Abstract
Background
Motor capacity is crucial in amyotrophic lateral sclerosis (ALS) clinical trial design and patient care. However, few studies have explored the potential of multimodal MRI to predict motor capacity in ALS. This study aims to evaluate the predictive value of cervical spinal cord MRI parameters for motor capacity in ALS compared to clinical prognostic factors.
Methods
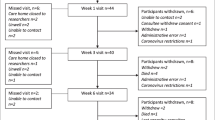
Spinal multimodal MRI was performed shortly after diagnosis in 41 ALS patients and 12 healthy participants as part of a prospective multicenter cohort study, the PULSE study (NCT 2013-A00969-36). Motor capacity was assessed using ALSFRS-R scores. Multiple stepwise linear regression models were constructed to predict motor capacity at 3 and 6 months from diagnosis, based on clinical variables, structural MRI measurements, including spinal cord cross-sectional area (CSA), anterior–posterior, and left-to-right cross-section diameters at vertebral levels from C1 to T4, and diffusion parameters in the lateral corticospinal tracts (LCSTs) and dorsal columns.
Results
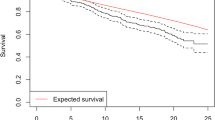
Structural MRI measurements were significantly correlated with the ALSFRS-R score and its sub-scores. And as early as 3 months from diagnosis, structural MRI measurements fit the best multiple linear regression model to predict the total ALSFRS-R (R2 = 0.70, p value = 0.0001) and arm sub-score (R2 = 0.69, p value = 0.0002), and combined with DTI metric in the LCST and clinical factors fit the best multiple linear regression model to predict leg sub-score (R2 = 0.73, p value = 0.0002).
Conclusions
Spinal multimodal MRI could be promising as a tool to enhance prognostic accuracy and serve as a motor function proxy in ALS.



Similar content being viewed by others
Abbreviations
- AAE:
-
Average absolute error
- AD:
-
Axial diffusivity
- ALS:
-
Amyotrophic lateral sclerosis
- ALSFRS-R:
-
ALS functional rating scale-revised
- APD:
-
Anterior–posterior diameter
- RLD:
-
Right-left diameter
- CSA:
-
Cross-sectional area
- DC:
-
Dorsal columns
- DTI:
-
Diffusion tensor imaging
- EPI:
-
Echoplanar imaging
- FA:
-
Fractional anisotropy
- FOV:
-
Field of view
- HC:
-
Healthy control
- LCST:
-
Lateral corticospinal tracts
- LMN:
-
Lower motor neuron
- MD:
-
Mean diffusivity
- MRI:
-
Magnetic resonance imaging
- R 2 :
-
R-Square
- RASE:
-
Relative average squared error
- RD:
-
Radial diffusivity
- SCT:
-
Spinal Cord Toolbox
- SD:
-
Standard deviation
- TSE:
-
Turbo spin-echo
- UMN:
-
Upper motor neuron
References
Robberecht W, Philips T (2013) The changing scene of amyotrophic lateral sclerosis. Nat Rev Neurosci 14:248–264. https://doi.org/10.1038/nrn3430
Rowland LP, Shneider NA (2001) Amyotrophic lateral sclerosis. N Engl J Med 344:1688–1700. https://doi.org/10.1056/nejm200105313442207
Turner MR, Bowser R, Bruijn L, Dupuis L, Ludolph A, McGrath M, Manfredi G, Maragakis N, Miller RG, Pullman SL, Rutkove SB, Shaw PJ, Shefner J, Fischbeck KH (2013) Mechanisms, models and biomarkers in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 14:19–32. https://doi.org/10.3109/21678421.2013.778554
Turner MR, Benatar M (2015) Ensuring continued progress in biomarkers for amyotrophic lateral sclerosis. Muscle Nerve 51:14–18. https://doi.org/10.1002/mus.24470
Ravits J, Paul P, Jorg C (2007) Focality of upper and lower motor neuron degeneration at the clinical onset of ALS. Neurology 68:1571–1575. https://doi.org/10.1212/01.wnl.0000260965.20021.47
