Abstract
Purpose
To evaluate the incidence, risk factors, management options, and outcomes of portal vein thrombosis following major hepatectomy for perihilar cholangiocarcinoma.
Methods
A total of 177 perihilar cholangiocarcinoma patients who (1) underwent major hepatectomy and (2) underwent investigating the portal vein morphology, which was measured by rotating the reconstructed three-dimensional images after facilitating bone removal using Aquarius iNtuition workstation between 2002 and 2018, were included. Risk factors were evaluated using the Kaplan-Meier method and Cox proportional hazard models.
Results
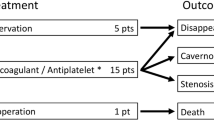
Six patients developed portal vein thrombosis (3.4%) within a median time of 6.5 (range 0–22) days. Portal vein and hepatic artery resection were performed in 30% and 6% patients, respectively. A significant difference in the probability of the occurrence of portal vein thrombosis (PV) within 30 days was found among patients with portal vein resection, a postoperative portal vein angle < 100°, remnant portal vein diameter < 5.77 mm, main portal vein diameter > 13.4 mm, and blood loss (log-rank test, p = 0.003, p = 0.06, p < 0.0001, p = 0.01, and p = 0.03, respectively). Decreasing the portal vein angle and narrowing of the remnant PV diameter remained significant predictors on multivariate analysis (p = 0.027 and 0.002, respectively). Reoperation with thrombectomy was performed in four patients, and the other two patients were successfully treated with anticoagulants. All six patients subsequently recovered and were discharged between 25 and 70 days postoperatively.
Conclusion
Narrowing of the remnant portal vein diameter and a decreased portal vein angle after major hepatectomy for perihilar cholangiocarcinoma are significant independent risk factors for postoperative portal vein thrombosis.

Similar content being viewed by others
References
Nagino M, Ebata T, Yokoyama Y et al (2013) Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg 258:129–140. https://doi.org/10.1097/SLA.0b013e3182708b57
Molina V, Sampson J, Ferrer J et al (2017) Surgical treatment of perihilar cholangiocarcinoma: early results of en bloc portal vein resection. Langenbeck's Arch Surg 402:95–104. https://doi.org/10.1007/s00423-016-1542-9
Lee SG, Song GW, Hwang S et al (2010) Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci 17:476–489. https://doi.org/10.1007/s00534-009-0204-5
Higuchi R, Ota T, Yazawa T et al (2016) Improved surgical outcomes for hilar cholangiocarcinoma: changes in surgical procedures and related outcomes based on 40 years of experience at a single institution. Surg Today 46:74–83. https://doi.org/10.1007/s00595-015-1119-1
Ebata T, Ito T, Yokoyama Y et al (2014) Surgical technique of hepatectomy combined with simultaneous resection of hepatic artery and portal vein for perihilar cholangiocarcinoma (with video). J Hepatobiliary Pancreat Sci 21(8):E57–61. https://doi.org/10.1002/jhbp.121
Farid SG, White A, Khan N et al (2016) Clinical outcomes of left hepatic trisectionectomy for hepatobiliary malignancy. Br J Surg 103:249–256. https://doi.org/10.1002/bjs.10059
Lee Y, Choi D, Han S et al (2018) Comparison analysis of left-side versus right-side resection in bismuth type III hilar cholangiocarcinoma. Ann Hepato-Biliary-Pancreatic Surg 22:350. https://doi.org/10.14701/ahbps.2018.22.4.350
Higuchi R, Yazawa T, Uemura S et al (2019) Surgical outcomes for perihilar cholangiocarcinoma with vascular invasion. J Gastrointest Surg 23:1443–1453. https://doi.org/10.1007/s11605-018-3948-x
Ebata T, Mizuno T, Yokoyama Y et al (2018) Surgical resection for Bismuth type IV perihilar cholangiocarcinoma. Br J Surg 105:829–838. https://doi.org/10.1002/bjs.10556
Shimizu H, Kimura F, Yoshidome H et al (2010) Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg 251:281–286. https://doi.org/10.1097/SLA.0b013e3181be0085
