Abstract
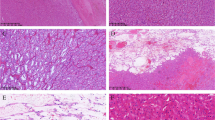
The spectrum of the renal oncocytic tumors has been expanded in recent years to include several novel and emerging entities. We describe a cohort of novel, hitherto unrecognized and morphologically distinct high-grade oncocytic tumors (HOT), currently diagnosed as “unclassified” in the WHO classification. We identified 14 HOT by searching multiple institutional archives. Morphologic, immunohistochemical (IHC), molecular genetic, and molecular karyotyping studies were performed to investigate these tumors. The patients included 3 men and 11 women, with age range from 25 to 73 years (median 50, mean 49 years). Tumor size ranged from 1.5 to 7.0 cm in the greatest dimension (median 3, mean 3.4 cm). The tumors were all pT1 stage. Microscopically, they showed nested to solid growth, and focal tubulocystic architecture. The neoplastic cells were uniform with voluminous oncocytic cytoplasm. Prominent intracytoplasmic vacuoles were frequently seen, but no irregular (raisinoid) nuclei or perinuclear halos were present. All tumors demonstrated prominent nucleoli (WHO/ISUP grade 3 equivalent). Nine of 14 cases were positive for CD117 and cytokeratin (CK) 7 was either negative or only focally positive in of 6/14 cases. All tumors were positive for AE1-AE3, CK18, PAX 8, antimitochondrial antigen, and SDHB. Cathepsin K was positive in 13/14 cases and CD10 was positive in 12/13 cases. All cases were negative for TFE3, HMB45, Melan-A. No TFEB and TFE3 genes rearrangement was found in analyzable cases. By array CGH, complete chromosomal losses or gains were not found in any of the cases, and 3/9 cases showed absence of any abnormalities. Chromosomal losses were detected on chromosome 19 (4/9), 3 with losses of the short arm (p) and 1 with losses of both arms (p and q). Loss of chromosome 1 was found in 3/9 cases; gain of 5q was found in 1/9 cases. On molecular karyotyping, 3/3 evaluated cases showed loss of heterozygosity (LOH) on 16p11.2-11.1 and 2/3 cases showed LOH at 7q31.31. Copy number (CN) losses were found at 7q11.21 (3/3), Xp11.21 (3/3), Xp11.22-11.21 (3/3), and Xq24-25 (2/3). CN gains were found at 13q34 (2/3). Ten patients with available follow up information were alive and without disease progression, after a mean follow-up of 28 months (1 to 112 months). HOT is a tumor with unique morphology and its IHC profile appears mostly consistent. HOT should be considered as an emerging renal entity because it does not meet the diagnostic criteria for other recognized eosinophilic renal tumors, such as oncocytoma, chromophobe renal cell carcinoma (RCC), TFE3 and TFEB RCC, SDH-deficient RCC, and eosinophilic solid and cystic RCC.






Similar content being viewed by others
References
Hes O, Brunelli M, Michal M, Cossu Rocca P, Hora M, Chilosi M, Mina M, Boudova L, Menestrina F, Martignoni G (2006) Oncocytic papillary renal cell carcinoma: a clinicopathologic, immunohistochemical, ultrastructural, and interphase cytogenetic study of 12 cases. Ann Diagn Pathol 10:133–139. https://doi.org/10.1016/j.anndiagpath.2005.12.002
Lefevre M, Couturier J, Sibony M, Bazille C, Boyer K, Callard P, Vieillefond A, Allory Y (2005) Adult papillary renal tumor with oncocytic cells: clinicopathologic, immunohistochemical, and cytogenetic features of 10 cases. Am J Surg Pathol 29:1576–1581
Pavlovich CP, Walther MM, Eyler RA, Hewitt SM, Zbar B, Linehan WM, Merino MJ (2002) Renal tumors in the Birt-Hogg-Dube syndrome. Am J Surg Pathol 26:1542–1552
