Abstract
Purpose
Anti-vascular endothelial growth factor (Anti-VEGF) therapy is currently seen as the standard for treatment of neovascular AMD (nAMD). However, while treatments are highly effective, decisions for initial treatment and retreatment are often challenging for non-retina specialists. The purpose of this study is to develop convolutional neural networks (CNN) that can differentiate treatment indicated presentations of nAMD for referral to treatment centre based solely on SD-OCT. This provides the basis for developing an applicable medical decision support system subsequently.
Methods
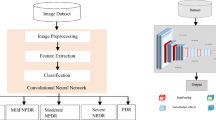
SD-OCT volumes of a consecutive real-life cohort of 1503 nAMD patients were analysed and two experiments were carried out. To differentiate between no treatment class vs. initial treatment nAMD class and stabilised nAMD vs. active nAMD, two novel CNNs, based on SD-OCT volume scans, were developed and tested for robustness and performance. In a step towards explainable artificial intelligence (AI), saliency maps of the SD-OCT volume scans of 24 initial indication decisions with a predicted probability of > 97.5% were analysed (score 0–2 in respect to staining intensity). An AI benchmark against retina specialists was performed.
Results
At the first experiment, the area under curve (AUC) of the receiver-operating characteristic (ROC) for the differentiation of patients for the initial analysis was 0.927 (standard deviation (SD): 0.018), for the second experiment (retreatment analysis) 0.865 (SD: 0.027). The results were robust to downsampling (¼ of the original resolution) and cross-validation (tenfold). In addition, there was a high correlation between the AI analysis and expert opinion in a sample of 102 cases for differentiation of patients needing treatment (κ = 0.824). On saliency maps, the relevant structures for individual initial indication decisions were the retina/vitreous interface, subretinal space, intraretinal cysts, subretinal pigment epithelium space, and the choroid.
Conclusion
The developed AI algorithms can define and differentiate presentations of AMD, which should be referred for treatment or retreatment with anti-VEGF therapy. This may support non-retina specialists to interpret SD-OCT on expert opinion level. The individual decision of the algorithm can be supervised by saliency maps.







Similar content being viewed by others
Abbreviations
- AI:
-
Artificial intelligence
- AMD:
-
Age-related macular degeneration
- AUC:
-
Area under curve
- BCVA:
-
Best corrected visual acuity
- BM:
-
Bruch’s membrane
- CATT trial:
-
Comparison of Age-related Macular Degeneration Treatment Trials: Lucentis-Avastin Trial
- CNN:
-
Convolutional neural network
- CNV:
-
Choroidal neovascularization
- FA:
-
Fluorescein angiography
- ILM:
-
Inner limiting membrane
- IVAN trial:
-
Inhibition of VEGF in Age-related choroidal Neovascularisation trial
- GPU:
-
Graphics processing unit
- LSTM:
-
Long short-term memory
- M:
-
Mean score
- nAMD:
-
Neovascular age-related macular degeneration
- PRN:
-
Pro re nata
- RC:
-
reading centre
- RPE:
-
Retinal pigment epithelium
- ROC:
-
Receiver operating characteristic
- ReLU:
-
Rectified linear unit
- SD:
-
Standard deviation
- SD-OCT:
-
Spectral domain optical coherence tomography
- tanh:
-
Hyperbolic tangent
- TNR:
-
True negative rate
- TPR:
-
True positive rate
- VEGF:
-
Vascular endothelial growth factor
References
Brown DM, Kaiser PK, Michels M et al (2006) Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 355:1432–1444. https://doi.org/10.1056/NEJMoa062655
Stasch-Bouws J, Eller-Woywod SM, Schmickler S et al (2020) IVOM quality assurance in Westfalen-Lippe : Structure of quality assurance and results of the pilot study Q-VERA. Ophthalmologe 117:336–342. https://doi.org/10.1007/s00347-019-01030-3
