Abstract
Purpose
To estimate the effect of metabolic syndrome (MetS) on the prevalence of prostate cancer using a large retrospective cohort with a 5-year follow-up duration.
Methods
National Health Insurance Service health checkup cohort was used for the study. In total, 130,342 men included in the health checkup cohort in 2009 were divided into two groups according to the presence of prostate cancer. The prevalence of prostate cancer from 2009 to 2013 was cumulatively calculated from 2003. A generalized estimating equation was used to assess the effect of MetS and its component on the prevalence of prostate cancer after adjusting for other variables.
Results
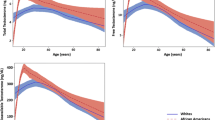
Prostate cancer was present in 2369 men (1.8%) in 2009. The prevalence of prostate cancer was significantly higher in patients with MetS than in those without MetS throughout the entire follow-up duration. Multivariable analysis showed that in addition to year at evaluation and age, the presence of MetS was associated with an increased prevalence of prostate cancer. Alcohol consumption and smoking levels were negatively associated with the prevalence of prostate cancer. Among MetS components, decreased high density lipoprotein (HDL)-cholesterolemia and central obesity were associated with an increased prevalence of prostate cancer after adjusting for other variables.
Conclusion
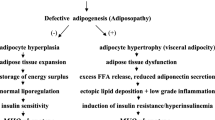
MetS and its components, especially decreased HDL-cholesterol levels and central obesity, were related to the increased prevalence of prostate cancer. Preventing MetS, maintaining high HDL-cholesterol level, and maintaining low waist circumference might be useful ways for decreasing the prevalence of prostate cancer.
Similar content being viewed by others
References
Ahn J, Lim U, Weinstein SJ, Schatzkin A, Hayes RB, Virtamo J, Albanes D (2009) Prediagnostic total and high-density lipoprotein cholesterol and risk of cancer. Cancer Epidemiol Prev Biomark 18:1055–9965. (EPI-1008-1248)
Alexandrov LB et al (2016) Mutational signatures associated with tobacco smoking in Human Cancer. Science 354:618–622
Baade PD, Youlden DR, Cramb SM, Dunn J, Gardiner RA (2013) Epidemiology of prostate cancer in the Asia–Pacific region. Prostate Int 1:47–58
Bhindi B et al (2015) Dissecting the association between metabolic syndrome and prostate cancer risk: analysis of a large clinical cohort. Eur Urol 67:64–70
Bhindi B et al (2016) Influence of metabolic syndrome on prostate cancer stage, grade, and overall recurrence risk in men undergoing radical prostatectomy. Urology 93:77–85
Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL (2015) Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 351:h4238
Cowey S, Hardy RW (2006) The metabolic syndrome: a high-risk state for cancer? Am J Pathol 169:1505–1522
Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Mucci LA, Kaprio J (2016) Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 27:1049–1058
Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D (2012) Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care 35:2402–2411
Ferlay J et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012 Int J Cancer 136: E359–E386
Gacci M et al (2015) Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int 115:24–31
Gacci M et al (2017) Meta-analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis 20:146
Grönberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864
Grundy SM et al (2004) Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Circulation 110:227–239. https://doi.org/10.1161/01.cir.0000133317.49796.0e
Klein EA et al (2011) Vitamin E and the risk of prostate cancer: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 306:1549–1556
Kwiterovich PO Jr (2000) The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: a current review. Am J Cardiol 86:5 l–10 l
Lippman SM et al (2009) Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 301:39–51
Mistry T, Digby JE, Desai KM, Randeva HS (2007) Obesity and prostate cancer: a role for adipokines. Eur Urol 52:46–53. https://doi.org/10.1016/j.eururo.2007.03.054
Mondul AM, Weinstein SJ, Virtamo J, Albanes D (2011) Serum total and HDL cholesterol and risk of prostate cancer. Cancer Causes Control 22:1545
Mottet N et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629
Oremosu AA, Akang EN (2015) Impact of alcohol on male reproductive hormones, oxidative stress and semen parameters in Sprague–Dawley rats. Middle East Fertil Soc J 20:114–118
Parikesit D, Mochtar CA, Umbas R, Hamid ARAH (2016) The impact of obesity towards prostate diseases. Prostate Int 4:1–6. https://doi.org/10.1016/j.prnil.2015.08.001
Rhee H, Vela I, Chung E (2016) Metabolic syndrome and prostate cancer: a review of complex interplay amongst various endocrine factors in the pathophysiology and progression of prostate cancer. Horm Cancer 7:75–83
Sawada N, Inoue M, Iwasaki M, Sasazuki S, Yamaji T, Shimazu T, Tsugane S (2014) Alcohol and smoking and subsequent risk of prostate cancer in Japanese men: the Japan Public Health Center-based prospective study. Int J Cancer 134:971–978
Schoonen WM, Salinas CA, Kiemeney LA, Stanford JL (2005) Alcohol consumption and risk of prostate cancer in middle-aged men. Int J Cancer 113:133–140
Stewart B, Wild CP (eds) (2017) World cancer report 2014. International Agency for Research on Cancer, Lyon (ISBN: 978-92-832-0429-9)
Van Hemelrijck M et al (2011) Low levels of apolipoprotein AI and HDL are associated with risk of prostate cancer in the Swedish AMORIS study. Cancer Causes Control 22:1011–1019
Yoo S, Oh S, Park J, Cho SY, Cho MC, Jeong H, Son H (2018) The impacts of metabolic syndrome and life style on the prevalence of benign prostatic hyperplasia requiring treatment: historical cohort study using 130,454 men. BJU Int. https://doi.org/10.1111/bju.14528
Zuccolo L, Lewis SJ, Donovan JL, Hamdy FC, Neal DE, Smith GD (2013) Alcohol consumption and PSA-detected prostate cancer risk—a case-control nested in the ProtecT study. Int J Cancer 132:2176–2185
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animal
Not applicable.
Informed consent
Informed consent waive by IRB.
Rights and permissions
About this article
Cite this article
Yoo, S., Oh, S., Park, J. et al. Effects of metabolic syndrome on the prevalence of prostate cancer: historical cohort study using the national health insurance service database. J Cancer Res Clin Oncol 145, 775–780 (2019). https://doi.org/10.1007/s00432-019-02842-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02842-1