Petersson F, Gatalica Z, Grossmann P, Perez Montiel MD, Alvarado Cabrero I, Bulimbasic S, Swatek A, Straka L, Tichy T, Hora M, Kuroda N, Legendre B, Michal M, Hes O (2010) Sporadic hybrid oncocytic/chromophobe tumor of the kidney: a clinicopathologic, histomorphologic, immunohistochemical, ultrastructural, and molecular cytogenetic study of 14 cases. Virchows Archiv : Int J Pathol 456:355–365. https://doi.org/10.1007/s00428-010-0898-4
Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK, Zhou M, Argani P, Panel IRT (2013) The International Society of Urological Pathology (ISUP) Vancouver classification of renal neoplasia. Am J Surg Pathol 37:1469–1489. https://doi.org/10.1097/PAS.0b013e318299f2d1
Moch H, Humphrey PA, Ulbright TM, Reuter VE (2016) WHO classification of tumours of the urinary system and male genital organs IARC, Lyon, p 356
Williamson SR, Gadde R, Trpkov K, Hirsch MS, Srigley JR, Reuter VE, Cheng L, Kunju LP, Barod R, Rogers CG, Delahunt B, Hes O, Eble JN, Zhou M, McKenney JK, Martignoni G, Fleming S, Grignon DJ, Moch H, Gupta NS (2017) Diagnostic criteria for oncocytic renal neoplasms: a survey of urologic pathologists. Hum Pathol 63:149–156. https://doi.org/10.1016/j.humpath.2017.03.004
Steiner P, Andreasen S, Grossmann P, Hauer L, Vanecek T, Miesbauerova M, Santana T, Kiss K, Slouka D, Skalova A (2018) Prognostic significance of 1p36 locus deletion in adenoid cystic carcinoma of the salivary glands. Virchows Archiv : Int J Pathol. https://doi.org/10.1007/s00428-018-2349-6
Sperga M, Martinek P, Vanecek T, Grossmann P, Bauleth K, Perez-Montiel D, Alvarado-Cabrero I, Nevidovska K, Lietuvietis V, Hora M, Michal M, Petersson F, Kuroda N, Suster S, Branzovsky J, Hes O (2013) Chromophobe renal cell carcinoma—chromosomal aberration variability and its relation to Paner grading system: an array CGH and FISH analysis of 37 cases. Virchows Archiv: Int J Pathol 463:563–573. https://doi.org/10.1007/s00428-013-1457-6
Perrino CM, Grignon DJ, Williamson SR, Idrees MT, Eble JN, Cheng L (2018) Morphological spectrum of renal cell carcinoma, unclassified: an analysis of 136 cases. Histopathology 72:305–319. https://doi.org/10.1111/his.13362
Amin MB, Crotty TB, Tickoo SK, Farrow GM (1997) Renal oncocytoma: a reappraisal of morphologic features with clinicopathologic findings in 80 cases. Am J Surg Pathol 21:1–12
Trpkov K, Yilmaz A, Uzer D, Dishongh KM, Quick CM, Bismar TA, Gokden N (2010) Renal oncocytoma revisited: a clinicopathological study of 109 cases with emphasis on problematic diagnostic features. Histopathology 57:893–906. https://doi.org/10.1111/j.1365-2559.2010.03726.x
Foix MP, Dunatov A, Martinek P, Mundo EC, Suster S, Sperga M, Lopez JI, Ulamec M, Bulimbasic S, Montiel DP, Alaghehbandan R, Peckova K, Pivovarcikova K, Daum O, Rotterova P, Skenderi F, Prochazkova K, Dusek M, Hora M, Michal M, Hes O (2016) Morphological, immunohistochemical, and chromosomal analysis of multicystic chromophobe renal cell carcinoma, an architecturally unusual challenging variant. Virchows Archiv : Int J Pathol 469:669–678. https://doi.org/10.1007/s00428-016-2022-x
Hes O, Vanecek T, Perez-Montiel DM, Alvarado Cabrero I, Hora M, Suster S, Lamovec J, Curik R, Mandys V, Michal M (2005) Chromophobe renal cell carcinoma with microcystic and adenomatous arrangement and pigmentation--a diagnostic pitfall. Morphological, immunohistochemical, ultrastructural and molecular genetic report of 20 cases. Virchows Archiv : Int J Pathol 446:383–393. https://doi.org/10.1007/s00428-004-1187-x
Ohe C, Kuroda N, Keiko M, Tomoki K, Masatsugu M, Shun S, Shintaro T, Naoki H, Hes O, Michal M, Tadashi M, Yoshiko U (2014) CHromophobe renal cell carcinoma with neuroendocrine differentiation/morphology: a clinicopathological and genetic study of three cases. Human Pathol: Case Rep 1:31–39
