Abstract
Purpose
To investigate the effectiveness and safety of posterior scleral reinforcement (PSR) combined with vitrectomy for myopic foveoschisis (MF) treatment.
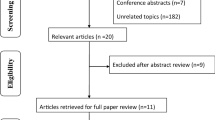
Methods
We conducted a systematic review and meta-analysis. We evaluated the improvement of best-corrected visual acuity (BCVA) in logMAR unit, the percentage of patients with improved or stabled BCVA, benefit on axial length (AL), the retinal reattachment rate, the macular hole (MH) closure rate, as well as the complication rate.
Results
Fourteen studies (311 eyes) were included. Overall, patients’ BCVA improved − 0.46 (95% confidence interval [CI] − 0.52, − 0.40) logMAR unit, with 80% (95%CI 74%, 85%) benefiting from BCVA improvement and 6% (95%CI 3%, 10%) suffering from BCVA loss. Patients’ AL was shortened by − 1.74 (95%CI − 2.92, − 0.57) mm, and for patients whose AL was ≥ 30 mm, the average benefit reached − 3.68 (95%CI − 4.59, − 2.77) mm. Ninety-three percent (95%CI 89%, 96%) of the patients achieved retinal reattachment, and 65% (95%CI 47%, 80%) of the MH was closed. Patients’ central foveal thickness decreased; the MD was − 187.32 (95%CI − 206.25, − 168.40) mm. The pooled complication rate was 9% (95%CI 8%, 19%), with extrusion, choroidal atrophy, and choroidal neovascularization being the most common complications. Subgroup analysis indicated no statistical difference in BCVA improvement, AL change, retinal reattachment rate, and complication rate between patients with or without MH. Subgroup analysis indicated no statistical difference in the above four outcomes between the primary and the recurrent patients either. There was no statistical difference in the above four outcomes no matter ILM peeling was combined or not.
Conclusion
PSR combined with vitrectomy helps improve 80% MF patients’ BCVA; the average benefit on BCVA is − 0.46 logMAR unit. The average change in AL is − 1.74 mm; patients with AL ≥ 30 mm benefit much more than the patients with AL < 30 mm. The retinal reattachment rate is up to 93%; the MH closure rate is 65%. About 9% patients will suffer from extrusion, choroidal atrophy, choroidal neovascularization, and other complications. The outcomes were not influenced by presence of MH, disease recurrence, or ILM peeling.







Similar content being viewed by others
References
Ikuno Y (2017) Overview of the complications of high myopia. Retina 37(12):2347–2351
Chen YP, Chen TL, Yang KR, Lee WH, Kuo YH, Chao AN, Wu WC, Chen KJ, Lai CC (2006) Treatment of retinal detachment resulting from posterior staphyloma-associated macular hole in highly myopic eyes. Retina 26(1):25–31
Chazalon T, Ruellan YM (1986) Treatment of retinal detachment of the posterior pole in severe myopia by vitrectomy and gas tamponade. Bull Soc Ophtalmol Fr 86(8–9):981–982 987-988
Xie A, Lei J (2013) Pars plana vitrectomy and silicone oil tamponade as a primary treatment for retinal detachment caused by macular holes in highly myopic eyes: a risk-factor analysis. Curr Eye Res 38(1):108–113
Kuhn F (2003) Internal limiting membrane removal for macular detachment in highly myopic eyes. Am J Ophthalmol 135(4):547–549
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J (1999) Macular hole surgery with internal-limiting membrane peeling and intravitreous air. OPHTHALMOLOGY 106(7):1392–1397 1397-1398
Baba R, Wakabayashi Y, Umazume K, Ishikawa T, Yagi H, Muramatsu D, Goto H (2017) Efficacy of the inverted internal limiting membrane flap technique with vitrectomy for retinal detachment associated with myopic macular holes. Retina 37(3):466–471
Hong MC, Wu TT, Sheu SJ (2011) Primary gas tamponade in the management of macular hole with retinal detachment in highly myopic eyes. J Chin Med Assoc 74(3):121–124
Ikuno Y, Sayanagi K, Ohji M, Kamei M, Gomi F, Harino S, Fujikado T, Tano Y (2004) Vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol 137(4):719–724
