Abstract
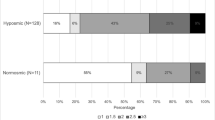
The role of specific sex-related patterns in olfactory dysfunctions of Parkinson’s disease (PD) patients is unclear. The aim of this study was to assess the presence of specific sex-related patterns in olfactory dysfunctions excluding the possibility of confounding effects in patients with Parkinson’s disease. One hundred and sixty-eight participants (99 PD patients and 69 controls) were enrolled and evaluated using Sniffin’ Sticks Extended test (SSET). There was no significant sex difference in the control group for the SSET parameters. By contrast, in the PD group male patients scored significantly lower on odor discrimination (OD), identification (OI), and Threshold-Discrimination-Identification (TDI) score than females. On multivariable linear regression analysis, the only significant predictors of TDI score were sex and apathy. Among PD patients, men showed a significantly greater impairment compared to women in OI, OD and TDI score, but not in odor threshold (OT). These findings highlighted the possible role of sex differences in the development of associated PD non-motor symptoms.
Similar content being viewed by others
References
Schrag A, Ben-Shlomo Y, Quinn NP (2000) Cross sectional prevalence survey of idiopathic Parkinson’s disease and parkinsonism in London. BMJ 321:21–22
Doty RL (2007) Olfaction in PD. Parkinsonism Relat Disord 13:S225–S228
Fullard ME, Morley JF, Duda JE (2017) Olfactory dysfunction as an early biomarker in Parkinson’s disease. Neurosci Bull 33(5):515–525
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18(7):435–450. https://doi.org/10.1038/nrn.2017.62
Haehner A, Boesveldt S, Berendse HW, Mackay-Sim A, Fleischmann J, Silburn PA, Johnston AN, Mellick GD, Herting B, Reichmann H, Hummel T (2009) Prevalence of smell loss in Parkinson’s disease—a multicenter study. Parkinsonism Relat Disord 15(7):490–494
Haehner A, Masala C, Walter S, Reichmann H, Hummel T (2019) Incidence of Parkinson’s disease in a large patient cohort with idiopathic smell and taste loss. J Neurol 266:339–345. https://doi.org/10.1007/s00415-018-9135-x
Huisman E, Uylings HB, Hoogland PV (2008) Gender-related changes in increase of dopaminergic neurons in the olfactory bulb of Parkinson’s disease patients. Mov Disord 23(10):1407–1413
Masala C, Solla P, Liscia A, Defazio G, Saba L, Cannas A, Cavazzana A, Hummel T, Haehner A (2018) Correlation among olfactory function, motors’ symptoms, cognitive impairment, apathy, and fatigue in patients with Parkinson’s disease. J Neurol 265:1764–1771
Poewe W (2008) Non-motor symptoms in Parkinson’s disease. Eur J Neurol 15(1):14–20. https://doi.org/10.1111/j.1468-1331.2008.02056.x
Baba Y, Putzke JD, Whaley NR, Wszolek ZK, Uitti RJ (2005) Gender and the Parkinson’s disease phenotype. J Neurol 252:1201–1205
Guo X, Song W, Chen K, Chen X, Zheng Z, Cao B, Huang R, Zhao B, Wu Y, Shang HF (2013) Gender and onset age related features of non-motor symptoms of patients with Parkinson’s disease—a study from southwest China. Parkinsonism Relat Disord 19:961–965
Haaxma CA, Bloem BR, Borm GF, Oyen WJ, Leenders KL, Eshuis S, Booij J, Dluzen DE, Horstink MW (2007) Gender differences in Parkinson’s disease. J Neurol Neurosurg Psychiatry 78(8):819–824
Baldereschi M, Di Carlo A, Rocca WA, Vanni P, Maggi S, Perissinotto E, Grigoletto F, Amaducci L, Inzitari D, ILSA Working Group (2000) Parkinson’s disease and parkinsonism in a longitudinal study: twofold higher incidence in men. Italian Longitudinal Study on Aging. Neurology 55:1358–1363
Melis M, Sollai G, Masala C, Pisanu C, Cossu G, Melis M, Sarchiotto M, Oppo V, Morelli M, Crnjar R, Hummel T, Tomassini Barbarossa I (2019) Odor identification performance in idiopathic Parkinson’s disease is associated with gender and the genetic variability of the olfactory binding protein. Chem Senses 44:311–318
Martinez-Martin P, Falup Pecurariu C, Odin P, van Hilten JJ, Antonini A, Rojo-Abuin JM, Borges V, Trenkwalder C, Aarsland D, Brooks DJ, Ray Chaudhuri K (2012) Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J Neurol 259(8):1639–1647
Picillo M, Amboni M, Erro R, Longo K, Vitale C, Moccia M, Pierro A, Santangelo G, De Rosa A, De Michele G, Santoro L, Orefice G, Barone P, Pellecchia MT (2013) Gender differences in non-motor symptoms in early, drug naïve Parkinson’s disease. J Neurol 260(11):2849–2855
Picillo M, Pellecchia MT, Erro R, Amboni M, Vitale C, Iavarone A, Moccia M, Allocca R, Orefice G, Barone P (2014) The use of University of Pennsylvania smell identification test in the diagnosis of Parkinson’s disease in Italy. Neurol Sci 35(3):379–383
Picillo M, Nicoletti A, Fetoni V, Garavaglia B, Barone P, Pellecchia MT (2017) The relevance of gender in Parkinson’s disease: a review. J Neurol 264:1583–1607
Liu R, Umbach DM, Peddada SD, Xu Z, Tröster AI, Huang X, Chen H (2015) Potential sex differences in nonmotor symptoms in early drug-naive Parkinson disease. Neurology 84(21):2107–2115
