Abstract
Although Parkinson’s disease (PD) is usually considered as a movement disorder, it is strongly associated with non-motor symptoms (NMS), including smell and taste dysfunctions, cognitive impairment, apathy, fatigue, and autonomic dysregulation. Olfactory deficit is considered the most common NMS in PD preceding the motor symptoms for years. The aim of this study was to investigate olfactory function, cognitive impairment, apathy, and fatigue in patients with PD in comparison with healthy controls, and subsequently to analyse the correlations between these NMS and motor symptoms severity in subjects with PD. One hundred and forty-seven participants were enrolled (96 PD patients, mean age in years 67.5, SD 7.2; 51 healthy controls; mean age 65.1, SD 11.8). Olfactory function was evaluated using the Sniffin’ Sticks test (odor detection threshold, discrimination and identification). The Montreal Cognitive Assessment (MoCA) was used to assess cognitive impairment. Apathy was examined by the self-report version of Starkstein Apathy Scale and fatigue was evaluated with the Parkinson’s Disease Fatigue Scale. PD patients showed severe impairment in odor detection threshold, discrimination, and identification compared to healthy controls. Moreover, in PD patients, apathy and fatigue scores were significantly increased, while MoCA scores were decreased in comparison with controls. Multivariate linear regression analyses showed that both apathy and Unified PD Rating Scale (UPDRS) were associated with odor identification, discrimination and Threshold–Discrimination–Identification (TDI) score. In conclusion, our results reported changes in apathy and motor disability as significant predictors in alterations of odor identification, discrimination and TDI score. Furthermore, these data suggest that olfactory dysfunction might progress in tight relation with motor impairment UPDRS but also with non-motor symptoms such as apathy.





Similar content being viewed by others
References
Halliday GM, Stevens CH, Hons B (2011) Glia: initiators and progressors of pathology in Parkinson’ s disease. Mov Disord 26(1):6–17. https://doi.org/10.1002/23455
Poewe W (2008) Non-motor symptoms in Parkinson’s disease. Eur J Neurol 15(1):14–20. https://doi.org/10.1111/j.1468-1331.2008.02056.x
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18(7):435–450. https://doi.org/10.1038/nrn.2017.62
Ansari KA, Johnson A (1975) Olfactory function in patients with Parkinson’s disease. J Chronic Dis 28(9):493–497. https://doi.org/10.1016/0021-9681(75)90058-2
Berendse HW, Roos DS, Raijmakers P, Doty RL (2011) Motor and non-motor correlates of olfactory dysfunction in Parkinson’s disease. J Neurol Sci 310(1–2):21–24. https://doi.org/10.1016/j.jns.2011.06.020
Haehner A, Boesveldt S, Berendse HW, Mackay-Sim A, Fleischmann J, Silburn PA, Johnston AN, Mellick GD, Herting B, Reichmann H, Hummel T (2009) Prevalence of smell loss in Parkinson’s disease—a multicenter study. Parkinsonism Relat Disord 15(7):490–494. https://doi.org/10.1016/j.parkreldis.2008.12.005
Boesveldt S, Verbaan D, Knol DL, Visser M, van Rooden SM, van Hilten JJ, Berendse HW (2008) A comparative study of odor identification and odor discrimination deficits in Parkinson’s disease. Mov Disord 23(14):1984–1990. https://doi.org/10.1002/mds.22155
Duda JE (2010) Olfactory system pathology as a model of Lewy neurodegenerative disease. J Neurol Sci 289(1–2):49–54. https://doi.org/10.1016/j.jns.2009.08.042
