications. In addition, eligible patients were required to have undergone a PET/CT examination within 1 month before treatment, on the basis of previously reported PET/CT methodology (Wang et al. 2011). Patients were excluded if they had organ dysfunction (e.g., involving the liver, kidneys, or heart), more than one primary tumor, or an unknown metastasis status, had undergone multiple transfers, or had received targeted therapy or immunotherapy.
Adverse events were evaluated according to the Common Terminology Criteria for Adverse Events (version 4.0). Patients were grouped according to whether they had received or not received LCT within 2 months before or after the administration of systemic treatment. The study’s retrospective protocol was approved by the ethics committees of the Liaoning Cancer Hospital and the First Hospital of China Medical University, and the study was conducted in compliance with the Declaration of Helsinki. All data were anonymized, and the requirement for informed consent was waived.
Propensity score matching
Propensity score matching (PSM) was used to create groups of patients that did and did not receive LCT to reduce the influence of selection bias and confounding variables. Propensity scores were estimated using the PSM function of IBM SPSS software, and PSM was performed using 1:1 nearest neighbor matching with a caliper width of 0.02. The Chi squared test was used to examine covariate balances before and after PSM for the groups of patients with and without LCT as well as for the various subgroups.
Statistical analysis
Demographic characteristics and clinicopathological features were reported as number (percentage) and compared using the Chi squared test. Overall survival (OS) was calculated from the date of first diagnosis to the date of death or last follow-up for surviving patients. The OS curves were estimated using the Kaplan–Meier method and compared using the log-rank test. The Cox proportional hazards model was used for univariate and multivariate analyses and the results were reported as hazard ratios (HRs) and 95% confidence intervals (CIs). Variables with p values < 0.1 in the univariable analysis were selected for multivariable analysis. Statistical analysis was performed using IBM SPSS software (version 25.0; IBM Corporation, Armonk, NY), and subgroup analyses according to the baseline characteristics were performed by drawing forest plots for overall survival using Stata MP 14 software (Stata Corp LLC, College Station, TX). All tests were two sided, and the results were considered significant at p values < 0.05.
Results
Follow-up and outcomes
Among the 289 patients treated during the study period, 205 were excluded because of targeted therapy/immunotherapy, loss to follow-up, incomplete data, or unclear metastasis status. Thus, 84 patients were considered eligible for the study. During a median follow-up of 11 months, 7 patients survived (8.3%) and 77 patients died (91.7%), with the deaths being caused by tumor-related complications (73 cases) and non-tumor-related complications (myocardial infarction in 2 cases and a cerebrovascular event in 2 cases). On the basis of the PSM, we created well-balanced groups of 35 patients who did or did not receive LCT (Fig. 1).
Patient characteristics and distant metastasis
The 70 matched patients (35 patients in the LCT group and 35 patients in the control group) included 50 men (71.4%) and 20 women (28.6%) with pathological diagnoses of squamous cell carcinoma (28 cases, 40%), adenocarcinoma (31 cases, 44.3%), and other carcinoma types (11 cases, 15.7%). Table 1 shows the patients’ characteristics. Three patients received surgery as local treatment, 42 patients received RT (biological equivalent dose of ≥ 36 Gy), and 1 patient received surgery plus RT. There were 46 patients (65.7%) with 2–5 metastases. The most common sites were intrathoracic metastasis (41 cases, 58.6%), bone metastasis (33 cases, 47.1%), liver metastasis (15 cases, 21.4%), adrenal metastasis (8 cases, 11.4%), and brain metastasis (3 cases, 4.3%). Single-organ metastasis was observed in 33 cases, and metastasis to 2–3 organs was observed in 37 cases. The overall median survival time was 11 months (1-year OS rate: 47.6%, 2-year OS rate: 22.6%).
