Abstract
Purpose
Aging impairs the autonomic balance reducing the vagal and increasing the sympathetic components of heart rate variability (HRV) and this could be associated with a decline in physical capacity. Inspiratory muscle training (IMT) is a possible tool to attenuate this physical capacity decline in older women. The aim of this study was to investigate the influence of IMT in the older women on physical capacity and autonomic cardiac modulation at rest and post exercise.
Methods
20 female participants 60–72 years old were randomly allocated in two groups. One group underwent IMT set at 50% of maximum inspiratory pressure (MIP), every day for 4 weeks (IMT-group). The placebo group performed the same training procedure but with a minimal resistance (5% MIP; PLA-group). Every week, the IMT load was readjusted and the HRV evaluated at rest. The six-minute walk test (6MWT) was performed once pre and post IMT-intervention. The IMT-group and PLA-group performed the same test and intervention procedures.
Results
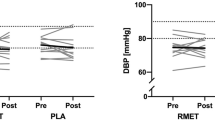
After a 5 weeks intervention, the MIP had significantly improved in the IMT-group but not in the PLA-group (p < 0.01; es = 1.17). The high frequency power of the HRV spectrum had already improved by the second week (p < 0.01; es = 1.13) and remained elevated until the last week of intervention (p < 0.01; es = 1.43). The same positive results were described in 6MWT distance (p = 0.04; es = 0.39) and the change (∆) of heart rate recovery (HRR) from 1 min (p = 0.02; es = 0.68).
Conclusion
IMT increases HRV, improves 6MWT distance and HRR.



Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- BP:
-
Blood pressure
- es:
-
Effect size
- FVC:
-
Forced vital capacity
- FEV1:
-
Forced expiratory volume in 1 s
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- HRR:
-
Post-exercise heart rate recovery
- HF:
-
High frequency domain
- IMT:
-
Inspiratory muscle training
- LF:
-
Low frequency domain
- LF/HF:
-
Autonomic balance
- MIP:
-
Maximal inspiratory pressure
- HRmax :
-
Maximal heart rate
- PLA:
-
Placebo
- PF:
-
Peak flow
- PFT:
-
Pulmonary function test
- 6MWT:
-
Six-minute walking test
- Δ:
-
Delta
References
Aznar-Lain S, Webster AL, Cañete S, San Juan AF, López Mojares LM, Lucia A, Chicharro JL (2007) Effects of inspiratory muscle training on exercise capacity and spontaneous physical activity in elderly subjects: a randomized controlled pilot trial. Int J Sports Med 28(12):1025–1029
Bernardi L, Porta C, Gabutti A, Spicuzza L, Sleight P (2001) Modulatory effects of respiration. Auton Neurosci 90(1–2):47–56. https://doi.org/10.1016/S1566-0702(01)00267-3
Cooper PJ, Kohl P (2005). Species—and preparation-dependence of stretch effects on sino-atrial node pacemaking. Ann N Y Acad Sci 1047:324–335
Darr KC, Bassett DR, Morgan BJ, Thomas DP (1988) Effect of age and training status on heart rate recovery after peak exercise. Am J Physiol 254(2Pt2):H340–H343
de Abreu R, Rehder-Santosa P, Minatel V, dos Santos G, Catai A (2017). Effects of inspiratory muscle training on cardiovascular autonomic control: a systematic review. Auton Neurosci. https://doi.org/10.1016/j.autneu.2017.09.002 (Article in press)
Dick TE, Mims JR, Hsieh YH, Morris KF, Wehrwein EA (2014) Increased cardio-respiratory coupling evoked by slow deep breathing can persist in normal humans. Respir Physiol Neurobiol 204:99–111
Duarte A, Soares PP, Pescatello L, Farinatti P (2015) Aerobic training improves vagal reactivation regardless of resting vagal control. Med Sci Sports Exerc 47(6):1159–1167
