Abstract
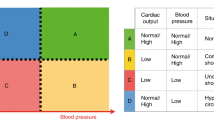
Physiologic-based management of hemodynamic instability is proven to guide the logical selection of cardiovascular support and shorten the time to clinical recovery compared to an empiric approach that ignores the heterogeneity of the hemodynamic instability related mechanisms. In this report, we classified neonatal hemodynamic instability, circulatory shock, and degree of compensation into five physiologic categories, based on different phenotypes of blood pressure (BP), other clinical parameters, echocardiography markers, and oxygen indices. This approach is focused on hemodynamic instability in infants with normal cardiac anatomy.
Conclusion: The management of hemodynamic instability is challenging due to the complexity of the pathophysiology; integrating different monitoring techniques is essential to understand the underlying pathophysiologic mechanisms and formulate a physiologic-based medical recommendation and approach.
What is Known: • Physiologic-based assessment of hemodynamics leads to targeted and pathophysiologic-based medical recommendations. | |
What is New: • Hemodynamic instability in neonates can be categorized according to the underlying mechanism into five main categories, based on blood pressure phenotypes, systemic vascular resistance, and myocardial performance. • The new classification helps with the targeted management and logical selection of cardiovascular support. |



Similar content being viewed by others
Availability of data and material
Yes.
Code availability
N/A.
Abbreviations
- BP:
-
Blood pressure
- DBP:
-
Diastolic blood pressure
- DO2 :
-
Oxygen delivery
- FOE:
-
Fractional oxygen extraction
- PDA:
-
Patent ductus arteriosus
- PP:
-
Pulse pressure
- PVR:
-
Pulmonary vascular resistance
- MABP:
-
Mean arterial blood pressure
- NIRS:
-
Near-infrared spectroscopy
- POCUS:
-
Point of care ultrasound
- StO2 :
-
Tissue oxygen saturation
- VO2 :
-
Oxygen consumption
- SBP:
-
Systolic blood pressure
- SpO2 :
-
Arterial oxygen saturation
- SVR:
-
Systemic vascular resistance
References
Burton VJ, Gerner G, Cristofalo E, Chung S en, Jennings JM, Parkinson C et al (2015) A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia. BMC Neurol 15(1):1–13
Chock VY, Ramamoorthy C, Van Meurs KP (2012) Cerebral autoregulation in neonates with a hemodynamically significant patent ductus arteriosus. J Pediatr [Internet]. [cited 2012 May 5] 160(6):936–42. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022347611012285
Eriksen VR, Hahn GH, Greisen G (2015) Cerebral autoregulation in the preterm newborn using near-infrared spectroscopy: a comparison of time-domain and frequency-domain analyses. J Biomed Opt 20(3):037009
Votava-Smith JK, Statile CJ, Taylor MD, King EC, Pratt JM, Nelson DP et al (2017) Impaired cerebral autoregulation in preoperative newborn infants with congenital heart disease. J Thorac Cardiovasc Surg [Internet] 154(3):1038–44. Available from: https://doi.org/10.1016/j.jtcvs.2017.05.045
Allen BW, Stamler JS, Piantadosi CA (2009) Hemoglobin, nitric oxide and molecular mechanisms of hypoxic vasodilation. Trends Mol Med 15(10):452–60
Hickok RL, Spaeder MC, Berger JT, Schuette JJ, Klugman D (2016) Postoperative abdominal NIRS values predict low cardiac output syndrome in neonates. World J Pediatr Congenit Hear Surg [Internet] 7(2):180–4. Available from: https://doi.org/10.1177/2150135115618939
Chock VY, Kwon SH, Ambalavanan N, Batton B, Nelin LD, Chalak LF et al (2020) Cerebral oxygenation and autoregulation in preterm infants (early NIRS study). J Pediatr 227:94-100.e1
Bozzetti V, Paterlini G, Meroni V, DeLorenzo P, Gazzolo D, Van Bel F et al (2012) Evaluation of splanchnic oximetry, Doppler flow velocimetry in the superior mesenteric artery and feeding tolerance in very low birth weight IUGR and non-IUGR infants receiving bolus versus continuous enteral nutrition. BMC Pediatr [Internet] 12(1):106. Available from: BMC Pediatrics