Verbaan D, Boesveldt S, Van Rooden SM, Visser M, Marinus J, Macedo MG, Fang Y, Heutink P, Berendse HW, Van Hilten JJ (2008) Is olfactory impairment in Parkinson disease related to phenotypic or genotypic characteristics? Neurology 71(23):1877–1882. https://doi.org/10.1212/01.wnl.0000336651.48596.c7
Braak H, Del Tredici K, Rüb U, De Vos RAI, Jansen Steur ENH, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24(2):197–211. https://doi.org/10.1016/S0197-4580(02)00065-9
Croy I, Nordin S, Hummel T (2014) Olfactory disorders and quality of life-an updated review. Chem Senses 39(3):185–194. https://doi.org/10.1093/chemse/bjt072
Deems DA, Doty RL, Settle RG, Moore-Gillon V, Shaman P, Mester AF, Kimmelman CP, Brightman VJ, Snow JB (1991) Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg 117:519–528. https://doi.org/10.1001/archotol.1991.01870170065015
Soudry Y, Lemogne C, Malinvaud D, Consoli SM, Bonfils P (2011) Olfactory system and emotion: common substrates. Eur Ann Otorhinolaryngol Head Neck Dis 128(1):18–23. https://doi.org/10.1016/j.anorl.2010.09.007
Péron J, Dondaine T, Le Jeune F, Grandjean D, Vérin M (2012) Emotional processing in parkinson’s disease: a systematic review. Mov Disord 27(2):186–199. https://doi.org/10.1002/mds.24025
Bohnen NI, Kaufer DI, Hendrickson R, Constantine GM, Mathis CA, Moore RY (2007) Cortical cholinergic denervation is associated with depressive symptoms in Parkinson’s disease and parkinsonian dementia. J Neurol Neurosurg Psychiatry 78(6):641–643. https://doi.org/10.1136/jnnp.2006.100073
Fullard ME, Tran B, Xie SX, Toledo JB, Scordia C, Linder C, Purri R, Weintraub D, Duda JE, Chahine LM, Morley JF (2016) Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord 25:45–51. https://doi.org/10.1016/j.parkreldis.2016.02.013
Postuma R, Gagnon JF (2010) Cognition and olfaction in Parkinson’s disease. Brain 133(12):1–2. https://doi.org/10.1093/brain/awq225
Stephenson R, Houghton D, Sundarararjan S, Doty RL, Stern M, Xie SX, Siderowf A (2010) Odor identification deficits are associated with increased risk of neuropsychiatric complications in patients with Parkinson’s disease. Mov Disord 25(13):2099–2104. https://doi.org/10.1002/mds.23234
Cramer CK, Friedman JH, Amick MM (2010) Olfaction and apathy in Parkinson’s disease. Parkinsonism Relat Disord 16(2):124–126. https://doi.org/10.1016/j.parkreldis.2009.09.004
Hong JY, Sunwoo MK, Ham JH, Lee JJ, Lee PH, Sohn YH (2015) Apathy and olfactory dysfunction in early Parkinson’s disease. J Mov Disord 8(1):21–25. https://doi.org/10.14802/jmd.14029
Morley JF, Weintraub D, Mamikonyan E, Moberg PJ, Siderowf AD, Duda JE (2011) Olfactory dysfunction is associated with neuropsychiatric manifestations in Parkinson’s disease. Mov Disord 26(11):2051–2057. https://doi.org/10.1002/mds.23792
Doty RL, Deems DA, Stellar S (1988) Olfactory dysfunction in parkinsonism: a general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology 38(8):1237–1244. https://doi.org/10.1212/WNL.38.8.1237
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56(1):33–39. https://doi.org/10.1001/archneur.56.1.33
Litvan I, Bhatia KP, Burn DJ, Goetz CG, Lang AE, McKeith I, Quinn N, Sethi KD, Shults C, Wenning GK (2003) Movement disorders society scientific issues committee report: SIC task force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord 18(5):467–486. https://doi.org/10.1002/mds.10459
Hoehn MM, Yahr MD (1998) Parkinsonism: onset, progression, and mortality. Neurology 50(2):318–318. https://doi.org/10.1212/WNL.50.2.318
Fahn S, Elton R and Members of the UPDRS Development Committee (1987) The Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB and Goldstein M (eds) Recent Developments in Parkinson’s Disease, vol. 2, McMellam Health Care Information, Florham Park, pp 153–163
Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G (1997) “Sniffin” sticks’. Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22(1):39–52. https://doi.org/10.1093/chemse/22.1.39
Hummel T, Kobal G, Gudziol H, Mackay-Sim A (2007) Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3000 subjects. Eur Arch Otorhinolaryngol Suppl 264(3):237–243. https://doi.org/10.1007/s00405-006-0173-0
Masala C, Saba L, Cecchini MP, Solla P, Loy F (2017) Olfactory function and age: a Sniffin’ Sticks extended test study performed in Sardinia. Chemosensory Percept. https://doi.org/10.1007/s12078-017-9233-7
Conti S, Bonazzi S, Laiacona M, Masina M, Coralli MV (2015) Montreal Cognitive Assessment (MoCA)-Italian version: regression based norms and equivalent scores. Neurol Sci 36(2):209–214. https://doi.org/10.1007/s10072-014-1921-3
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Kluger BM, Pedersen KF, Tysnes OB, Ongre SO, Øygarden B, Herlofson K (2017) Is fatigue associated with cognitive dysfunction in early Parkinson’s disease? Parkinsonism Relat Disord 37:87–91. https://doi.org/10.1016/j.parkreldis.2017.02.005
Brown RG, Dittner A, Findley L, Wessely SC (2005) The Parkinson Fatigue Scale. Parkinsonism Relat Disord 11(1):49–55. https://doi.org/10.1016/j.parkreldis.2004.07.007
Haehner A, Hummel T, Reichmann H (2011) Olfactory loss in Parkinson’s disease. Parkinsons Dis 2011:450939. https://doi.org/10.4061/2011/450939
Haehner A, Hummel T, Reichmann H (2014) A clinical approach towards smell loss in Parkinson’s disease. J Parkinsons Dis 4(2):189–195. https://doi.org/10.3233/JPD-130278
Doty RL (2012) Olfaction in Parkinson’s disease and related disorders. Neurobiol Dis 46(3):527–552. https://doi.org/10.1016/j.nbd.2011.10.026
Hummel T, Nordin S (2005) Olfactory disorders and their consequences for quality of life. Acta Otolaryngol 125(2):116–121. https://doi.org/10.1080/00016480410022787
Politis M, Wu K, Molloy S, Bain PG, Chaudhuri KR, Piccini P (2010) Parkinson’s disease symptoms: the patient’s perspective. Mov Disord 25(11):1646–1651. https://doi.org/10.1002/mds.23135
Hurt CS, Alkufri F, Brown RG, Burn DJ, Hindle JV, Landau S, Wilson KC, Samuel M; PROMS-PD study group (2014) Cognition, coping, and outcome in Parkinson’s disease. J Parkinsons Dis 4(2):245–254. https://doi.org/10.3233/JPD-130314
Opara JA, Brola W, Leonardi M, Błaszczyk B (2012) Quality of life in Parkinson’s disease. J Med Life 5(4):375–381
Hawkes CH, Del Tredici K, Braak H (2010) A timeline for Parkinson’s disease. Parkinsonism Relat Disord 16(2):79–84. https://doi.org/10.1016/j.parkreldis.2009.08.007
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386(9996):896–912. https://doi.org/10.1016/S0140-6736(14)61393-3
Pearce RKB, Hawkes CH, Daniel SE (1995) The anterior olfactory nucleus in Parkinson’ s disease. Mov Disord 10(3):283–287
Cheng W, Rolls ET, Gu H, Zhang J, Feng J (2015) Autism: reduced connectivity between cortical areas involved in face expression, theory of mind, and the sense of self. Brain 138(5):1382–1393. https://doi.org/10.1093/brain/awv051
Wang J, Eslinger PJ, Smith MB, Yang QX (2005) Functional magnetic resonance imaging study of human olfaction and normal aging. J Gerontol A Biol Sci Med Sci 60(4):510–514. https://doi.org/10.1093/gerona/60.4.510
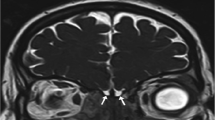
Wu X, Yu C, Fan F, Zhang K, Zhu C, Wu T, Li K, Chan P (2011) Correlation between progressive changes in piriform cortex and olfactory performance in early Parkinson’s disease. Eur Neurol 66(2):98–105. https://doi.org/10.1159/000329371