Gordon PH, Cheng B, Katz IB, Pinto M, Hays AP, Mitsumoto H, Rowland LP (2006) The natural history of primary lateral sclerosis. Neurology 66:647–653. https://doi.org/10.1212/01.wnl.0000200962.94777.71
Kraemer M, Buerger M, Berlit P (2010) Diagnostic problems and delay of diagnosis in amyotrophic lateral sclerosis. Clin Neurol Neurosurg 112:103–105. https://doi.org/10.1016/j.clineuro.2009.10.014
Witzel S, Frauhammer F, Steinacker P, Devos D, Pradat PF, Meininger V, Halbgebauer S, Oeckl P, Schuster J, Anders S, Dorst J, Otto M, Ludolph AC (2021) Neurofilament light and heterogeneity of disease progression in amyotrophic lateral sclerosis: development and validation of a prediction model to improve interventional trials. Transl Neurodegener 10:31. https://doi.org/10.1186/s40035-021-00257-y
Cai Z, Liu Q, Liu M, Yang X, Shen D, Sun X, He D, Zhang K, Shang L, Zhang X, Cui L (2022) Survival analysis of clinical and genetic factors in an amyotrophic lateral sclerosis cohort from China. Neurol Res 44:651–658. https://doi.org/10.1080/01616412.2022.2029292
Westeneng HJ, Debray TPA, Visser AE, van Eijk RPA, Rooney JPK, Calvo A, Martin S, McDermott CJ, Thompson AG, Pinto S, Kobeleva X, Rosenbohm A, Stubendorff B, Sommer H, Middelkoop BM, Dekker AM, van Vugt J, van Rheenen W, Vajda A, Heverin M, Kazoka M, Hollinger H, Gromicho M, Körner S, Ringer TM, Rödiger A, Gunkel A, Shaw CE, Bredenoord AL, van Es MA, Corcia P, Couratier P, Weber M, Grosskreutz J, Ludolph AC, Petri S, de Carvalho M, Van Damme P, Talbot K, Turner MR, Shaw PJ, Al-Chalabi A, Chiò A, Hardiman O, Moons KGM, Veldink JH, van den Berg LH (2018) Prognosis for patients with amyotrophic lateral sclerosis: development and validation of a personalised prediction model. Lancet Neurol 17:423–433. https://doi.org/10.1016/s1474-4422(18)30089-9
Trojsi F, Siciliano M, Femiano C, Santangelo G, Lunetta C, Calvo A, Moglia C, Marinou K, Ticozzi N, Ferro C, Scialò C, Sorarù G, Conte A, Falzone YM, Tortelli R, Russo M, Sansone VA, Chiò A, Mora G, Silani V, Volanti P, Caponnetto C, Querin G, Sabatelli M, Riva N, Logroscino G, Messina S, Fasano A, Monsurrò MR, Tedeschi G, Mandrioli J (2019) Comparative analysis of C9orf72 and sporadic disease in a large multicenter ALS population: the effect of male sex on survival of C9orf72 positive patients. Front Neurosci. https://doi.org/10.3389/fnins.2019.00485
Ahmed RM, Devenney EM, Strikwerda-Brown C, Hodges JR, Piguet O, Kiernan MC (2020) Phenotypic variability in ALS-FTD and effect on survival. Neurology 94:e2005–e2013. https://doi.org/10.1212/wnl.0000000000009398
Zhou YN, Chen YH, Dong SQ, Yang WB, Qian T, Liu XN, Cheng Q, Wang JC, Chen XJ (2021) Role of blood neurofilaments in the prognosis of amyotrophic lateral sclerosis: a meta-analysis. Front Neurol. https://doi.org/10.3389/fneur.2021.712245
El Mendili MM, Cohen-Adad J, Pelegrini-Issac M, Rossignol S, Morizot-Koutlidis R, Marchand-Pauvert V, Iglesias C, Sangari S, Katz R, Lehericy S, Benali H, Pradat PF (2014) Multi-parametric spinal cord MRI as potential progression marker in amyotrophic lateral sclerosis. PLoS ONE 9:e95516. https://doi.org/10.1371/journal.pone.0095516
European Medicines Agency. Guideline on clinical investigation of medicinal products for the treatment of amyotrophic lateral sclerosis 2016 [Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-treatment-amyotrophic-lateral-sclerosis_en.pdf. Accessed 06 Oct 2022.