Martini S, Corvaglia L (2018) Splanchnic NIRS monitoring in neonatal care: rationale, current applications and future perspectives. J Perinatol [Internet] 1–13. Available from: https://doi.org/10.1038/s41372-018-0075-1
Verhagen EA, Hummel LA, Bos AF, Kooi EMW (2014) Near-infrared spectroscopy to detect absence of cerebrovascular autoregulation in preterm infants. Clin Neurophysiol [Internet] 125(1):47–52. Available from: http://www.clinph-journal.com/article/S1388245713009280/fulltext
Tortoriello TA, Stayer SA, Mott AR, McKenzie ED, Fraser CD, Andropoulos DB et al (2005) A noninvasive estimation of mixed venous oxygen saturation using near-infrared spectroscopy by cerebral oximetry in pediatric cardiac surgery patients. Paediatr Anaesth 15(6):495–503
Elsayed YN, Louis D, Ali YH, Amer R, Seshia MM, Patrick J et al (2018) Integrated evaluation of hemodynamics: a novel approach for the assessment and management of preterm infants with compromised systemic circulation. J Perinatol (1)
Dempsey EM, Barrington KJ, Marlow N, O’Donnell CPF, Miletin J, Naulaers G et al (2021) Hypotension in preterm infants (HIP) randomised trial. Arch Dis Child Fetal Neonatal Ed
Elsayed YN, Amer R, Seshia MM (2017) The impact of integrated evaluation of hemodynamics using targeted neonatal echocardiography with indices of tissue oxygenation: a new approach. J Perinatol
Seear M, Wensley D, MacNab A (1993) Oxygen consumption-oxygen delivery relationship in children. J Pediatr 123(2):208–214
Giesinger RE, McNamara PJ (2016) Hemodynamic instability in the critically ill neonate: an approach to cardiovascular support based on disease pathophysiology. Semin Perinatol [Internet] 40(3):174–88. Available from: https://doi.org/10.1053/j.semperi.2015.12.005
Barrington KJ (2008) Hypotension and shock in the preterm infant. Semin Fetal Neonatal Med 2008:16–23
Alderliesten T, Lemmers PMA, van Haastert IC, de Vries LS, Bonestroo HJC, Baerts W et al (2014) Hypotension in preterm neonates: low blood pressure alone does not affect neurodevelopmental outcome. J Pediatr [Internet] 164(5):986–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24484771
Parker MM (2014) Hemodynamics in preterm neonates with septic shock. Pediatr Crit Care Med [Internet] 15:494–5. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00130478-201406000-00015
Perera P, Mailhot T, Riley D, Mandavia D (2010) The RUSH exam: rapid ultrasound in shock in the evaluation of the critically lll. Emerg Med Clin North Am [Internet] 28(1):29–56. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0733862709001175
Thewissen L, Caicedo A, Lemmers P, Van BF, Van HS, Naulaers G (2018) Measuring near-infrared spectroscopy derived cerebral autoregulation in neonates: from research tool toward bedside multimodal monitoring. Front Pediatr 6(May):1–21
Tweddell JS, Ghanayem NS, Hoffman GM (2010) Pro: NIRS is “standard of care” for postoperative management. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu [Internet] 13(1):44–50. Available from: https://doi.org/10.1053/j.pcsu.2010.02.008
Sood BG, McLaughlin K, Cortez J (2015) Near-infrared spectroscopy: applications in neonates. Semin Fetal Neonatal Med [Internet] 20(3):164–72. Available from: https://doi.org/10.1016/j.siny.2015.03.008
Amer R, Kalash R, Seshia MM, Elsayed YN (2017) The impact of integrated evaluation of hemodynamics on management of preterm infants with late-onset compromised systemic circulation. Am J Perinatol
van Vonderen JJ, Roest AW, Siew ML, Walther FJ, Hooper SB, Te Pas AB (2014) Measuring physiological changes during the transition to life after birth. Neonatology [Internet]. [cited 2014 Mar 24] 105(3):230–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24504011
Singh Y (2017) Echocardiographic evaluation of hemodynamics in neonates and children. Front Pediatr 5(September):1–14
Wynn JL, Wong HR (2010) Pathophysiology and treatment of septic shock in neonates. Clin Perinatol [Internet] 37(2):439–79. Available from: https://doi.org/10.1016/j.clp.2010.04.002