Elstad M, Walløe L (2015) Heart rate variability and stroke volume variability to detect central hypovolemia during spontaneous breathing and supported ventilation in young, healthy volunteers. Physiol Meas 36(4):671–681
Evans J, Whitelaw W (2009) The assessment of maximal respiratory mouth pressures in adults. Respir Care 54(10):1348–1359
Farinatti PTV, Soares PPS (2009) Cardiac output and oxygen uptake relationship during physical effort in men and women over 60 years old. Eur J Appl Physiol 107(6):625–631
Feriani DJ, Coelho-júnior HJ, Scapini KB, Moraes OA, De Mostarda C (2017) Effects of inspiratory muscle exercise in the pulmonary function, autonomic modulation and hemodynamic variables in older women with metabolic syndrome. J Exerc Rehabil 13(2):218–226
Ferreira JB, Plentz RDM, Stein C, Casali KR, Arena R, Lago PD (2013) Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J Cardiol 166(1):61–67
Fried LP, Tangen CM, Walston J et al (2001) frailty in older adults: evidence for a phenotype. J Gerontol Med Sci 56(3):M146–M156
Gibson GJ, Whitelaw W, Siafakas N et al (2002) ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 166(4):518–624
Greig CA, Young A, Skelton DA, Pippet E, Butler FMM, Mahmud SM (1994) Exercise studies with elderly volunteers. Age Ageing 23:185–189. https://doi.org/10.1093/ageing/23.3.185
Held HE, Pendergast DR (2014) The effects of respiratory muscle training on respiratory mechanics and energy cost. Respir Physiol Neurobiol 200:7–17
Hopkins WG, Marshall SW, Batterham AM, Hanin J (2009) Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc 41(1):3–13
Huang C, Yang G, Wu Y, Lee C (2011) Comparison of inspiratory muscle strength training effects between older subjects with and without chronic obstructive pulmonary disease. J Formos Med Assoc 110(8):518–526. https://doi.org/10.1016/S0929-6646(11)60078-8
Huikuri HV, Ma TH, Airaksinen KEJ, Seppa T, Puukka P, Ra IJ (1998) Power-law relationship of heart rate variability as a predictor of mortality in the elderly. Circulation 97:2031–2036. https://doi.org/10.1161/01.CIR.97.20.2031
Illi S, Held U, Frank I, Spengler CM (2012) Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sports Med 42(8):707–724
Janssens JP (2005) Aging of the respiratory system: impact on pulmonary function tests and adaptation to exertion. Clin Chest Med 26(3):469–484
Johnson CD, Roe S, Tansey EA (2013) Investigating autonomic control of the cardiovascular system: a battery of simple tests. Adv Physiol Educ 37(4):401–404. https://doi.org/10.1152/advan.00065.2013
Joseph CN, Porta C, Casucci G, Casiraghi N, Maffeis M, Rossi M, Bernardi L (2005) Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension 46(4):714–718. https://doi.org/10.1161/01.HYP.0000179581.68566.7d
Laitinen T, Niskanen L, Geelen G, Länsimies E, Hartikainen J (2004) Age dependency of cardiovascular autonomic responses to head-up tilt in healthy subjects. J Appl Physiol 96(6):2333–2340
Malik M, Bigger JT, Camm AJ, Kleiger RE, Malliani A, Moss AJ, Schwartz PJ (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065
McConnell AK (2012) Crosstalk opposing view: respiratory muscles training does improve exercise tolerance. J Physiol 590(15):3397–3338
Mcconnell AK, Lomax M (2006) The influence of inspiratory muscle work history and specific inspiratory muscle training upon human limb muscle fatigue. J Physiol 577:445–457. https://doi.org/10.1113/jphysiol.2006.117614
Miller MR et al (2005) ATS/ERS Task force: standardisation of lung function testing: Standardisation of spirometry. Eur Respir J 26:319–338