Kondo S, Katoh H, Hirano S et al (2002) Vedge resection of the portal bifurcation concomitant with left hepatectomy plus biliary reconstruction for hepatobiliary cancer. J Hepato-Biliary-Pancreat Surg 9:603–606. https://doi.org/10.1007/s005340200081
Kuboki S, Shimizu H, Ohtsuka M et al (2015) Incidence, risk factors, and management options for portal vein thrombosis after hepatectomy: a 14-year, single-center experience. Am J Surg 210:878–885.e2. https://doi.org/10.1016/j.amjsurg.2014.11.021
Yoshiya S, Shirabe K, Nakagawara H et al (2014) Portal vein thrombosis after hepatectomy. World J Surg 38:1491–1497. https://doi.org/10.1007/s00268-013-2440-8
Han JH, Kim DS, Yu YD et al (2019) Analysis of risk factors for portal vein thrombosis after liver resection. Ann Surg Treat Res 96:230–236. https://doi.org/10.4174/astr.2019.96.5.230
Blasi A, Molina V, Sanchez-Cabús S et al (2018) Prediction of thromboembolic complications after liver resection for cholangiocarcinoma: is there a place for thromboelastometry? Blood Coagul Fibrinolysis 29:61–66. https://doi.org/10.1097/MBC.0000000000000672
Narita M, Matsusue R, Hata H et al (2014) Precaution against postoperative venous complications after major hepatectomy using the pedicled omental transposition flap: report of two cases. Int J Surg Case Rep 5:646–651. https://doi.org/10.1016/j.ijscr.2014.07.019
Thomas RM, Ahmad SA (2010) Management of acute post-operative portal venous thrombosis. J Gastrointest Surg 14:570–577. https://doi.org/10.1007/s11605-009-0967-7
Smoot RL, Christein JD, Farnell MB (2006) Durability of portal venous reconstruction following resection during pancreaticoduodenectomy. J Gastrointest Surg 10:1371–1375. https://doi.org/10.1016/j.gassur.2006.09.001
Ansari D, Ansorge C, Andrén-Sandberg Å et al (2013) Portal venous system thrombosis after pancreatic resection. World J Surg 37:179–184. https://doi.org/10.1007/s00268-012-1777-8
Miyazaki M, Yoshitomi H, Miyakawa S et al (2015) Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. J Hepatobiliary Pancreat Sci 22:249–273. https://doi.org/10.1002/jhbp.233
Chaudhary RJ, Higuchi R, Nagino M et al (2019) A survey of preoperative management protocol for perihilar cholangiocarcinoma at 10 Japanese high-volume centers with a combined experience of 2778 cases. J Hepatobiliary Pancreat Sci 26:490–502. https://doi.org/10.1002/jhbp.668
Uchida T, Yamamoto Y, Sugiura T et al (2019) Prediction of portal vein thrombosis following hepatectomy for perihilar cholangiocarcinoma: efficacy of postoperative portal vein diameter ratio and angle. Anticancer Res 39:5019–5026. https://doi.org/10.21873/anticanres.13692
Kato A, Shimizu H, Ohtsuka M et al (2017) Portal vein stent placement for the treatment of postoperative portal vein stenosis: long-term success and factor associated with stent failure. BMC Surg 17:1–6. https://doi.org/10.1186/s12893-017-0209-y
Miyazaki M, Shimizu H, Ohtuka M et al (2017) Portal vein thrombosis after reconstruction in 270 consecutive patients with portal vein resections in hepatopancreatobiliary (HPB) surgery. Am J Surg 214:74–79. https://doi.org/10.1016/j.amjsurg.2016.12.008
Ponziani FR, Zocco MA, Campanale C et al (2010) Portal vein thrombosis: Insight into physiopathology, diagnosis, and treatment. World J Gastroenterol 16:143–155. https://doi.org/10.3748/wjg.v16.i2.143
Imamura N, Nanashima A, Tsuchimochi Y et al (2018) Intrahepatic portal vein thrombosis due to postoperative biliary obstruction successfully treated by a partial thrombectomy combined with thrombolytic drug therapy. Int J Surg Case Rep 42:20–23. https://doi.org/10.1016/j.ijscr.2017.11.047
Mueller AR, Platz K-P, Kremer B (2004) Early postoperative complications following liver transplantation. Best Pract Res Clin Gastroenterol 18:881–900. https://doi.org/10.1016/j.bpg.2004.07.004