Peckova K, Martinek P, Ohe C, Kuroda N, Bulimbasic S, Condom Mundo E, Perez Montiel D, Lopez JI, Daum O, Rotterova P, Kokoskova B, Dubova M, Pivovarcikova K, Bauleth K, Grossmann P, Hora M, Kalusova K, Davidson W, Slouka D, Sulc M, Buzrla P, Hynek M, Michal M, Hes O (2015) Chromophobe renal cell carcinoma with neuroendocrine and neuroendocrine-like features. Morphologic, immunohistochemical, ultrastructural, and array comparative genomic hybridization analysis of 18 cases and review of the literature. Ann Diagn Pathol 19:261–268. https://doi.org/10.1016/j.anndiagpath.2015.05.001
Delongchamps NB, Galmiche L, Eiss D, Rouach Y, Vogt B, Timsit MO, Vieillefond A, Mejean A (2009) Hybrid tumour 'oncocytoma-chromophobe renal cell carcinoma' of the kidney: a report of seven sporadic cases. BJU Int 103:1381–1384. https://doi.org/10.1111/j.1464-410X.2008.08263.x
Mai KT, Dhamanaskar P, Belanger E, Stinson WA (2005) Hybrid chromophobe renal cell neoplasm. Pathol Res Pract 201:385–389. https://doi.org/10.1016/j.prp.2005.03.008
Petersson F, Gatalica Z, Grossmann P, Montiel MDP, Cabrero IA, Bulimbasic S, Swatek A, Straka L, Tichy T, Hora M, Kuroda N, Legendre B, Michal M, Hes O (2010) Sporadic hybrid oncocytic/chromophobe tumor of the kidney: a clinicopathologic, histomorphologic, immunohistochemical, ultrastructural, and molecular cytogenetic study of 14 cases. Virchows Arch 456:355–365. https://doi.org/10.1007/s00428-010-0898-4
Hes O, Petersson F, Kuroda N, Hora M, Michal M (2013) Renal hybrid oncocytic/chromophobe tumors—a review. Histol Histopathol 28:1257–1264
Eble JN, Delahunt B (2018) Emerging entities in renal cell neoplasia: thyroid-like follicular renal cell carcinoma and multifocal oncocytoma-like tumours associated with oncocytosis. Pathology 50:24–36. https://doi.org/10.1016/j.pathol.2017.09.005
Li Y, Reuter VE, Matoso A, Netto GJ, Epstein JI, Argani P (2018) Re-evaluation of 33 'unclassified' eosinophilic renal cell carcinomas in young patients. Histopathology 72:588–600. https://doi.org/10.1111/his.13395
McKenney JK, Przybycin CG, Trpkov K, Magi-Galluzzi C (2018) Eosinophilic solid and cystic renal cell carcinomas have metastatic potential. Histopathology 72:1066–1067. https://doi.org/10.1111/his.13457
Trpkov K, Hes O, Bonert M, Lopez JI, Bonsib SM, Nesi G, Comperat E, Sibony M, Berney DM, Martinek P, Bulimbasic S, Suster S, Sangoi A, Yilmaz A, Higgins JP, Zhou M, Gill AJ, Przybycin CG, Magi-Galluzzi C, McKenney JK (2016) Eosinophilic, solid, and cystic renal cell carcinoma: clinicopathologic study of 16 unique, sporadic neoplasms occurring in women. Am J Surg Pathol 40:60–71. https://doi.org/10.1097/PAS.0000000000000508
Peckova K, Vanecek T, Martinek P, Spagnolo D, Kuroda N, Brunelli M, Vranic S, Djuricic S, Rotterova P, Daum O, Kokoskova B, Vesela P, Pivovarcikova K, Bauleth K, Dubova M, Kalusova K, Hora M, Michal M, Hes O (2014) Aggressive and nonaggressive translocation t(6;11) renal cell carcinoma: comparative study of 6 cases and review of the literature. Ann Diagn Pathol 18:351–357. https://doi.org/10.1016/j.anndiagpath.2014.10.002
Argani P, Ladanyi M (2006) The evolving story of renal translocation carcinomas. Am J Clin Pathol 126:332–334. https://doi.org/10.1309/EAEJTJGD5J4J3B4F
Argani P, Lae M, Hutchinson B, Reuter VE, Collins MH, Perentesis J, Tomaszewski JE, Brooks JS, Acs G, Bridge JA, Vargas SO, Davis IJ, Fisher DE, Ladanyi M (2005) Renal carcinomas with the t(6;11)(p21;q12): clinicopathologic features and demonstration of the specific alpha-TFEB gene fusion by immunohistochemistry, RT-PCR, and DNA PCR. Am J Surg Pathol 29:230–240
Martignoni G, Tardarico, R., Pea, M., Pecciarini, L., Gobbo, S. (2005) t6;11 renal cell tumor. A clinicopathological study of two cases in adults. Modern Pathol 18:155A