Elsayed Y, Fraser D (2016) Integrated evaluation of neonatal hemodynamics program optimizing organ perfusion and performance in critically ill neonates, part 1 : understanding physiology of neonatal hemodynamics. Neonatal Netw 143–50
Giesinger RE, Bailey LJ, Deshpande P, McNamara PJ (2016) Hypoxic-ischemic encephalopathy and therapeutic hypothermia: the hemodynamic perspective. J Pediatr [Internet] 1–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27742125
Fraser D (2017) Patent ductus arteriosus in preterm infants, part 1 : understanding the pathophysiologic link between the patent ductus arteriosus and clinical complications. 36(5):265–72
Giesinger RE, Elsayed YN, Castaldo MP, McNamara PJ (2019) Targeted neonatal echocardiography-guided therapy in vein of galen aneurysmal malformation: a report of two cases with a review of physiology and approach to management. AJP Rep 9(2):E172–E176
Selim A, El Wahab AA, Salem H, Yahmadi MA, Al Aisary S, Malviya M et al (2020) Perioperative management of arteriovenous malformation guided by integrated evaluation of hemodynamics. Eur J Pediatr
Boet A, Jourdain G, Demontoux S, De Luca D (2016) Stroke volume and cardiac output evaluation by electrical cardiometry: accuracy and reference nomograms in hemodynamically stable preterm neonates. J Perinatol 36(9):748–752
Noori S, McCoy M, Anderson MP, Ramji F, Seri I (2014) Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr [Internet] 164(2):264–270.e3. Available from: http://linkinghub.elsevier.com/retrieve/pii/S002234761301216X
Jones P (1999) Haemodynamic measurements (continuous cardiac output and systemic vascular resistance) in critically ill patients: transoesophageal Doppler versus continuous thermodilution. Crit Care 1(1):33–37
Abbas AE, Fortuin FD, Patel B, Moreno CA, Schiller NB, Lester SJ (2004) Noninvasive measurement of systemic vascular resistance using Doppler echocardiography. J Am Soc Echocardiogr 17(8):834–838
Cerussi A, Van Woerkom R, Waffarn F, Tromberg B (2005) Noninvasive monitoring of red blood cell transfusion in very low birthweight infants using diffuse optical spectroscopy. J Biomed Opt [Internet] 10(5):051401. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16292938
Amer R, Elsayed YN, Graham MR, Sikarwar AS, Hinton M, Dakshinamurti S (2019) Effect of vasopressin on a porcine model of persistent pulmonary hypertension of the newborn. J of pediatr pulmonology (December 2018):319–32
Wynn JL, Wong HR (2010) Pathophysiology and treatment of septic shock in neonates. Clin Perinatol 37(2):439–479
Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC et al (2017) American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med 45:1061–1093
Limperopoulos C, Gauvreau KK, O’Leary H, Moore M, Bassan H, Eichenwald EC et al (2008) Cerebral hemodynamic changes during intensive care of preterm infants. Pediatrics [Internet] 122(5):e1006–13. Available from: https://pediatrics.aappublications.org/content/122/5/e1006/tab-e-letters. https://doi.org/10.1542/peds.2008-0768
Elsayed YFD (2016) Integrated evaluation of neonatal hemodynamics, part 2: systematic bedside assessment. Neonatal Netw 192–203
Dempsey E, Cabañas F, De Boode WP, Vrancken SL, Van Heijst AF (2018) Neonatal hemodynamics: from developmental physiology to comprehensive monitoring. Front Pediatr 687(6):1–15
Fortas F, Di Nardo M, Yousef N, Humbert M, De Luca D (2021) Life-threatening PPHN refractory to nitric oxide: proposal for a rational therapeutic algorithm. Eur J Pediatr 180(8):2379–2387
Manouchehri N, Bigam DL, Churchill T, Rayner D, Joynt C, Cheung PY (2013) A comparison of combination dopamine and epinephrine treatment with high-dose dopamine alone in asphyxiated newborn piglets after resuscitation. Pediatr Res [Internet]. [cited 2014 Mar 5] 73(4 Pt 1):435–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23344679
Bonestroo HJC, Lemmers PMA, Baerts W, van Bel F (2011) Effect of antihypotensive treatment on cerebral oxygenation of preterm infants without PDA. Pediatrics 128(6):e1502–10.
