Abstract
Objective
To compare natural orifice specimen extraction surgery (NOSES) and conventional laparoscopic (LAP) surgery in treating colorectal cancer.
Methods
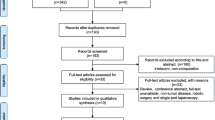
The present authors conducted a systematic search in the PubMed, EMBASE, and Cochrane databases for randomized controlled trials (RCTs), prospective nonrandomized studies, and retrospective studies up to May 2019. We used postoperative complications as the main endpoints, and used hospital stay, time to first flatus, operative time, postoperative pain, cosmetic result, wound infections, and oncological outcomes as the secondary endpoints. Subgroup analyses were conducted according to the different specimen extraction sites (transanal and transvaginal). A sensitivity analysis was carried out to evaluate the reliability of the outcomes. RevMan5.3 software was used for statistical analysis.
Result
Twelve studies (one RCT, ten retrospective studies, and one prospective nonrandomized study) involving a total of 1437 patients (NOSES group 665 patients and LAP surgery group 772 patients) were included. Meta-analysis showed that compared with LAP surgery, NOSES resulted in a shorter hospital stay (WMD = −0.79 days; 95% CI −1.17 to −0.42; P < 0.001; P = 0.02), a shorter time to first flatus (WMD = −0.58 days; 95% CI −0.75 to −0.40; P < 0.001), less postoperative pain (WMD = −1.51; 95% CI −1.99 to −1.04; P < 0.001), a better cosmetic result (WMD = 1.37; 95% CI 0.59 to 2.14; P < 0.001), and fewer wound infections (OR = 0.13; 95% CI 0.05 to 0.35; P < 0.001) and postoperative complications (OR = 0.48; 95% CI 0.36 to 0.65; P < 0.001). Oncological outcomes did not differ between the two groups, while the operative time (WMD = 13.95 min; 95% CI 4.55 to 23.35; P = 0.004) was longer in the NOSES group.
Conclusion
The present systematic meta-analysis is an attempt to assess the impact of NOSES, namely, its oncological outcomes and surgical safety in colorectal cancer patients. Pooled comparisons revealed that NOSES was superior to LAP surgery in terms of postoperative morbidity, postoperative pain, hospital stay, the time to first flatus, cosmetic results, and wound infections; however, NOSES was associated with a longer operative time. Considering the abovementioned limitations and the very low level of evidence of the comparisons, further RCTs are required to verify the results of our study.























Similar content being viewed by others
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ, Group CcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Kim W, Kim H-H, Han S-U, Kim M-C, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang H-K, Park DJ (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer. Ann Surg 263(1):28–35
Sakuramoto S, Yamashita K, Kikuchi S, Futawatari N, Katada N, Watanabe M, Okutomi T, Wang G, Bax L (2013) Laparoscopy versus open distal gastrectomy by expert surgeons for early gastric cancer in Japanese patients: short-term clinical outcomes of a randomized clinical trial. Surg Endosc 27(5):1695–1705
Romy S, Eisenring M-C, Bettschart V, Petignat C, Francioli P, Troillet N (2008) Laparoscope use and surgical site infections in digestive surgery. Ann Surg 247(4):627–632
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22(12):2596–2600
Winslow E, Fleshman J, Birnbaum E, Brunt L (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc Other Interv Tech 16(10):1420–1425
Wang Z, Zhang XM, Zhou HT, Liang JW, Zhou ZX (2014) New technique of intracorporeal anastomosis and transvaginal specimen extraction for laparoscopic sigmoid colectomy. Asian Pac J Cancer Prev 15(16):6733–6736. https://doi.org/10.7314/apjcp.2014.15.16.6733
Franklin ME Jr, Liang S, Russek K (2013) Integration of transanal specimen extraction into laparoscopic anterior resection with total mesorectal excision for rectal cancer: a consecutive series of 179 patients. Surg Endosc 27(1):127–132. https://doi.org/10.1007/s00464-012-2440-z