Oshima Y, Ikuno Y, Motokura M, Nakae K, Tano Y (1998) Complete epiretinal membrane separation in highly myopic eyes with retinal detachment resulting from a macular hole. Am J Ophthalmol 126(5):669–676
Ando Y, Hirakata A, Ohara A, Yokota R, Orihara T, Hirota K, Koto T, Inoue M (2017) Vitrectomy and scleral imbrication in patients with myopic traction maculopathy and macular hole retinal detachment. Graefes Arch Clin Exp Ophthalmol 255(4):673–680
Kono T, Takesue Y, Shiga S (2006) Scleral resection technique combined with vitrectomy for a macular hole retinal detachment in highly myopic eyes. OPHTHALMOLOGICA 220(3):159–163
Mateo C, Bures-Jelstrup A, Navarro R, Corcostegui B (2012) Macular buckling for eyes with myopic foveoschisis secondary to posterior staphyloma. Retina 32(6):1121–1128
Ward B (2013) Degenerative myopia: myopic macular schisis and the posterior pole buckle. Retina 33(1):224–231
Alkabes M, Bures-Jelstrup A, Salinas C, Medeiros MD, Rios J, Corcostegui B, Mateo C (2014) Macular buckling for previously untreated and recurrent retinal detachment due to high myopic macular hole: a 12-month comparative study. Graefes Arch Clin Exp Ophthalmol 252(4):571–581
Baba T, Tanaka S, Nizawa T, Oshitari T, Yamamoto S (2016) Scleral imbrication combined with pars plana vitrectomy without internal limiting membrane peeling for myopic schisis. Retina 36(10):1927–1934
Mura M, Iannetta D, Buschini E, de Smet MD (2017) T-shaped macular buckling combined with 25G pars plana vitrectomy for macular hole, macular schisis, and macular detachment in highly myopic eyes. Br J Ophthalmol 101(3):383–388
Ma J, Li H, Ding X, Tanumiharjo S, Lu L (2017) Effectiveness of combined macular buckle under direct vision and vitrectomy with ILM peeling in refractory macular hole retinal detachment with extreme high axial myopia: a 24-month comparative study. Br J Ophthalmol 101(10):1386–1394
Cao K, Friedman DS, Jin S, Yusufu M, Zhang J, Wang J, Hou S, Zhu G, Wang B, Xiong Y, Li J, Li X, He H, Chai L, Wan XH (2019) Multifocal versus monofocal intraocular lenses for age-related cataract patients: a system review and meta-analysis based on randomized controlled trials. Surv Ophthalmol 64(5):647–658
Deeks J, Higgins J, Altman D (2019) https://training.cochrane.org/handbook/current/chapter-10. Accessed 10 October 2019
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. BIOMETRICS 56(2):455–463
Bures-Jelstrup A, Alkabes M, Gomez-Resa M, Rios J, Corcostegui B, Mateo C (2014) Visual and anatomical outcome after macular buckling for macular hole with associated foveoschisis in highly myopic eyes. Br J Ophthalmol 98(1):104–109
Fujikawa M, Kawamura H, Kakinoki M, Sawada O, Sawada T, Saishin Y, Ohji M (2014) Scleral imbrication combined with vitrectomy and gas tamponade for refractory macular hole retinal detachment associated with high myopia. Retina 34(12):2451–2457
Ghoraba HH, Mansour HO, Elgouhary SM (2014) Effect of 360 degrees episcleral band as adjunctive to pars plana vitrectomy and silicone oil tamponade in the management of myopic macular hole retinal detachment. Retina 34(4):670–678
Li XJ, Yang XP, Li QM, Wang YY, Wang J, Lyu XB, Jia H (2016) Posterior scleral reinforcement combined with vitrectomy for myopic foveoschisis. Int J Ophthalmol 9(2):258–261
Lin H (2015) Posterior sclera reinforcement combined with vitrectomy and internal limiting membrane peeling for high myopic foveoschisis. Chinese Journal of Ocular Trauma and Occupational Eye Disease 9(37):650–653
Qi Y, Duan AL, You QS, Jonas JB, Wang N (2015) Posterior scleral reinforcement and vitrectomy for myopic foveoschisis in extreme myopia. Retina 35(2):351–357
Zheng L, Pan A, Zhu S, Wu Y, Dong L, Xue A (2019) Posterior scleral contraction to treat recurrent or persistent macular detachment after previous vitrectomy in highly myopic eyes. Retina 39(1):193–201