U.S. Food and Drug Administration. Guidance for industry: amyotrophic lateral sclerosis: developing drugs for treatment 2019 [Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/amyotrophic-lateral-sclerosis-developing-drugs-treatment-guidance-industry.
Steering committee members of The ALS CNTF Treatment Study Phase I-II Study Group (1996) The Amyotrophic Lateral Sclerosis Functional Rating Scale. Assessment of activities of daily living in patients with amyotrophic lateral sclerosis. The ALS CNTF treatment study (ACTS) phase I-II Study Group. Arch Neurol 53:141–147. https://doi.org/10.1001/archneur.1996.00550020045014
van Eijk R, Kliest T, van den Berg L (2020) Current trends in the clinical trial landscape for amyotrophic lateral sclerosis. Curr Opin Neurol 33:655–661. https://doi.org/10.1097/WCO.0000000000000861
Kiernan MC, Vucic S, Cheah BC, Turner MR, Eisen A, Hardiman O, Burrell JR, Zoing MC (2011) Amyotrophic lateral sclerosis. Lancet 377:942–955. https://doi.org/10.1016/s0140-6736(10)61156-7
El Mendili MM, Querin G, Bede P, Pradat P-F (2019) Spinal cord imaging in amyotrophic lateral sclerosis: historical concepts—novel techniques. Front Neurol 10:350. https://doi.org/10.3389/fneur.2019.00350
Cohen-Adad J, El Mendili MM, Morizot-Koutlidis R, Lehéricy S, Meininger V, Blancho S, Rossignol S, Benali H, Pradat PF (2013) Involvement of spinal sensory pathway in ALS and specificity of cord atrophy to lower motor neuron degeneration. Amyotroph Lateral Scler Frontotemporal Degener 14:30–38. https://doi.org/10.3109/17482968.2012.701308
Branco LM, De Albuquerque M, De Andrade HM, Bergo FP, Nucci A, França MC Jr (2014) Spinal cord atrophy correlates with disease duration and severity in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 15:93–97. https://doi.org/10.3109/21678421.2013.852589
Nair G, Carew JD, Usher S, Lu D, Hu XP, Benatar M (2010) Diffusion tensor imaging reveals regional differences in the cervical spinal cord in amyotrophic lateral sclerosis. Neuroimage 53:576–583. https://doi.org/10.1016/j.neuroimage.2010.06.060
Querin G, El Mendili MM, Lenglet T, Delphine S, Marchand-Pauvert V, Benali H, Pradat PF (2017) Spinal cord multi-parametric magnetic resonance imaging for survival prediction in amyotrophic lateral sclerosis. Eur J Neurol 24:1040–1046. https://doi.org/10.1111/ene.13329
Grolez G, Kyheng M, Lopes R, Moreau C, Timmerman K, Auger F, Kuchcinski G, Duhamel A, Jissendi-Tchofo P, Besson P, Laloux C, Petrault M, Devedjian JC, Pérez T, Pradat PF, Defebvre L, Bordet R, Danel-Brunaud V, Devos D (2018) MRI of the cervical spinal cord predicts respiratory dysfunction in ALS. Sci Rep 8:1828. https://doi.org/10.1038/s41598-018-19938-2
Querin G, El Mendili MM, Bede P, Delphine S, Lenglet T, Marchand-Pauvert V, Pradat PF (2018) Multimodal spinal cord MRI offers accurate diagnostic classification in ALS. J Neurol Neurosurg Psychiatry 89:1220–1221. https://doi.org/10.1136/jnnp-2017-317214
Brooks BR, Miller RG, Swash M, Munsat TL (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1:293–299. https://doi.org/10.1080/146608200300079536
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169:13–21. https://doi.org/10.1016/s0022-510x(99)00210-5
Gros C, De Leener B, Dupont SM, Martin AR, Fehlings MG, Bakshi R, Tummala S, Auclair V, McLaren DG, Callot V, Cohen-Adad J, Sdika M (2018) Automatic spinal cord localization, robust to MRI contrasts using global curve optimization. Med Image Anal 44:215–227. https://doi.org/10.1016/j.media.2017.12.001