Prognostic factors
Tables 2 and 3 show the significant variables from univariate analysis which included LCT status, lymph node metastasis, and weight loss (all p < 0.05). Given the heterogeneity of the study sample, we did not evaluate the effects of different chemotherapy regimens on prognosis. Figure 2 shows that, among our patients with oligometastatic stage IV NSCLC, LCT of the tumor site (primary tumor and/or distant metastasis) was associated with a significantly improved median OS (13 months vs. 7 months, p = 0.002). Subgroup analyses according to the patients’ clinical characteristics also confirmed that LCT was associated with a significantly longer OS in all subgroups (Fig. 3). Multivariate analysis confirmed that LCT independently predicted a better OS for oligometastatic NSCLC (p = 0.001) (Tables 4 and 5).
Discussion
Most deaths caused by NSCLC are related to the development and growth of distant metastases, which highlights the importance of systemic disease control (Fidler 2003). However, optimal treatment selection remains challenging for this patient group. A large trial investigated the potential benefit of four platinum-based doublet chemotherapy regimens (cisplatin plus either paclitaxel, gemcitabine, or docetaxel, and carboplatin plus paclitaxel) in 1155 patients with metastatic NSCLC; however, the results revealed that none of these regimens were significantly superior (Schiller et al. 2002). This finding may be related to the variable biology of metastatic lesions, which might respond differently to therapy (vs. the primary tumor), and highlights the importance of biological characterization if metastatic lesions. Pretreatment tumor characterization using PET might help guide treatment selection, such as surgery, RT, or specific chemotherapy regimens. Although it seems intuitive that improving patient selection and tumor targeting would improve the results of RT, there is little information regarding long-term patient outcomes to justify the use of PET/CT for planning LCT in cases of oligometastatic stage IV NSCLC. Our earlier study on FDG-PET scanning (Wang et al. 2012a) revealed that this technique influenced patient selection for curative treatment and frequently changed the RT target volumes. The present study investigated PET/CT-based management using different regimens (chemotherapy vs. chemotherapy plus LCT), which revealed that chemotherapy plus LCT was associated with better long-term survival. Furthermore, our treatment results tended to be better than previously reported results for stage IV NSCLC (Song et al. 2018). We suspect that the PET/CT evaluation might have improved the selection of surgery or RT for patients with NSCLC and previously unknown metastatic disease. The PET/CT evaluation may also increase the likelihood of correctly delineating the tumor tissue. For example, we have previously reported (Wang et al. 2012b) that using FDG-PET during RT planning for NSCLC helped improve the reliability of target volume delineation and allowed for a higher tumor dose without an increased risk of side effects. Thus, by more reliably confining the planning target volume to morphologically and functionally visible tumor manifestations, less normal tissue would be irradiated, and a higher total tumor dose would be possible. Several studies have shown that PET/CT planning for NSCLC patients allowed for a significantly higher threshold for the intolerable total dose (68.9 Gy vs. 55.2 Gy for CT alone), on the basis of commonly accepted dose restrictions for normal tissues (De Ruysscher et al. 2005; Greco et al. 2007; Gregoire et al. 2007; Grills et al. 2007; MacManus et al. 2009; Nestle et al. 2002).