Cheung TP, Cheung HY, Ng LW, Chung CC, Li MK (2012) Hybrid NOTES colectomy for right-sided colonic tumors. Asian J Endosc Surg 5(1):46–49. https://doi.org/10.1111/j.1758-5910.2011.00106.x
Wolthuis AM, van Overstraeten AD, Fieuws S, Boon K, D'Hoore A (2015) Standardized laparoscopic NOSE-colectomy is feasible with low morbidity. Surg Endosc Other Interv Tech 29(5):1167–1173. https://doi.org/10.1007/s00464-014-3784-3
Franklin ME Jr, Liang S, Russek K (2013) Natural orifice specimen extraction in laparoscopic colorectal surgery: transanal and transvaginal approaches. Tech Coloproctol 17(Suppl 1):S63–S67. https://doi.org/10.1007/s10151-012-0938-y
Ngu J, Wong ASY (2016) Transanal natural orifice specimen extraction in colorectal surgery: bacteriological and oncological concerns. ANZ J Surg 86(4):299–302
Wolthuis AM, van Overstraeten AB, D’Hoore A (2014) Laparoscopic natural orifice specimen extraction-colectomy: a systematic review. World J Gastroenterol: WJG 20(36):12981–12992
Leroy J, Costantino F, Cahill R, D'agostino J, Morales A, Mutter D, Marescaux J (2011) Laparoscopic resection with transanal specimen extraction for sigmoid diverticulitis. Br J Surg 98(9):1327–1334
Ma B, Huang XZ, Gao P, Zhao JH, Song YX, Sun JX, Chen XW, Wang ZN (2015) Laparoscopic resection with natural orifice specimen extraction versus conventional laparoscopy for colorectal disease: a meta-analysis. Int J Color Dis 30(11):1479–1488. https://doi.org/10.1007/s00384-015-2337-0
David Moher P, Alessandro Liberati M, Jennifer Tetzlaff B, Douglas G, Altman D, Group* atP (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med
Awad ZT, Griffin R (2014) Laparoscopic right hemicolectomy: a comparison of natural orifice versus transabdominal specimen extraction. Surg Endosc Other Interv Tech 28(10):2871–2876. https://doi.org/10.1007/s00464-014-3540-8
Denost Q, Adam JP, Pontallier A, Celerier B, Laurent C, Rullier E (2015) Laparoscopic total mesorectal excision with coloanal anastomosis for rectal cancer. Orig Artic 261(1):138–143. https://doi.org/10.1097/sla.0000000000000855
Hisada M, Katsumata K, Ishizaki T, Enomoto M, Matsudo T, Kasuya K, Tsuchida A (2014) Complete laparoscopic resection of the rectum using natural orifice specimen extraction. World J Gastroenterol 20(44):16707–16713. https://doi.org/10.3748/wjg.v20.i44.16707
Kim HJ, Choi GS, Park JS, Park SY, Ryuk JP, Yoon SH (2014) Transvaginal specimen extraction versus conventional minilaparotomy after laparoscopic anterior resection for colorectal cancer: mid-term results of a case-matched study. Surg Endosc 28(8):2342–2348. https://doi.org/10.1007/s00464-014-3466-1
Park JS, Choi GS, Kim HJ, Park SY, Jun SH (2011) Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg 98(5):710–715. https://doi.org/10.1002/bjs.7419
Saurabh B, Chang S-C, Ke T-W, Huang Y-C, Kato T, Wang H-M, Tzu-Liang Chen W, Fingerhut A (2017) Natural orifice specimen extraction with single stapling colorectal anastomosis for laparoscopic anterior resection: feasibility, outcomes, and technical considerations. Dis Colon Rectum 60(1):43–50
Xingmao Z, Haitao Z, Jianwei L, Huirong H, Junjie H, Zhixiang Z (2014) Totally laparoscopic resection with natural orifice specimen extraction (NOSE) has more advantages comparing with laparoscopic-assisted resection for selected patients with sigmoid colon or rectal cancer. Orig Artic 29(9):1119–1124. https://doi.org/10.1007/s00384-014-1950-7
Ng HI, Sun WQ, Zhao XM, Jin L, Shen XX, Zhang ZT, Wang J (2018) Outcomes of trans-anal natural orifice specimen extraction combined with laparoscopic anterior resection for sigmoid and rectal carcinoma: an observational study. Med (U S) 97(38):e12347. https://doi.org/10.1097/MD.0000000000012347
Park JS, Kang H, Park SY, Kim HJ, Lee IT, Choi GS (2018) Long-term outcomes after natural orifice specimen extraction versus conventional laparoscopy-assisted surgery for rectal cancer: a matched case-control study. Ann Surg Treat Res 94(1):26–35. https://doi.org/10.4174/astr.2018.94.1.26