Fonov VS, Le Troter A, Taso M, De Leener B, Lévêque G, Benhamou M, Sdika M, Benali H, Pradat PF, Collins DL, Callot V, Cohen-Adad J (2014) Framework for integrated MRI average of the spinal cord white and gray matter: the MNI-Poly-AMU template. Neuroimage 102:2817–2827. https://doi.org/10.1016/j.neuroimage.2014.08.057
Lévy S, Benhamou M, Naaman C, Rainville P, Callot V, Cohen-Adad J (2015) White matter atlas of the human spinal cord with estimation of partial volume effect. Neuroimage 119:262–271. https://doi.org/10.1016/j.neuroimage.2015.06.040
Jiao Y, Lin F, Wu J, Li H, Wang L, Jin Z, Wang S, Cao Y (2018) A supplementary grading scale combining lesion-to-eloquence distance for predicting surgical outcomes of patients with brain arteriovenous malformations. J Neurosurg 128:530–540. https://doi.org/10.3171/2016.10.Jns161415
Sabatelli M, Madia F, Conte A, Luigetti M, Zollino M, Mancuso I, Lo Monaco M, Lippi G, Tonali P (2008) Natural history of young-adult amyotrophic lateral sclerosis. Neurology 71:876–881. https://doi.org/10.1212/01.wnl.0000312378.94737.45
Chen L, Zhang B, Chen R, Tang L, Liu R, Yang Y, Yang Y, Liu X, Ye S, Zhan S, Fan D (2015) Natural history and clinical features of sporadic amyotrophic lateral sclerosis in China. J Neurol Neurosurg Psychiatry 86:1075–1081. https://doi.org/10.1136/jnnp-2015-310471
Paquin M, El Mendili MM, Gros C, Dupont SM, Cohen-Adad J, Pradat PF (2018) Spinal cord gray matter atrophy in amyotrophic lateral sclerosis. AJNR Am J Neuroradiol 39:184–192. https://doi.org/10.3174/ajnr.A5427
Barry RL, Torrado-Carvajal A, Kirsch JE, Arabasz GE, Albrecht DS, Alshelh Z, Pijanowski O, Lewis AJ, Keegan M, Reynolds B, Knight PC, Morrissey EJ, Loggia ML, Atassi N, Hooker JM, Babu S (2022) Selective atrophy of the cervical enlargement in whole spinal cord MRI of amyotrophic lateral sclerosis. NeuroImage Clin 36:103199. https://doi.org/10.1016/j.nicl.2022.103199
Bede P, Hardiman O (2014) Lessons of ALS imaging: Pitfalls and future directions—a critical review. NeuroImage Clin 4:436–443. https://doi.org/10.1016/j.nicl.2014.02.011
Cao B, Wei Q, Ou R, Zhang L, Hou Y, Chen Y, Shang H (2019) Neurophysiological index is associated with the survival of patients with amyotrophic lateral sclerosis. Clin Neurophysiol 130:1730–1733. https://doi.org/10.1016/j.clinph.2019.05.012
Acknowledgements
The authors would like to express their gratitude to all the participants and their families for their cooperation. The research was generously supported by the French ARSLA charity (Christine Tabuenca, Marie FranceCazalère, Sabine Turgeman, and Valérie Goutines), as well as the French clinical research networks FILSLAN and ACT4ALS-MND. The authors are also grateful to the Fédération de la Recherche Clinique du CHU de Lille for their invaluable support (Anne-Sophie Rolland, Alain Duhamel, Maeva Kheng, Julien Labreuch, Dominique Deplanque, Edouard Millois, Victor Laugeais, Maxime Caillier, Aymen Aouni, Pauline Guyon, Francine Niset, Valérie Santraine, Marie Pleuvret, Mathilde Bon and Laetitia Thibault). We also thank the neurologists who participated in the recruitment of the patients. We thank the Center for NeuroImaging Research (CENIR), the CATI platform especially Marie Chupin and Fouzia El-Mountassir, and the Center for Clinical Investigation, especially Nadia Osman and Vanessa Brochard, in the Brain Institute (Pitié-Salpêtrière Hospital, Paris, France).