Solla P, Cannas A, Ibba FC, Loi F, Corona M, Orofino G, Marrosu MG, Marrosu F (2012) Gender differences in motor and non-motor symptoms among Sardinian patients with Parkinson’s disease. J Neurological Sci 323:33–39. https://doi.org/10.1016/j.jns.2012.07.026
San Luciano M, Wang C, Ortega RA, Giladi N, Marder K, Bressman S, Saunders-Pullman R, The Michael J Fox Foundation LRRK2 Consortium (2017) Sex differences in LRRK2 G2019S and idiopathic Parkinson’s disease. Ann Clin Transl Neurol 4(11):801–810. https://doi.org/10.1002/acn3.489
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56(1):33–39
Litvan I, Bhatia KP, Burn DJ, Goetz CG, Lang AE, McKeith I, Quinn N, Sethi KD, Shults C, Wenning GK (2003) Movement disorders society scientific issues committee report: SIC task force appraisal of clinical diagnostic criteria for parkinsonian disorders. Mov Disord 18(5):467–486. https://doi.org/10.1002/mds.10459
Conti S, Bonazzi S, Laiacona M, Masina M, Coralli MV (2015) Montreal cognitive assessment (MoCA)-Italian version: regression based norms and equivalent scores. Neurol Sci 36(2):209–214
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Cecchini MP, Federico A, Zanini A, Mantovani E, Masala C, Tinazzi M, Tamburin S (2019) Olfaction and taste in Parkinson’s disease: the association with mild cognitive impairment and the single cognitive domain dysfunction. J Neural Transm 126(5):585–595
Brown RG, Dittner A, Findley L, Wessely SC (2005) The Parkinson fatigue scale. Parkinsonism Relat Disord 11(1):49–55
Pedersen KF, Alves G, Larsen JP, Tysnes OB, Møller SG, Brønnick K (2012) Psychometric properties of the Starkstein apathy scale in patients with early untreated Parkinson disease. Am J Geriatr Psychiatry 20(2):142–148
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Fahn S, Elton R, Members of the UPDRS Development Committee (1987) The unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M (eds) Recent developments in Parkinson’s disease, vol 2. Macmillan Health Care Information, Florham Park, pp 153–163 (293–304)
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G (1997) “Sniffin” sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22(1):39–52. https://doi.org/10.1093/chemse/22.1.39
Hummel T, Kobal G, Gudziol H, Mackay-Sim A (2007) Normative data for the “Sniffin’ sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3000 subjects. Eur Arch Otorhinolaryngol Suppl 264(3):237–243. https://doi.org/10.1007/s00405-006-0173-0
Masala C, Saba L, Cecchini MP, Solla P, Loy F (2018) Olfactory function and age: a Sniffin’ sticks extended test study performed in Sardinia. Chem Percept 11:19–26. https://doi.org/10.1007/s12078-017-9233-7
Doty RL, Deems DA, Stellar S (1988) Olfactory dysfunction in parkinsonism: a general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology 38(8):1237–1244
Masala C, Käehling C, Fall F, Hummel T (2019) Correlation between olfactory function, trigeminal sensitivity, and nasal anatomy in healthy subjects. Eur Arch Oto-Rhino-L 276:1649–1654. https://doi.org/10.1007/s00405-019-05367-y
Fagundo AB, Jiménez-Murcia S, Giner-Bartolomé C, Islam MA, de la Torre R, Pastor A et al (2015) Modulation of higher-order olfaction components on executive functions in humans. PLoS ONE 10(6):e0130319. https://doi.org/10.1371/journal.pone.0130319
Quinn NP, Rossor MN, Marsden CD (1987) Olfactory threshold in Parkinson’s disease. J Neurol Neurosurg Psychiatry 50(1):88–89
Doty RL, Cameron EL (2009) Sex differences and reproductive hormone influences on human odor perception. Physiol Behav 97(2):213–228
Boesveldt S, Yee JR, McClintock MK, Lundström J (2017) Olfactory function and the social lives of older adults: a matter of sex. Sci Rep 7:45118. https://doi.org/10.1038/srep45118
Mayeux R, Marder K, Cote LJ, Denaro J, Hemenegildo N, Mejia H, Tang MX, Lantigua R, Wilder D, Gurland B et al (1995) The frequency of idiopathic Parkinson’s disease by age, ethnic group, and sex in northern Manhattan, 1988–1993. Am J Epidemiol 142:820–827
Beyer C, Pilgrim C, Reisert I (1991) Dopamine content and metabolism in mesencephalic and diencephalic cell cultures: sex differences and effects of sex steroids. J Neurosci 11(5):1325–1333
Acknowledgements
The authors thank all the participants for their availability and Dr. Alan Moat for improving the English text. This work was supported by a grant from the University of Cagliari (Progetti di Ricerca di Interesse Dipartimentale, PRID 2017).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the local Ethics Committee (Prot. PG/2018/10157) and was performed according to the Declaration of Helsinki.
Informed consent
Participants received an explanatory statement and gave their written informed consent to participate in the study.
Rights and permissions
About this article
Cite this article
Solla, P., Masala, C., Liscia, A. et al. Sex-related differences in olfactory function and evaluation of possible confounding factors among patients with Parkinson’s disease. J Neurol 267, 57–63 (2020). https://doi.org/10.1007/s00415-019-09551-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09551-2