Brinkmann CK, Chang P, Schick T et al (2019) Baseline diagnostics and initial treatment decision for anti-vascular endothelial growth factor treatment in retinal diseases : Comparison between results by study physician and reading centers (ORCA/OCEAN study). Ophthalmologe 116:753–765. https://doi.org/10.1007/s00347-018-0805-y
Gulshan V, Peng L, Coram M et al (2016) Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. JAMA 316:2402. https://doi.org/10.1001/jama.2016.17216
Lee CS, Tyring AJ, Deruyter NP et al (2017) Deep-learning based, automated segmentation of macular edema in optical coherence tomography. Biomed Opt Express 8:3440–3448. https://doi.org/10.1364/BOE.8.003440
Burlina PM, Joshi N, Pekala M et al (2017) Automated Grading of Age-Related Macular Degeneration From Color Fundus Images Using Deep Convolutional Neural Networks. JAMA Ophthalmol 135:1170–1176. https://doi.org/10.1001/jamaophthalmol.2017.3782
Abràmoff MD, Lavin PT, Birch M et al (2018) Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit Med 1:39. https://doi.org/10.1038/s41746-018-0040-6
De Fauw J, Ledsam JR, Romera-Paredes B et al (2018) Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat Med 24:1342–1350. https://doi.org/10.1038/s41591-018-0107-6
Russakoff DB, Lamin A, Oakley JD et al (2019) Deep Learning for Prediction of AMD Progression: A Pilot Study. Invest Ophthalmol Vis Sci 60:712. https://doi.org/10.1167/iovs.18-25325
Wang Y, Tu D, Du J et al (2019) Classification of Subcortical Vascular Cognitive Impairment Using Single MRI Sequence and Deep Learning Convolutional Neural Networks. Front Neurosci 13:627. https://doi.org/10.3389/fnins.2019.00627
Maetschke S, Antony B, Ishikawa H et al (2019) A feature agnostic approach for glaucoma detection in OCT volumes. PLoS ONE 14:e0219126. https://doi.org/10.1371/journal.pone.0219126
Li Z, Guo C, Nie D et al (2020) Deep learning for detecting retinal detachment and discerning macular status using ultra-widefield fundus images. Commun Biol 3:15. https://doi.org/10.1038/s42003-019-0730-x
Kermany DS, Goldbaum M, Cai W et al (2018) Identifying Medical Diagnoses and Treatable Diseases by Image-Based Deep Learning. Cell 172:1122-1131.e9. https://doi.org/10.1016/j.cell.2018.02.010
Liefers B, Colijn JM, González-Gonzalo C et al (2020) A Deep Learning Model for Segmentation of Geographic Atrophy to Study Its Long-Term Natural History. Ophthalmology 127:1086–1096. https://doi.org/10.1016/j.ophtha.2020.02.009
Schmidt-Erfurth U, Waldstein SM, Klimscha S et al (2018) Prediction of Individual Disease Conversion in Early AMD Using Artificial Intelligence. Invest Ophthalmol Vis Sci 59:3199–3208. https://doi.org/10.1167/iovs.18-24106
Yim J, Chopra R, Spitz T et al (2020) Predicting conversion to wet age-related macular degeneration using deep learning. Nat Med 26:892–899. https://doi.org/10.1038/s41591-020-0867-7
Lee CS, Baughman DM, Lee AY (2016) Deep learning is effective for the classification of OCT images of normal versus Age-related Macular Degeneration. Ophthalmol Retina 1:322–327. https://doi.org/10.1016/j.oret.2016.12.009
Schmidt-Erfurth U, Bogunovic H, Sadeghipour A et al (2018) Machine Learning to Analyze the Prognostic Value of Current Imaging Biomarkers in Neovascular Age-Related Macular Degeneration. Ophthalmol Retina 2:24–30. https://doi.org/10.1016/j.oret.2017.03.015
Rothaus K, Farecki M-L, Mussinghoff P et al (2019) Analysis of the “Portal” Care Model - Examination of the Outcome Quality of IVOM Therapy with Regard to Latency Periods in Exudative AMD. Klin Monbl Augenheilkd 238:293–301. https://doi.org/10.1055/a-0982-5294
IVAN Study Investigators, Chakravarthy U, Harding SP et al (2012) Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 119:1399–1411. https://doi.org/10.1016/j.ophtha.2012.04.015
CATT Research Group, Martin DF, Maguire MG et al (2011) Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 364:1897–1908. https://doi.org/10.1056/NEJMoa1102673