Lille Neurologists: Dr Veronique Danel-Brunaud, Pr Caroline Moreau. Pneumologists: Dr Thierry Perez. Neuroradiologists: Dumont. Neuropsychologists: Pr K Dujardin. Neurophysiologists: Dr Arnaud Delval; Biologists: Patrick Gelé. Clinical Assistant: Marie Pleuvret, Valerie Santraine, Francine Niset, Julien Dumont, Victor Laugeais, Mathilde Bon. Clinical trials vigilance unit: Thavarak Ouk, Camille Potey, Celine Leclercq, Elise Gers. Paris Neurologists: Dr Francois Salachas, Dr Pierre-François Pradat, Dr Gaelle Bruneteau. Neuropsychologists: Dr Lucette Lacomblez, Julie Socha, Fanny Pineau. Neurophysiologists: Dr Timothee Lenglet. Biologists: Patricia Doucelance Stéphanie Folhinha. Clinical Assistant: Amandine Bordet, Hugo Royer, Nadia Osman, Sabah Ait Khelifa. Tours Neurologists: Dr Philippe Corcia, Dr Stephane Beltran; Pneumologists: Dr Delphine Carmier. Neuroradiologists: Dr Laurent Barantin. Biologists: Hélène Blasco. Clinical Assistant: Salah Eddine Bakkouche, Mohad Mouzouri. Saint-Etienne Neurologists: Pr Jean-Christophe Antoine, Pr Jean-Philippe Camdessanché, Dr Nathalie Dimier, Dr Anne-Laure Kaminsky. Pneumologists: Dr Isabelle Court-Fortune. Neuroradiologists: Dr Claire Boutet. Biologists: Philippe Gonzalo. Clinical Assistant: Vincent Visneux, Karine Ferraud, Georgette Berlier. Brest Neurologists: Dr Steeve Genestet. Pneumologists: Dr Christophe Gut-Gobert. Neuroradiologists: Pr Douraied Ben Salem. Neuropsychologists: Pauline Nicolas, Sabine Larvor; . Biologists: Kevin Mouly, Liana Le Roux, Kevin Postec, Camille Bezeazux, Sylvain Rosec. Clinical Assistant: Hélène Fortin-Prunier, Gaelle Novert, Elsa Menanteau, Kevin Postec, Magali Denizot. Lyon Neurologists: Dr Emilien Bernard, Dr Christophe Vial, Pr Emmanuel Broussole, Dr Juliette Svahn. Pneumologists: Dr Pierre Le Cam; Neuroradiologists: Pr Yves Berthezene, Philippe Combet. Neuropsychologists: Sophie Jacqueline. Clinical Assistant: Camille Neuillet, Adeline Mansuy. Montpellier Neurologists: Pr William Camu, Dr Juntas-Morates, Dr Pageot, Dr Esselin. Neuroradiologists: Dr Champfleur. Neuropsychologists: Roy-Bellina. Biologists: Pr Sylvain Lehmann. Clinical Assistant: Sebastien Alphandry, Laura Labar, Leandra Baudesson. Marseille Neurologists: Pr Sharam Attarian, Dr Aude-Marie Grapperon, Pr Jean Pouget, Dr Annie Verschueren, Dr Jaochim Bas. Pneumologists: Dr Armelle Finet-Monnier. Neuropsychologists: Carole Belingher. Clinical Assistant: Saran Diallo, Nacime Heddadji, Sebastien Alphandery, Leandra Baudesson; Nurse: Pascale Reginensi. Nice Neurologists: Dr Claude Desnuelle, Dr Marie-Hélene Soriani. Neuroradiologists: Dr S Chanalet, Dr Lydiane Mondot. Neurophysiologists: Dr Puma; Biologists: Pr Isabelle Pruvost. Clinical Assistant: Carole Barré. Toulouse Neurologists: Dr Pascal Cintas, Dr Marie-Christine Arne Bes, Dr Blandine Acket, Dr Jérémie Pariente, Dr Isabelle Guilbaud. Neuroradiologists: Pr Fabrice Bonneville. Biologists: Dr E Causse. Physical therapists: Thierry Lagarde. Nutritionists: Jeremy Geffroy. Clinical Assistant: Magali Centelles, Véronique Hermet-Douard. Nancy Neurologists: Dr Sophie Pittion-Vouyovitch, Dr Maud Michon. Neuropsychologists: Mylène Meyer; Biologists: Sandra Lomazzi. Clinical Assistant: Gabriella Hossu, Anne Chatelain. Limoges Neurologists: Pr Philippe Couratier, Dr Geraldine Lautrette. Pneumologists: Dr Francois Vincent, Dr Larie-Therese Antonini, Dr