Abstract
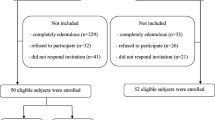
Parkinson’s disease is characterized by rigidity, akinesia and tremor, all of which interfere with automated small hand movements potentially affecting oral care. In addition, medication and craving for sweets are other risk factors for dental and periodontal disease in these patients. Here, we report the Community Periodontal Index for Treatment Needs (CPITN) data in 70 patients with Parkinson’s disease and 85 agematched control subjects. CPITN indices were assessed in all 6 sextants. Mean CPITN indices of control subjects ranged from 1.6 ± 0.2 in the upper frontal sextant to 2.5 ± 0.2 in the upper left lateral sextant. 17.9% of controls showed severely affected teeth (CPITN code 4) in the upper left or upper right sextant, while there were no teeth at risk in the upper frontal sextant. Patients suffering from Parkinson’s disease, however, had a markedly increased mean CPITN index in the upper frontal sextant (2.4 ± 0.2) with 11.5 patients having severely affected teeth (CPITN code 4). CPITN indices in all other sextants were less severely increased. Overall, there was a significant difference between mean CPITN indices of patients and controls (p < 0.05). It seems also noteworthy that female controls had lower CPITN indices in all sextants compared with male controls. This gender difference, however, was reversed in Parkinson’s patients. We believe that problems in oral hygiene contribute to this increased periodontal pathology in patients with Parkinson’s disease, which may further compromise the quality of life.
Similar content being viewed by others
References
Ahrens G, Bublitz KA (1987) Periodontal diseases and treatment needs of the population of Hamburg, An epidemiological study with 11305 probands. Dtsch Zahnarztl Z 42:433–437
Anastassiadou V, Katsarou Z, Naka O, Bostanzopoulou M (2002) Evaluating dental status and prosthetic need in relation to medical findings in Greek patients suffering from idiopathic Parkinson’s disease. Eur J Prosthodont Restor Dent 10:63–68
Chu FC, Deng FL, Siu AS, Chow TW (2004) Implant-tissue supported, magnet-retained mandibular overdenture for an edentulous patient with Parkinson’s disease: a clinical report. J Prosthet Dent 91:219–222
Contreras-Vidal JL, Teulings HL, Stelmach GE (1995) Micrographia in Parkinson’s disease. Neuroreport 6:2089–2092
Eichhorn TE, Gasser T, Mai N, Marquardt C, Arnold G, Schwarz J, Oertel WH (1996) Computational analysis of open loop handwriting movements in Parkinson’s disease: a rapid method to detect dopamimetic effects. Mov Disord 11:289–297
Fukayo S, Nonaka K, Shimizu T, Yano E (2003) Oral health of patients with Parkinson’s disease: factors related to their better dental status. Tohoku J Exp Med 201:171–179
Heckmann SM, Heckmann JG, Weber HP (2000) Clinical outcomes of three Parkinson’s disease patients treated with mandibular implant overdentures. Clin Oral Implants Res 11:566–571
Herren C, Abadi B (2005) Urgent denture repair in a medically compromised patient. Gen Dent 53:60–62
Hughes AJ, Daniel SE, Ben-Shlomo Y, Lees AJ (2002) The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain 125:861–870
Kennedy MA, Rosen S, Paulson GW, Jolly DE, Beck FM (1994) Relationship of oral microflora with oral health status in Parkinson’s disease. Spec Care Dentist 14:164–168
Kubo K, Kimura K (2004) Implant surgery for a patient with Parkinson’s disease controlled by intravenous midazolam: a case report. Int J Oral Maxillofac Implants 19:288–290
Marras C, Lang A, Krahn M, Tomlinson G, Naglie G (2004) Quality of life in early Parkinson’s disease: impact of dyskinesias and motor fluctuations. Mov Disord 19:22–28
Michels LF (1984) A case of high caries activity in a patient treated for Parkinson disease. Ned Tijdschr Tandheelkd 91:328
Nakayama Y, Washio M, Mori M (2004) Oral health conditions in patients with Parkinson’s disease. J Epidemiol 14:143–150
Quittenbaum BH, Grahn B (2004) Quality of life and pain in Parkinson’s disease: a controlled cross-sectional study. Parkinsonism Relat Disord 10:129–136
Shimada A, Sasaki Y, Mataki S (2005) An evaluation of self-reported oral health and health-related quality of life. J Med Dent Sci 52:65–72
Van Palenstein Helderman WH, Beijn W (1983) A case report of high caries activity due to the drug therapy in Parkinson’s disease, The problem of dry mouth–xerostomia. Ned Tijdschr Tandheelkd 90:545–550
Weintraub D, Moberg PJ, Duda JE, Katz IR, Stern MB (2004) Effect of psychiatric and other nonmotor symptoms on disability in Parkinson’s disease. J Am Geriatr Soc 52:784–788
Welsh M (2004) Parkinson’s disease and quality of life: issues and challenges beyond motor symptoms. Neurol Clin 22:S141–S148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schwarz, J., Heimhilger, E. & Storch, A. Increased periodontal pathology in Parkinson's disease. J Neurol 253, 608–611 (2006). https://doi.org/10.1007/s00415-006-0068-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0068-4