Herting B, Schulze S, Reichmann H, Haehner A, Hummel T (2008) A longitudinal study of olfactory function in patients with idiopathic Parkinson’s disease. J Neurol 255(3):367–370. https://doi.org/10.1007/s00415-008-0665-5
Müller NG, Machado L, Knight RT (2002) Contributions of Subregions of the prefrontal cortex to working memory: evidence from brain lesions in humans. J Cogn Neurosci 14(5):673–686. https://doi.org/10.1162/08989290260138582
Altinayar S, Oner S, Can S, Kizilay A, Kamisli S, Sarac K (2014) Olfactory disfunction and its relation olfactory bulb volume in Parkinson’s disease. Eur Rev Med Pharmacol Sci 18(23):3659–3664
Mueller A, Abolmaali ND, Hakimi AR, Gloeckler T, Herting B, Reichmann H, Hummel T (2005) Olfactory bulb volumes in patients with idiopathic Parkinson’s disease a pilot study. J Neural Transm (Vienna) 112(10):1363–1370. https://doi.org/10.1007/s00702-005-0280-x
Paschen L, Schmidt N, Wolff S, Cnyrim C, van Eimeren T, Zeuner KE, Deuschl G, Witt K (2015) The olfactory bulb volume in patients with idiopathic Parkinson’s disease. Eur J Neurol 22(7):1068–1073. https://doi.org/10.1111/ene.12709
Huisman E, Uylings HBM, Hoogland PV (2004) A 100% increase of dopaminergic cells in the olfactory bulb may explain hyposmia in Parkinson’s Disease. Mov Disord 19:687–692. https://doi.org/10.1002/mds.10713
Iannilli E (2017) Olfactory impairment in Parkinson’ s disease is a consequence of central nervous system decline. J Neurol 264(6):1236–1246. https://doi.org/10.1007/s00415-017-8521-0
Morley J, Weintraub D, Mamikonyan E, Moberg PJ, Siderowf AD, Duda JE (2011) Olfactory dysfunction is associated with neuropsychiatric manifestations in Parkinson’s disease. Mov Disord 26(11):2051–2057
Blonder LX, Slevin JT (2011) Emotional dysfunction in Parkinson’s disease. Behav Neurol 24(3):201–217. https://doi.org/10.3233/BEN-2011-0329
Pont-Sunyer C, Hotter A, Gaig C, Seppi K, Compta Y, Katzenschlager R et al, Tolosa E (2015) The onset of nonmotor symptoms in parkinson’s disease (the onset pd study). Mov Disord 30(2):229–237. https://doi.org/10.1002/mds.26077
Tolosa E, Gaig C, Santamaría J, Compta Y (2009) Diagnosis and the premotor phase of Parkinson disease. Neurology 17(7):S12-20. https://doi.org/10.1212/WNL.0b013e318198db11 72) .
Schrag A (2006) Quality of life and depression in Parkinson’s disease. J Neurol Sci 248(1–2):151–157. https://doi.org/10.1016/j.jns.2006.05.030
Rickards H (2005) Depression in neurological disorders: Parkinson’s disease, multiple sclerosis, and stroke. J Neurol Neurosurg Psychiatry 76(1):i48–i52. https://doi.org/10.1136/jnnp.2004.060426
Acknowledgements
The authors thank Dr Alan Moat for improving the English text, Dr Raffaella Piras for collecting data and all the participants for their availability. This work was supported by a grant from the University of Cagliari (Progetti di Ricerca di Interesse Dipartimentale, PRID 2017).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the local Ethics Committee (Prot. NP/2016/4523) and was performed according to the Declaration of Helsinki.
Informed consent
Participants received an explanatory statement and gave their written informed consent to participate in the study.
Rights and permissions
About this article
Cite this article
Masala, C., Solla, P., Liscia, A. et al. Correlation among olfactory function, motors’ symptoms, cognitive impairment, apathy, and fatigue in patients with Parkinson’s disease. J Neurol 265, 1764–1771 (2018). https://doi.org/10.1007/s00415-018-8913-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8913-9