Parolini B, Frisina R, Pinackatt S, Gasparotti R, Gatti E, Baldi A, Penzani R, Lucente A, Semeraro F (2015) Indications and results of a new l-shaped macular buckle to support a posterior staphyloma in high myopia. Retina 35(12):2469–2482
Takano M, Kishi S (1999) Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 128(4):472–476
Phillips CI (1958) Retinal detachment at the posterior pole. Br J Ophthalmol 42(12):749–753
Rosengren B (1966) The silver plomb method in macular holes. Trans Ophthalmol Soc U K 86:49–53
Feman SS, Hepler RS, Straatsma BR (1974) Rhegmatogenous retinal detachment due to macular hole. Management with cryotherapy and a Y-shaped sling. Arch Ophthalmol 91(5):371–372
Sayanagi K, Ikuno Y, Tano Y (2006) Tractional internal limiting membrane detachment in highly myopic eyes. Am J Ophthalmol 142(5):850–852
Ikuno Y (2006) Pathogenesis and treatment of myopic foveoschisis. Nippon Ganka Gakkai Zasshi 110(11):855–863
Li X, Wang W, Tang S, Zhao J (2009) Gas injection versus vitrectomy with gas for treating retinal detachment owing to macular hole in high myopes. OPHTHALMOLOGY 116(6):1182–1187
Lam RF, Lai WW, Cheung BT, Yuen CY, Wong TH, Shanmugam MP, Lam DS (2006) Pars plana vitrectomy and perfluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthalmol 142(6):938–944
Matsumura N, Ikuno Y, Tano Y (2004) Posterior vitreous detachment and macular hole formation in myopic foveoschisis. Am J Ophthalmol 138(6):1071–1073
Lansing MB, Glaser BM, Liss H, Hanham A, Thompson JT, Sjaarda RN, Gordon AJ (1993) The effect of pars plana vitrectomy and transforming growth factor-beta 2 without epiretinal membrane peeling on full-thickness macular holes. OPHTHALMOLOGY 100(6):868–871 871-872
Ripandelli G, Coppe AM, Fedeli R, Parisi V, D'Amico DJ, Stirpe M (2001) Evaluation of primary surgical procedures for retinal detachment with macular hole in highly myopic eyes: a comparison [corrected] of vitrectomy versus posterior episcleral buckling surgery. OPHTHALMOLOGY 108(12):2258–2264 2265
Theodossiadis GP, Theodossiadis PG (2005) The macular buckling procedure in the treatment of retinal detachment in highly myopic eyes with macular hole and posterior staphyloma: mean follow-up of 15 years. Retina 25(3):285–289
Tideman JW, Snabel MC, Tedja MS, van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE, Boon CJ, Geerards AJ, Luyten GP, Verhoeven VJ, Klaver CC (2016) Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol 134(12):1355–1363
Sit AJ, Lin SC, Kazemi A, McLaren JW, Pruet CM, Zhang X (2017) In vivo noninvasive measurement of Young’s modulus of elasticity in human eyes: a feasibility study. J Glaucoma 26(11):967–973
Meng B, Zhao L, Yin Y, Li H, Wang X, Yang X, You R, Wang J, Zhang Y, Wang H, Du R, Wang N, Zhan S, Wang Y (2017) Internal limiting membrane peeling and gas tamponade for myopic foveoschisis: a systematic review and meta-analysis. BMC Ophthalmol 17(1):166
Smiddy WE, Feuer W, Cordahi G (2001) Internal limiting membrane peeling in macular hole surgery. Ophthalmology 108(8):1471–1476 1477-1478
Pieczynski J, Kuklo P, Grzybowski A (2018) Pars plana vitrectomy with silicone oil tamponade for primary and secondary macular hole closure: is it still a useful procedure? Eur J Ophthalmol 28(5):503–514
Couvillion SS, Smiddy WE, Flynn HJ, Eifrig CW, Gregori G (2005) Outcomes of surgery for idiopathic macular hole: a case-control study comparing silicone oil with gas tamponade. Ophthalmic Surg Lasers Imaging 36(5):365–371
Chen SN, Yang CM (2016) Inverted internal limiting membrane insertion for macular hole-associated retinal detachment in high myopia. Am J Ophthalmol 162:99–106
El ML, Bouladi M, Chebil A, Kort F, Bouraoui R, Largueche L, Mghaieth F (2012) Choroidal thickness measurement in highly myopic eyes using SD-OCT. Ophthalmic Surg Lasers Imaging 43(6 Suppl):S38–S43
Financial support
This study was funded by the National natural science fund (grant number 30471861).