Oligometastatic NSCLC is a unique disease and research has focused on improving outcomes using appropriate management strategies. Several retrospective studies (Gomez et al. 2016; Iyengar et al. 2014; Petty et al. 2018) have suggested that LCT has a role in the management of oligometastatic NSCLC, with selection criteria involving lymph node status, tumor histology, thoracic disease bulk, performance status, and number of metastatic sites. On the basis of these criteria, LCT may help improve the effects of systemic treatment for lung cancers. For example, Iyengar et al. (Iyengar et al. 2014) evaluated 24 patients with advanced NSCLC who experienced progression after platinum-based chemotherapy and reported that 16 patients underwent stereotactic body radiation therapy. The results indicated that RT provided significantly better PFS and OS, relative to historical values for patients who had received only systemic treatment. A later prospective study (Iyengar et al. 2018) involved 29 patients with oligometastatic stage IV NSCLC, including 14 patients who were treated using stereotactic ablative radiotherapy (SAbR) plus maintenance chemotherapy and 15 patients who were treated using maintenance chemotherapy. That trial was closed early after an interim analysis revealed that SAbR plus maintenance chemotherapy yielded significantly improved PFS (9.7 months vs. 3.5 months, p = 0.01). In addition to the nearly tripling of the PFS value in that trial, the use of consolidative SAbR before maintenance chemotherapy did not increase the risk of toxicities in patients with limited metastatic NSCLC. Petty et al. (2018) also reported on 27 patients who fulfilled the criteria for combined RT. Although the study was ended prematurely because of slow patient accumulation, the results fulfilled the primary endpoint for success (PFS > 6 months, p < 0.0001), with a median PFS of 11.2 months (95% CI 7.6–15.9 months) and a median OS of 28.4 months (95% CI 14.5–45.8 months). Thus, among patients with oligometastatic NSCLC, intensive RT combined with non-maintenance chemotherapy after chemotherapy appears to yield significant long-term efficacy. Further studies are needed to validate the efficacy of LCT and standardize its use.
Gomez et al. (2016) conducted the first clinical trial of LCT plus standard maintenance therapy for all sites, which revealed a median PFS of 11.9 months (90% CI 5.7–20.9 months) in the LCT group and 3.9 months (90% CI 2.3–6.6 months) in the maintenance group. This difference was statistically significant (HR: 0.35, 90% CI 0.18–0.66; log-rank p = 0.0054), and both groups experienced similar side effects, with no treatment-related deaths or grade 4 adverse events. Moreover, the 1-year PFS rates were 48% in the LCT group (90% CI 28.7–65.7%) and 20% in the maintenance treatment group (90% CI 7.1–38.0%). Thus, relative to maintenance therapy/observation, LCT after systemic therapy for oligometastatic NSCLC appears to be feasible and tolerable and to yield a significant improvement in PFS. The researchers also reported that LCT was associated with a significantly longer time to appearance of new lesions. On the basis of these results, LCT appears to have a role in the management of oligometastatic stage IV NSCLC, in addition to traditional systemic therapy, although it is important to note that these data were derived from a few studies in American and French populations (Gomez et al. 2019; Rusthoven et al. 2009; Su et al. 2016; Zhang et al. 2018). Given the regional and ethnic differences in NSCLC cases, further studies are needed to confirm that LCT does indeed have a good efficacy, with acceptable side effects, in other populations. To the best of our knowledge, ours is the first study to address this issue in a cohort of Chinese patients with oligometastatic NSCLC who have unique genotypic and clinical characteristics. All of the patients in the present study received systemic chemotherapy to control their disease, and our results suggest that LCT may help address any lack of chemotherapy efficacy without increasing the risk of serious adverse events or treatment-related death. This finding is consistent with the reported results from previous studies. Therefore, despite the limitations related to a small sample size, retrospective design, and heterogeneous patient characteristics, our results suggest that LCT is feasible in this setting and requires further research.
Conclusions
Stage IV NSCLC is a systemic disease with a very poor prognosis, and the concept of oligometastasis may provide new insights regarding its treatment. For oligometastatic stage IV NSCLC, the combination of active LCT and systemic chemotherapy may help improve survival without increasing the incidence of side effects, relative to maintenance therapy or observation alone. Furthermore, the use of PET/CT may help clearly identify the disease and potentially help improve patient outcomes. However, further studies are needed to develop a standard for selecting LCT in cases of oligometastatic stage IV NSCLC.