Mazzaferri J, Beaton L, Hounye G et al (2017) Open-source algorithm for automatic choroid segmentation of OCT volume reconstructions. Sci Rep 7:42112. https://doi.org/10.1038/srep42112
Bradski G (2000) The OpenCV Library: Resampling using pixel area relation. https://docs.opencv.org/3.4/da/d54/group__imgproc__transform.html. Accessed 17 Oct 2021
Lim G, Bellemo V, Xie Y et al (2020) Different fundus imaging modalities and technical factors in AI screening for diabetic retinopathy: a review. Eye Vis Lond Engl 7:21. https://doi.org/10.1186/s40662-020-00182-7
Dozat T (2016) Incorporating Nesterov Momentum into Adam. https://openreview.net/forum?id=OM0jvwB8jIp57ZJjtNEZ. Accessed 17 Oct 2021
Chollet F (2015) Keras. https://keras.io. Accessed 17 Oct 2021
Abadi M, Agarwal A, Barham P, Brevdo, E (2015) TensorFlow: Large-scale machine learning on heterogeneous systems. https://www.tensorflow.org. Accessed 17 Oct 2021
Simonyan K, Vedaldi, Andrea, Zisserman, Andrew (2014) Deep Inside Convolutional Networks: Visualising Image Classification Models and Saliency Maps. arXiv:1312.6034. Accessed 17 Oct 2021
Kotikalapudi R (2017) What is Saliency? https://raghakot.github.io/keras-vis/visualizations/saliency/#what-is-saliency. Accessed 17 Oct 2021
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39:561–577
Fleiss JL (1971) Measuring nominal scale agreement among many raters. Psychol Bull 76:378–382. https://doi.org/10.1037/h0031619
Mishra Z, Ganegoda A, Selicha J et al (2020) Automated Retinal Layer Segmentation Using Graph-based Algorithm Incorporating Deep-learning-derived Information. Sci Rep 10:9541. https://doi.org/10.1038/s41598-020-66355-5
Maloca PM, Lee AY, de Carvalho ER et al (2019) Validation of automated artificial intelligence segmentation of optical coherence tomography images. PLoS ONE 14:e0220063. https://doi.org/10.1371/journal.pone.0220063
Kurmann T, Yu S, Márquez-Neila P et al (2019) Expert-level Automated Biomarker Identification in Optical Coherence Tomography Scans. Sci Rep 9:13605. https://doi.org/10.1038/s41598-019-49740-7
Schlegl T, Waldstein SM, Bogunovic H et al (2018) Fully Automated Detection and Quantification of Macular Fluid in OCT Using Deep Learning. Ophthalmology 125:549–558. https://doi.org/10.1016/j.ophtha.2017.10.031
Yan Q, Weeks DE, Xin H et al (2020) Deep-learning-based Prediction of Late Age-Related Macular Degeneration Progression. Nat Mach Intell 2:141–150. https://doi.org/10.1038/s42256-020-0154-9
Acknowledgements
H. Faatz, MD 1,6, as a retina specialist, he was involved in analysing the saliency maps. B. Heimes-Bussmann, MD 1,6, M. Ziegler, MD 1,6, as retina specialists, they were involved in benchmarking the AI analysis of the initial indication and in analysing the saliency maps.
Funding
This study was funded by Novartis Pharma GmbH, Nuernberg, Germany. The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval for the study was obtained from the local ethics committee at the University of Muenster.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. O. Ester, S. Aydin, M. Quassowski and K. Rothaus declare they have no financial interests. M. Gutfleisch received speaker honoraria from Novartis, Bayer and Zeiss outside the submitted work. G. Spital received speaker honoraria from Zeiss, OD-OS and Allergan outside the submitted work. A. Lommatzsch received speaker honoraria from Novartis, Bayer and Zeiss outside the submitted work. A. M. Dubis has a patent OCT analysis technology pending, and a patent prediction method from retinal imaging pending outside the submitted work. D. Pauleikhoff received speaker honoraria from Bayer, Novartis, Zeiss and Allergan outside the submitted work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gutfleisch, M., Ester, O., Aydin, S. et al. Clinically applicable deep learning-based decision aids for treatment of neovascular AMD. Graefes Arch Clin Exp Ophthalmol 260, 2217–2230 (2022). https://doi.org/10.1007/s00417-022-05565-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05565-1