Elsayed Y, Seshia M, Soni R, Buffo I, Baier RJ (2016) Pre-symptomatic prediction of morbitidies in preterm infants with patent ductus arteriosus by targeted neonatal echocardiography and brain-type natriuretic peptide. J Pediatr Neonatal Individual Med 5(2):1–10
Farooqui MA, Elsayed YN, Jeyaraman MM, Dingwall O, Tagin M, Zarychanski R et al (2019) Pre-symptomatic targeted treatment of patent ductus arteriosus in preterm newborns: a systematic review and meta-analysis. J Neonatal Perinatal Med 12(1)
Elsayed Y, Seshia M, Baier RJ, Dakshinamurti S (2017) Serial serum brain-type natriuretic peptide (BNP) identifies compromised blood flow in infants with hemodynamically significant patent ductus arteriosus. J Pediatr Neonatal Individual Med 6(2):1–10
El-khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN et al (2015) A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr [Internet] 167(6):1354–1361.e2. Available from: https://doi.org/10.1016/j.jpeds.2015.09.028
Singh Y, Katheria AC, Vora F (2018) Advances in diagnosis and management of hemodynamic instability in neonatal shock. Front Pediatr 6(January):1–12
Singh Y, Tissot C (2018) Echocardiographic evaluation of transitional circulation for the neonatologists. Front Pediatr [Internet] 6(May):140. Available from: http://journal.frontiersin.org/article/https://doi.org/10.3389/fped.2018.00140/full
So KW, Fok TF, Ng PC, Wong WW, Cheung KL (1997) Randomised controlled trial of colloid or crystalloid in hypotensive preterm infants. Arch Dis Child Fetal Neonatal Ed 76(1):46–49
Banerjee J, Leung TS, Aladangady N (2016) Cerebral blood flow and oximetry response to blood transfusion in relation to chronological age in preterm infants. Early Hum Dev [Internet] 97:1–8. Available from: https://doi.org/10.1016/j.earlhumdev.2015.10.017
Elsayed YN, Fraser D (2017) Patent ductus arteriosus in preterm infants, part 1: understanding the pathophysiologic link between the patent ductus arteriosus and clinical complications. Neonatal Netw 36(5)
Vesoulis ZA, Rhoades J, Muniyandi P, Conner S, Cahill AG, Mathur AM (2018) Delayed cord clamping and inotrope use in preterm infants. J Matern Neonatal Med [Internet] 31(10):1327–34. Available from: https://doi.org/10.1080/14767058.2017.1315663
Rivers EP, Kruse JA, Jacobsen G, Shah K, Loomba M, Otero R et al (2007) The influence of early hemodynamic optimization on biomarker patterns of severe sepsis and septic shock*. Crit Care Med [Internet] 35(9):2016–24. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003246-200709000-00002
Opal SM, Scannon PJ, Vincent JL, White M, Carroll SF, Palardy JE et al (1999) Relationship between plasma levels of lipopolysaccharide (LPS) and LPS-binding protein in patients with severe sepsis and septic shock. J Infect Dis 180(5):1584–1589
Giesinger RE, El Shahed AI, Castaldo MP, Breatnach CR, Chau V, Whyte HE et al (2019) Impaired right ventricular performance is associated with adverse outcome after hypoxic ischemic encephalopathy. Am J Respir Crit Care Med 200(10):1294–1305
Mohamed A, Nasef N, Shah V, Mcnamara PJ (2013) Pulmonary hypertension in neonates: case series. 1–7
Bidegain M, Greenberg R, Simmons C, Dang C, Cotten CM, Smith PB (2010) Vasopressin for refractory hypotension in extremely low birth weight infants. J Pediatr [Internet] 157(3):502–4. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022347610003380
Mohamed A, Nasef N, Shah V, McNamara PJ (2014) Vasopressin as a rescue therapy for refractory pulmonary hypertension in neonates: case series. Pediatr Crit Care Med [Internet] 15(2):148–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24141655
Evans N, Kluckow M, Currie A (1998) Range of echocardiographic findings in term neonates with high oxygen requirements. Arch Dis Child Fetal Neonatal Ed [Internet] 78(2):F105–11. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1720754&tool=pmcentrez&rendertype=abstract
Sehgal A, Francis JV, James A, Mcnamara PJ (2010) Patent ductus arteriosus ligation and post-operative hemodynamic instability: case report and framework for enhanced neonatal care. Indian J Pediatr [Internet] 77(8):905–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20740386
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J et al (2020) International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24(1):1–16