References
Ashworth A, Rodrigues G, Boldt G, Palma D (2013) Is there an oligometastatic state in non-small cell lung cancer? A systematic review of the literature. Lung Cancer 82:197–203. https://doi.org/10.1016/j.lungcan.2013.07.026
Bradley J et al (2012) A phase II comparative study of gross tumor volume definition with or without PET/CT fusion in dosimetric planning for non-small-cell lung cancer (NSCLC): primary analysis of Radiation Therapy Oncology Group (RTOG) 0515. Int J Radiat Oncol Biol Phys 82:435–441. https://doi.org/10.1016/j.ijrobp.2010.09.033(e431)
De Rose F et al (2016) Clinical outcome of stereotactic ablative body radiotherapy for lung metastatic lesions in non-small cell lung cancer oligometastatic patients. Clin Oncol (R Coll Radiol) 28:13–20. https://doi.org/10.1016/j.clon.2015.08.011
De Ruysscher D et al (2005) Effects of radiotherapy planning with a dedicated combined PET-CT-simulator of patients with non-small cell lung cancer on dose limiting normal tissues and radiation dose-escalation: a planning study. Radiother Oncol 77:5–10. https://doi.org/10.1016/j.radonc.2005.06.014
Fidler IJ (2003) The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer 3:453–458. https://doi.org/10.1038/nrc1098
Geiger GA et al (2014) Stage migration in planning PET/CT scans in patients due to receive radiotherapy for non-small-cell lung cancer. Clin Lung Cancer 15:79–85. https://doi.org/10.1016/j.cllc.2013.08.004
Gomez DR et al (2016) Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol 17:1672–1682. https://doi.org/10.1016/s1470-2045(16)30532-0
Gomez DR et al (2019) Local consolidative therapy vs maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. Clin Oncol 37:1558–1565. https://doi.org/10.1200/JCO.19.00201
Greco C, Rosenzweig K, Cascini GL, Tamburrini O (2007) Current status of PET/CT for tumour volume definition in radiotherapy treatment planning for non-small cell lung cancer (NSCLC). Lung Cancer 57:125–134. https://doi.org/10.1016/j.lungcan.2007.03.020
Gregoire V, Haustermans K, Geets X, Roels S, Lonneux M (2007) PET-based treatment planning in radiotherapy: a new standard? J Nucl Med 48(Suppl 1):68S–77S
Grills IS, Yan D, Black QC, Wong CY, Martinez AA, Kestin LL (2007) Clinical implications of defining the gross tumor volume with combination of CT and 18FDG-positron emission tomography in non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 67:709–719. https://doi.org/10.1016/j.ijrobp.2006.09.046
Houshmand S, Boursi B, Salavati A, Simone CB 2nd, Alavi A (2015) Applications of fluorodeoxyglucose PET/computed tomography in the assessment and prediction of radiation therapy-related complications. PET Clin 10:555–571. https://doi.org/10.1016/j.cpet.2015.05.003
Iyengar P et al (2014) Phase II trial of stereotactic body radiation therapy combined with erlotinib for patients with limited but progressive metastatic non-small-cell lung cancer. J Clin Oncol 32:3824–3830. https://doi.org/10.1200/JCO.2014.56.7412
Iyengar P et al (2018) Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol 4:e173501. https://doi.org/10.1001/jamaoncol.2017.3501
Khiewvan B, Ziai P, Houshmand S, Salavati A, Ziai P, Alavi A (2016) The role of PET/CT as a prognosticator and outcome predictor in lung cancer Expert Rev. Respir Med 10:317–330. https://doi.org/10.1586/17476348.2016.1147959
MacManus M et al (2009) Use of PET and PET/CT for radiation therapy planning: IAEA expert report 2006–2007. Radiother Oncol 91:85–94. https://doi.org/10.1016/j.radonc.2008.11.008
Mitchell KG et al (2019) Improved overall survival with local consolidative therapy in oligometastatic non-small cell lung cancer: results from a cohort of 194 patients with synchronous disease. Int J Radiat Oncol Biol Phys 104:229. https://doi.org/10.1016/j.ijrobp.2019.01.011