Kawasaki TY, Moriyasu F, Ozawa K et al (1991) Changes in portal blood flow consequent to partial hepatectomy: Doppler estimation. Radiology 180:373–377
Woo DH, LaBerge JM, Gordon RL et al (2007) Management of portal venous complications after liver transplantation. Tech Vasc Interv Radiol 10:233–239. https://doi.org/10.1053/j.tvir.2007.09.017
Cao G, Ko GY, Sung KB et al (2013) Treatment of postoperative main portal vein and superior mesenteric vein thrombosis with balloon angioplasty and/or stent placement. Acta Radiol 54:526–532. https://doi.org/10.1177/0284185113475917
Yamashita YI, Bekki Y, Imai D et al (2014) Efficacy of postoperative anticoagulation therapy with enoxaparin for portal vein thrombosis after hepatic resection in patients with liver cancer. Thromb Res 134:826–831. https://doi.org/10.1016/j.thromres.2014.07.038
Klempnauer J, GROTHUES F, BEKTAS H et al (1997) Results of portal thrombectomy and splanchnic thrombolysis for the surgical management of acute mesentericoportal thrombosis. Br J Surg 84:129–132
Malkowski P, Pawlak J, Michalowicz B et al (2003) Thrombolytic treatment of portal thrombosis. Hepatogastroenterology 50:2098–2100
Hollingshead M, Burke CT, Mauro MA et al (2005) Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol 16:651–661. https://doi.org/10.1097/01.RVI.0000156265.79960.86
Cho CW, Park YJ, Kim YW et al (2015) Follow-up results of acute portal and splenic vein thrombosis with or without anticoagulation therapy after hepatobiliary and pancreatic surgery. Ann Surg Treat Res 88:208–214. https://doi.org/10.4174/astr.2015.88.4.208
Kyoden Y, Tamura S, Sugawara Y et al (2008) Portal vein complications after adult-to-adult living donor liver transplantation. Transpl Int 21:1136–1144. https://doi.org/10.1111/j.1432-2277.2008.00752.x
Sobhonslidsuk A, Reddy KR (2002) Portal vein thrombosis: a concise review. Am J Gastroenterol 97:535–541. https://doi.org/10.1111/j.1572-0241.2002.05527.x
Trebicka J, Strassburg CP (2014) Etiology and complications of portal vein thrombosis. Visz Gastrointest Med Surg 30:375–380
Condat B, Pessione F, Hillaire S et al (2001) Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy. Gastroenterology 120:490–497. https://doi.org/10.1053/gast.2001.21209
Moon D-B, Lee S-G, Ahn C et al (2007) Application of intraoperative cine-portogram to detect spontaneous portosystemic collaterals missed by intraoperative Doppler exam in adult living donor liver transplantation. Liver Transpl 13:1279–1284. https://doi.org/10.1002/lt.21252
Uchida H, Sakamoto S, Shimizu S et al (2020) Efficacy of intraoperative cine-portogram for complicated portal vein reconstruction in pediatric living donor liver transplantation. Pediatr Transplant e13835. https://doi.org/10.1111/petr.13835
Acknowledgments
The superb secretarial assistance of J. Hunke is gratefully acknowledged.
Funding
This work was supported by the JSPS KAKENHI (grant number 18K08632).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: R.H. Acquisition of data: R.H., MT.C., S.M., T.Y., S.U., W.I., Y.M., and M.Y. Analysis and interpretation of data: R.H. and MT.C. Analysis of pathology: T.F. Statistics advice: Y.S. Draft and critical analysis: MT.C., R.H., and M.Y.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Institutional Review Board of Tokyo Women’s Medical University (acceptance number 4328-R2).
Consent to participate
The requirement to obtain written informed consent from each patient was waived due to the study’s retrospective design.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, MT., Higuchi, R., Yazawa, T. et al. Narrowing of the remnant portal vein diameter and decreased portal vein angle are risk factors for portal vein thrombosis after perihilar cholangiocarcinoma surgery. Langenbecks Arch Surg 406, 1511–1519 (2021). https://doi.org/10.1007/s00423-020-02044-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-02044-1