Sasidharan R, Gupta N, Chawla D (2019) Dopamine versus epinephrine for fluid-refractory septic shock in neonates. Eur J Pediatr 178(1):113–114
Gupta S, Donn SM (2014) Neonatal hypotension: dopamine or dobutamine? Vol. 19, Seminars Fetal Neonatal Med
Hallik M, Ilmoja ML, Standing JF, Soeorg H, Jalas T, Raidmäe M et al (2020) Population pharmacokinetics and pharmacodynamics of dobutamine in neonates on the first days of life. Br J Clin Pharmacol 86(2):318–328
Mahoney L, Shah G, Crook D, Rojas-Anaya H, Rabe H (2016) A literature review of the pharmacokinetics and pharmacodynamics of dobutamine in neonates. Pediatr Cardiol 37(1):14–23
Pryds O, Christensen NJ, Friis-Hansen B (1990) Increased cerebral blood flow and plasma epinephrine in hypoglycemic, preterm neonates. Pediatrics 85(2):172–176
Tourneux P, Rakza T, Bouissou A, Krim G, Storme L (2008) Pulmonary circulatory effects of norepinephrine in newborn infants with persistent pulmonary hypertension. J Pediatr [Internet] 153(3):345–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18534241
Rizk MY, Lapointe A, Lefebvre F, Barrington KJ (2018) Norepinephrine infusion improves haemodynamics in the preterm infants during septic shock. Acta Paediatr Int J Paediatr 107(3):408–413
Acker SN, Kinsella JP, Abman SH, Gien J (2014) Vasopressin improves hemodynamic status in infants with congenital diaphragmatic hernia. J Pediatr [Internet] 165(1):53–58.e1. Available from: https://doi.org/10.1016/j.jpeds.2014.03.059
Budniok T, ElSayed Y, Louis D (2020) Effect of vasopressin on systemic and pulmonary hemodynamics in neonates. Am J Perinatol
Filippi L, Gozzini E, Daniotti M, Pagliai F, Catarzi S, Fiorini P (2011) Rescue treatment with terlipressin in different scenarios of refractory hypotension in newborns and infants. Pediatr Crit Care Med 12(6):237–241
McNamara PJ, Shivananda SP, Sahni M, Freeman D, Taddio A (2013) Pharmacology of milrinone in neonates with persistent pulmonary hypertension of the newborn and suboptimal response to inhaled nitric oxide. Pediatr Crit Care Med [Internet] 14(1):74–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23132395
Lechner E, Hofer A, Leitner-Peneder G, Freynschlag R, Mair R, Weinzettel R et al (2012) Levosimendan versus milrinone in neonates and infants after corrective open-heart surgery: a pilot study. Pediatr Crit Care Med 13(5):542–548
Lechner E, Moosbauer W, Pinter M, Mair R, Tulzer G (2007) Use of levosimendan, a new inodilator, for postoperative myocardial stunning in a premature neonate. Pediatr Crit Care Med 8(1):61–63
Kobayashi S, Fujimoto S, Koyama N, Fukuda S, Iwaki T, Tanaka T et al (2008) Late-onset circulatory dysfunction of premature infants and late-onset periventricular leukomalacia. Pediatr Int 50:225–231
Osborn DA (2005) Diagnosis and treatment of preterm transitional circulatory compromise. Early Hum Dev 81(5):413–22
Seri I, Tan R, Evans J (2001) Cardiovascular effects of hydrocortisone in preterm infants with pressor-resistant hypotension. Pediatrics 107(5):1070–1074
Noori S, Friedlich P, Wong P, Ebrahimi M, Siassi B, Seri I (2006) Hemodynamic changes after low-dosage hydrocortisone administration in vasopressor-treated preterm and term neonates
Ng PC (2006) A double-blind, randomized, controlled study of a “stress dose” of hydrocortisone for rescue treatment of refractory hypotension in preterm infants. Pediatrics [Internet] 117(2):367–75. Available from: http://pediatrics.aappublications.org/cgi/https://doi.org/10.1542/peds.2005-0869
Eriksen VR, Hahn GH, Greisen G (2014) Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatr 103(12):1221–1226
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
YE and MA conceptualized the article. YE and MA conducted the background literature search. YE devised the manuscript, and both authors agree to the formatting and contents.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
N/A.
Consent for publication
Yes.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elsayed, Y., Abdul Wahab, M. A new physiologic-based integrated algorithm in the management of neonatal hemodynamic instability. Eur J Pediatr 181, 1277–1291 (2022). https://doi.org/10.1007/s00431-021-04307-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04307-5