Nestle U et al (2002) 2-Deoxy-2-[18F]fluoro-d-glucose positron emission tomography in target volume definition for radiotherapy of patients with non-small-cell lung cancer. Mol Imaging Biol 4:257–263
Petty WJ et al (2018) Long-term outcomes of a phase 2 trial of chemotherapy with consolidative radiation therapy for oligometastatic non-small cell lung cancer. Int J Radiat Oncol Biol Phys 102:527–535. https://doi.org/10.1016/j.ijrobp.2018.06.400
Rusthoven KE, Hammerman SF, Kavanagh BD, Birtwhistle MJ, Stares M, Camidge DR (2009) Is there a role for consolidative stereotactic body radiation therapy following first-line systemic therapy for metastatic lung cancer? A patterns-of-failure analysis. Acta Oncol 48:578–583. https://doi.org/10.1080/02841860802662722
Schiller JH et al (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346:92–98. https://doi.org/10.1056/NEJMoa011954
Simone CB, Houshmand S, Kalbasi A, Salavati A, Alavi A (2016) PET-based thoracic radiation oncology. PET Clin 11:319–332. https://doi.org/10.1016/j.cpet.2016.03.001
Song YQ et al (2018) Prognostic factors of IV stage non-small cell lung cancer and the potential significance of thoracic radiotherapy. J Mod Oncol 26(08):1207–1211. https://doi.org/10.3969/j.issn.1672-4992.2018.08.014
Su S et al (2016) Might radiation therapy in addition to chemotherapy improve overall survival of patients with non-oligometastatic stage IV non-small cell lung cancer?: Secondary analysis of two prospective studies. BMC Cancer 16:908. https://doi.org/10.1186/s12885-016-2952-3
Wahl RL, Herman JM, Ford E (2011) The promise and pitfalls of positron emission tomography and single-photon emission computed tomography molecular imaging-guided radiation therapy. Semin Radiat Oncol 21:88–100. https://doi.org/10.1016/j.semradonc.2010.11.004
Wang TL et al (2011) Effect of PET-CT on clinical stage of NSCLC and target area delineation in 3D conformal radiotherapy. Chin J Radiat Oncol 20(2):99–100. https://doi.org/10.3760/cma.j.isan.1004-4221.2011.02.005
Wang TL et al (2012a) Impact of PET/CT on the target volume delineation and treatment management of non-small cell lung cancer complicated with atelectasis. Chin J Nucl Med Mol Imaging 32(2):115–118. https://doi.org/10.11735/j.issn.1004-0242.2017.01.A011
Wang TL et al (2012b) Impact of PET/CT on dosimetric parameters of three-dimensional conformal radiotherapy planning in patients with non-small cell lung cancer. Chin J Cancer Prev Treat 19(4):284–286. https://doi.org/10.3969/j.issn.1674-4985.2016.26.001
Zhang R et al (2018) Radiotherapy improves the survival of patients with stage IV NSCLC: A propensity score matched analysis of the SEER database. Cancer Med 7:5015–5026. https://doi.org/10.1002/cam4.1776
Funding
This study was supported by grants from the National Cancer Institute, Cancer Research [NCC2017A08], the Liaoning Province Natural Science Foundation [20180550741], Shenyang Major Scientific Research Projects [19-112-4-090], and Liaoning Province Key Area Joint Open Fund [2019-KF-01-01].
Author information
Authors and Affiliations
Contributions
Conceptualization: YQS, NW, and YQ; data curation: TLW; software management: QKY; formal analysis: YQS, NW, and YQ; project administration: YQ; validation: YWR.; visualization: YQS and NW; writing the original draft: YQS., NW, and YQ; draft review and editing: all authors; modify and polish: RZW and RH; funding acquisition: TLW, additional resources: TLW.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, YQ., Wang, N., Qiao, Y. et al. Treatment patterns and survival after 18F-fluorodeoxyglucose positron emission tomography/computed tomography-guided local consolidation therapy for oligometastatic non-small cell lung cancer: a two-center propensity score-matched analysis. J Cancer Res Clin Oncol 146, 1021–1031 (2020). https://doi.org/10.1007/s00432-020-03134-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03134-9