Florent Favard. Neuroradiologists: Dr MLArie-Paule Boncoeur-Martel. Neuropsychologists: Marianne Chouly. Nutritionists: Pr Jean-Claude Desport, Dr Pierre Jesus, Dr Phillipe Fayemendy. Clinical Assistant: Clémence Labetoulle, Julie Catteau, Olivier Villeneuve. Nurse: Selam Machat. Clermont-Ferrand Neurologists: Dr Nathalie Guy, Pr Pierre Clavelou. Pneumologists: Dr Anick Greil, Pr M Duclos. Neuroradiologists: Dr Betty Jean, Dr Carine Chassain, Camille Tsoutsos, Claudine Speziale, Aurélie Cladiere. Nutritionists: Dr C Bouteloup, Dr N Farigon. Clinical Assistant: Sophia Sickout Argondo, Emilie Dumont. Nurse: Sandrine Rouvet. Caen Neurologists: Pr Fausto Viader, Dr Mathilde Lefilliatre, Dr Philippe Mouton, Dr A Mondou. Biologists: Pr Stephane Allouche. Clinical Assistant: Rachida Bari-Makouri. Saint-Brieuc Neurologists: Dr Ivan Kolev, Dr Morgane Pihan. Pneumologists: Dr Helene Le Ho. Neuroradiologists: Bertrand Catroux. Neuropsychologists: Maela Castel, Marine Rigal. Clinical Assistant: Catherine Bellot, Maelle Vomscheid, Marie-Cécile Hervé, Marie-Pierre Duban. Angers Neurologists: Dr Anne Vieillart, Dr Julien Cassereau, Dr Philippe Codron, Dr Vivien Pautot. Pneumologists: Dr Nicole Meslier, Dr Wojciech Trzepizur. Neuroradiologists: JY Tanguy. Neuropsychologists: Pr Philippe Allain, Cecile Thiery. Biologists: Pascal. Reynier. Physical therapists: Tiphaine Barbe, Vialle-Soubranne. Nutritionists: Nathalie Vienne. Clinical Assistant: Audrey Olivier, Jeanne Miller, Marie Bost. Nusre: Fournier. CATI (MRI acquisition management, preprocessing and data management): . David Gay, Robin Bonicel, Fouzia El Mountassir, Clara Fischer, Jean-François Mangin, Marie Chupin, Yann Cointepas. CRB of Lille (Center of Biological Resources): Bertrand Accart, Patrick Gelé, Florine Fievet, Matthieu Chabel, Virginie Derenaucourt, Loïc Facon, Yanick Tchantchou Njosse, Michael Hisbergues, Deplanque. Data management of Lille: Alain Duhamel, Lynda Djemmane, Florence Duflot, Hajar Chouiki. ARSLA CSV (Comité Scientifique et de Valorisation) and CSP (Comité de Suivi et de Pilotage): Christine Tabuenca, Marie-France Cazalère, Philippe Couratier, William Camu, Philippe Corcia, Claude Desnuelle, Maxime Caillier, Véronique Danel, Caroline Morerau, Victor Laugeais, Amelie Lecocq, Nathalie Potin, Marie Frisch, Marie Léon, David Devos, François Salachas, Pierre-Francois Pradat, Lucette Lacomblez, Jean-Philippe Camdessanché, Sharam Attarian, Timothée Langlet, Hélène Blasco, Luc Dupuis, Mathilde Bon, Emilien Bernard, Julien Cassereau, Marie-Hélène Soriani, Cedric Raoul, Sylvain Lehman, Sabine Turgeman, Valérie Goutines.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in accordance with good clinical practise guidelines and local regulations. All participants gave written informed consent prior to participation in the study. The study was approved by the CPP Nord Ouest-IV Ethical Committee (ID-RCB 2013-A00969-36).
Additional information
The members of Pulse study group are listed in acknowledgements section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khamaysa, M., Lefort, M., Pélégrini-Issac, M. et al. Comparison of spinal magnetic resonance imaging and classical clinical factors in predicting motor capacity in amyotrophic lateral sclerosis. J Neurol 270, 3885–3895 (2023). https://doi.org/10.1007/s00415-023-11727-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11727-w