Hu JH, Li XW, Wang CY, Zhang JJ, Ge Z, Li BH, Lin XH (2019) Short-term efficacy of natural orifice specimen extraction surgery for low rectal cancer. World J Clin Cases 7(2):122–129. https://doi.org/10.12998/wjcc.v7.i2.122
Wang RC, Wei ZW, Liu QL, Li WF, Xiao LB, Hang FHH, Yang SB (2018) Transanal versus transabdominal specimen extraction in laparoscopic rectal cancer surgery: a retrospective analysis from China. Videosurg Miniinvasive Tech 14(2):203–209. https://doi.org/10.5114/wiitm.2018.79529
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327(7414):557–560
Petitti DB (2001) Approaches to heterogeneity in meta-analysis. Stat Med 20(23):3625–3633
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Group GW (2004) Grading quality of evidence and strength of recommendations. BMJ: Br Med J 328(7454):1490
Leung ALH, Cheung HYS, Fok BKL, Chung CCC, Li MKW, Tang CN (2013) Prospective randomized trial of hybrid NOTES colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors. World J Surg 37(11):2678–2682. https://doi.org/10.1007/s00268-013-2163-x
Steinemann DC, Müller PC, Probst P, Schwarz AC, Büchler MW, Müller-Stich BP, Linke GR (2017) Meta-analysis of hybrid natural-orifice transluminal endoscopic surgery versus laparoscopic surgery. Br J Surg 104:977–989
Wolthuis AM, Meuleman C, Tomassetti C, D'Hooghe T, D'Hoore A (2014) How do patients score cosmesis after laparoscopic NOSE-colectomy? Color Dis 17(6)
Kantsevoy SV (2008) Infection prevention in NOTES. Gastrointest Endosc Clin N Am 18(2):291–296
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235(4):449–457
Leung ALH, Cheung HYS, Li MKW (2014) Advances in laparoscopic colorectal surgery: a review on NOTES and transanal extraction of specimen. Asian J Endosc Surg 7(1):11–16
Morlote DM, Alexis JB (2016) Is the routine microscopic examination of proximal and distal resection margins in colorectal cancer surgery justified? Ann Diagn Pathol S1092913416301058
Wolthuis A, Fieuws S, Van Den Bosch A, de Buck van Overstraeten A, D'Hoore A (2015) Randomized clinical trial of laparoscopic colectomy with or without natural-orifice specimen extraction. Br J Surg 102(6):630–637
Guan X, Liu Z, Longo A, Cai J-C, Tzu-Liang Chen W, Chen L-C, Chun H-K, Manuel da Costa Pereira J, Efetov S, Escalante R (2019) International consensus on natural orifice specimen extraction surgery (NOSES) for colorectal cancer. Gastroenterol Rep 7(1):24–31
Izquierdo KM, Unal E, Marks JH (2018) Natural orifice specimen extraction in colorectal surgery: patient selection and perspectives. Clin Exp Gastroenterol 11:265–279
(2015) Laparoscopic resection with natural orifice specimen extraction versus conventional laparoscopy for colorectal disease: a meta-analysis. Int J Color Dis 30(11):1479–1488
Acknowledgements
Not applicable.
Funding
This study was supported by the Fujian Province teaching reform project (grant no. FBJG20190063), the Training Project of Young Talents in the Health System of Fujian Province (grant no. 2019-2-20), and the Fujian Medical University Key teaching reform project (grant no. Y19001).
Author information
Authors and Affiliations
Contributions
SQC designed the study, obtained funding, analyzed the data, and revised the manuscript. JJL drafted the manuscript and supervised the study. SQC was a supporter of the funding (grant no. FBJG20190063) and participating in the drafting and subsequent revision of the manuscript. SYL, ZHC, and BQZ collected and analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, J., Lin, S., Chen, Z. et al. Meta-analysis of natural orifice specimen extraction versus conventional laparoscopy for colorectal cancer. Langenbecks Arch Surg 406, 283–299 (2021). https://doi.org/10.1007/s00423-020-01934-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01934-8