Argani P, Yonescu R, Morsberger L, Morris K, Netto GJ, Smith N, Gonzalez N, Illei PB, Ladanyi M, Griffin CA (2012) Molecular confirmation of t(6;11)(p21;q12) renal cell carcinoma in archival paraffin-embedded material using a break-apart TFEB FISH assay expands its clinicopathologic spectrum. Am J Surg Pathol 36:1516–1526. https://doi.org/10.1097/PAS.0b013e3182613d8f
Martignoni G, Bonetti F, Chilosi M, Brunelli M, Segala D, Amin MB, Argani P, Eble JN, Gobbo S, Pea M (2012) Cathepsin K expression in the spectrum of perivascular epithelioid cell (PEC) lesions of the kidney. Mod Pathol 25:100–111. https://doi.org/10.1038/modpathol.2011.136
Pitra T, Pivovarcikova K, Alaghehbandan R, Hes O (2017) Chromosomal numerical aberration pattern in papillary renal cell carcinoma: review article. Ann Diagn Pathol. https://doi.org/10.1016/j.anndiagpath.2017.11.004
Gill AJ, Pachter NS, Clarkson A, Tucker KM, Winship IM, Benn DE, Robinson BG, Clifton-Bligh RJ (2011) Renal tumors and hereditary pheochromocytoma-paraganglioma syndrome type 4. N Engl J Med 364:885–886. https://doi.org/10.1056/NEJMc1012357
Gill AJ, Pachter NS, Chou A, Young B, Clarkson A, Tucker KM, Winship IM, Earls P, Benn DE, Robinson BG, Fleming S, Clifton-Bligh RJ (2011) Renal tumors associated with germline SDHB mutation show distinctive morphology. Am J Surg Pathol 35:1578–1585. https://doi.org/10.1097/PAS.0b013e318227e7f4
Guo J, Tretiakova MS, Troxell ML, Osunkoya AO, Fadare O, Sangoi AR, Shen SS, Lopez-Beltran A, Mehra R, Heider A, Higgins JP, Harik LR, Leroy X, Gill AJ, Trpkov K, Campbell SC, Przybycin C, Magi-Galluzzi C, McKenney JK (2014) Tuberous sclerosis-associated renal cell carcinoma: a clinicopathologic study of 57 separate carcinomas in 18 patients. Am J Surg Pathol 38:1457–1467. https://doi.org/10.1097/PAS.0000000000000248
Trpkov K, Abou-Ouf H, Hes O, Lopez JI, Nesi G, Comperat E, Sibony M, Osunkoya AO, Zhou M, Gokden N, Leroy X, Berney DM, Werneck Cunha I, Musto ML, Athanazio DA, Yilmaz A, Donnelly B, Hyndman E, Gill AJ, McKenney JK, Bismar TA (2017) Eosinophilic solid and cystic renal cell carcinoma (ESC RCC): further morphologic and molecular characterization of ESC RCC as a distinct entity. Am J Surg Pathol 41:1299–1308. https://doi.org/10.1097/PAS.0000000000000838
Contributions
Huiying He and Ondrej Hes: revision of all cases, evaluation of immunohistochemistry. Kiril Trpkov and Ondrej Hes: design of study. Petr Martinek: molecular genetics. Ozlem Tanas Isikci, Kristyna Pivovarcikova: evaluation of immunohistochemistry. Anthony J Gill: evaluation of SDHB mutation and SDHB staining interpretation. Cristina Maggi-Galuzzi, Reza Alaghehbandan, Maria Tretiakova, Jose Ignacio Lopez, Sean Williamson, Delia Perez Montiel, Maris Sperga, Eva Comperat, Fadi Brimo, Michael Bonert, and Ali Yilmaz: case contribution, providing follow up data, and help with discussion. Kveta Michalova, David Slouka: follow up information, photodocumentation, Kristyna Prochazkova, Milan Hora: evaluation of clinical data. Michal Michal: discussion.
Funding
The study was supported by the Charles University Research Fund (project number Q39) and by the project Institutional Research Fund of University Hospital Plzen (FN 00669806).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Study design has been approved by local ethical committee (Charles University, Medical School Plzen) LEK FN Plzeň.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
He, H., Trpkov, K., Martinek, P. et al. “High-grade oncocytic renal tumor”: morphologic, immunohistochemical, and molecular genetic study of 14 cases. Virchows Arch 473, 725–738 (2018). https://doi.org/10.1007/s00428-018-2456-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2456-4