Author information
Authors and Affiliations
Contributions
Study design and concept (Xiu Hua Wan, Jinda Wang, Jingshang Zhang, Kai Cao); database search (Kai Cao, Shanshan Jin); data extracting (Kai Cao, Shanshan Jin); data analysis (Kai Cao); manuscript writing (Kai Cao, Xiu Hua Wan); manuscript revising (Mayinuer Yusufu, Xiaoxia Li, Guyu Zhu, Hailong He).
Corresponding author
Ethics declarations
Conflict of interest
Author Kai Cao declares that he has no conflict of interest. Author Jinda Wang declares that he has no conflict of interest. Author Jingshang Zhang declares that he has no conflict of interest. Author Mayinuer Yusufu declares that she has no conflict of interest. Author Shanshan Jin declares that she has no conflict of interest. Author Guyu Zhu declares that she has no conflict of interest. Author Hailong He declares that he has no conflict of interest. Author Yue Qi declares that she has no conflict of interest. Author Xiu Hua Wan has received research grants from the National Natural Science Foundation of China.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Appendix 1. Search strategy
((“sclera”[MeSH Terms] OR “sclera”[All Fields] OR “scleral”[All Fields]) OR (“sclera”[MeSH Terms] OR “sclera”[All Fields]) OR (posterior[All Fields] AND (“sclera”[MeSH Terms] OR “sclera”[All Fields] OR “scleral”[All Fields]) AND (“reinforcement (psychology)”[MeSH Terms] OR (“reinforcement”[All Fields] AND “(psychology)”[All Fields]) OR “reinforcement (psychology)”[All Fields] OR “reinforcement”[All Fields])) OR (“Policy Stud Rev”[Journal] OR “Pac Sociol Rev”[Journal] OR “psr”[All Fields]) OR buckle[All Fields] OR buckling[All Fields] OR (gas[All Fields] AND tamponade[All Fields]) OR ((“membranes”[MeSH Terms] OR “membranes”[All Fields] OR “membrane”[All Fields]) AND peeling[All Fields]) OR ERM[All Fields] OR ILM[All Fields]) AND ((“vitrectomy”[MeSH Terms] OR “vitrectomy”[All Fields]) OR (“vitrectomy”[MeSH Terms] OR “vitrectomy”[All Fields] OR “vitrectomies”[All Fields]) OR (pars[All Fields] AND plana[All Fields] AND (“vitrectomy”[MeSH Terms] OR “vitrectomy”[All Fields])) OR ppv[All Fields]) AND ((“retinoschisis”[MeSH Terms] OR “retinoschisis”[All Fields]) OR foveoschisis[All Fields] OR (macular[All Fields] AND cleft[All Fields]) OR (macular[All Fields] AND split[All Fields]) OR ((“retinal perforations”[MeSH Terms] OR (“retinal”[All Fields] AND “perforations”[All Fields]) OR “retinal perforations”[All Fields] OR (“macular”[All Fields] AND “hole”[All Fields]) OR “macular hole”[All Fields]) OR (“retinal detachment”[MeSH Terms] OR (“retinal”[All Fields] AND “detachment”[All Fields]) OR “retinal detachment”[All Fields]))) AND ((pathologic[All Fields] AND (“myopia”[MeSH Terms] OR “myopia”[All Fields])) OR (high[All Fields] AND (“myopia”[MeSH Terms] OR “myopia”[All Fields])) OR (“myopia”[MeSH Terms] OR “myopia”[All Fields] OR “myopic”[All Fields]))
Rights and permissions
About this article
Cite this article
Cao, K., Wang, J., Zhang, J. et al. The effectiveness and safety of posterior scleral reinforcement with vitrectomy for myopic foveoschisis treatment: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 258, 257–271 (2020). https://doi.org/10.1007/s00417-019-04550-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04550-5