Mills DE, Johnson MA, Barnett YA, Smith WHT, Sharpe GR (2015) The effects of inspiratory muscle training in older adults. Med Sci Sports Exerc 47(4):691–697. https://doi.org/10.1249/MSS.0000000000000474
Montano N, Porta A, Cogliati C, Cosantino G, Tobaldini E, Casali K, Iellamo F (2009) Heart rate variability explored in the frequency domain: a tool to investigate the link between heart and behavior. Neurosci Biobehav Rev 33(2):71–80
Myers J, Hadley D, Oswald U, Bruner F, Kottman W, Hsu L, Dubach P (2007) Effects of exercise training on heart rate recovery in patients with chronic heart failure. Am Heart J 153:1056–1063. https://doi.org/10.1016/j.ahj.2007.02.038
Patel MS, Hart N, Polkey MI (2012) CrossTalk proposal: training the respiratory muscles does not improve exercise tolerance. J Physiol 590(15):3393–3395
Pereira C, Duarte A, Gimenez A, Soares MR (2014) Comparison between reference values for FVC, FEV1, and FEV1/FVC ratio in White adults in Brazil and those suggested by the Global Lung Function Initiative 2012. J Bras Pneumol 40(4):397–402
Piha SJ (1993) Age related diminution of the cardiovascular autonomic responses: diagnostic problems in the elderly. Clin Physio1 13(5):507–517
Reis MS, Arena R, Archiza B, De Toledo CF, Catai AM, Borghi-Silva A (2014) Deep breathing heart rate variability is associated with inspiratory muscle weakness in chronic heart failure. Physiother Res Int 19(1):16–24. https://doi.org/10.1002/pri.1552
Santaella DF, Devesa CRS, Rojo MR et al (2011) Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. BMJ Open 1(1):e000085–e000085
Souza H, Rocha T, Pessoa M et al (2014) Effects of inspiratory muscle training in elderly women on respiratory muscle strength, diaphragm thickness and mobility. J Gerontol A Biol Sci Med Sci 69(12):1545–1553. https://doi.org/10.1093/gerona/glu182
Troosters T, Gosselink R, Decramer M (1999) Six minute walking distance in healthy elderly subjects. Eur Respir J 2:270–274
Turner LA, Tecklenburg-lund SL, Chapman RF, Stager JM, Wilhite DP, Mickleborough TD (2012). Inspiratory muscle training lowers the oxygen cost of voluntary hyperpnea. J Appl Physiol 127–134. https://doi.org/10.1152/japplphysiol.00954.2011
Watsford M, Murphy A (2008) The effects of respiratory-muscle training on exercise in older women. J Aging Phys Act 16:245–260
Witt JD, Guenette JA, Rupert JL, McKenzie DC, Sheel AW (2007) Inspiratory muscle training attenuates the human respiratory muscle metaboreflex. J Physiol 584(Pt 3):1019–1028. https://doi.org/10.1113/jphysiol.2007.140855
Yanagisawa S, Miki K, Yasuda N, Hirai T, Suzuki N, Tanaka T (2011). The prognostic value of treadmill exercise testing in very elderly patients: heart rate recovery as a predictor of mortality in octogenarians. Europace. https://doi.org/10.1093/europace/euq422
Acknowledgements
This work was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação Carlos Chagas de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ/ E-26/110.079/2013).
Author information
Authors and Affiliations
Contributions
GDR, TRG, and PPSS conceived and designed research. GDR and TRG conducted experiments. GDR, JLG, TRG and PPSS analyzed the data. GDR, JLG, TRG, and PPSS wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Additional information
Communicated by Susan Hopkins.
Rights and permissions
About this article
Cite this article
Rodrigues, G.D., Gurgel, J.L., Gonçalves, T.R. et al. Inspiratory muscle training improves physical performance and cardiac autonomic modulation in older women. Eur J Appl Physiol 118, 1143–1152 (2018). https://doi.org/10.1007/s00421-018-3844-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-018-3844-9