Abstract
Purpose
Intravenous lidocaine infusion has been used for postoperative analgesia in many surgical procedures in recent years. The aim of this randomized, double-blind study was to investigate the postoperative analgesic efficacy of perioperative intravenous lidocaine infusion in patients undergoing septorhinoplasty surgery.
Materials and methods
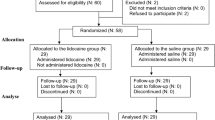
Forty-eight American Society of Anesthesiologists I and II patients, aged 18–40 years scheduled for septorhinoplasty surgery, were assigned into two groups. Before anesthesia induction, patients in the lidocaine group (Group L, n = 24) received an intravenous bolus infusion of 1.5 mg/kg lidocaine followed by a continuous infusion of 1.5 mg/kg/h during the operation and until the end of the first postoperative hour. Patients in the control group (Group C, n = 24) received normal saline according to the same protocol. In the postoperative period, 50 mg dexketoprofen trometamol was administered and repeated every 12 h. Postoperative pain scores, rescue analgesia, intraoperative opioid requirements, and side effects were recorded.
Results
Postoperative pain scores were significantly lower in Group L than in Group C at postoperative 30 min, 1, 2, 4, 8, 12 and 24 h (p < 0.05). There was no difference between groups intraoperative remifentanil consumption (p > 0.05). Rescue analgesia use was statistically significantly higher in Group C than in Group L (12/24 versus 1/24, respectively, p = 0.001). Postoperative nausea was statistically higher in Group C than in Group L (13/24 versus 5/24 respectively, p = 0.017), whereas other side-effects were similar for the two groups (p > 0.05).
Discussion
We recommended the use of intravenous lidocaine infusion for intraoperatively and first postoperative hours in septorhinoplasty surgery as it reduces pain scores and the need for additional opioid use.


Similar content being viewed by others
References
Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10:2287–2298. https://doi.org/10.2147/jpr.s144066
Kim DH, Kang H, Jin HJ, Hwang SH (2019) Effect of piezoelectric osteotomy on postoperative oedema and ecchymosis after rhinoplasty. Clin Otolaryngol. https://doi.org/10.1111/coa.13415
Celik EC, Kara D, Koc E, Yayik AM (2018) The comparison of single-dose preemptive intravenous ibuprofen and paracetamol on postoperative pain scores and opioid consumption after open septorhinoplasty: a randomized controlled study. Eur Arch Otorhinolaryngol 275(9):2259–2263. https://doi.org/10.1007/s00405-018-5065-6
Yayik AM, Yildirim H, Ahiskalioglu A, Sakat MS, Erguney OD, Ahiskalioglu EO, Sulak MM, Celik EC (2019) Effects of bupivacaine versus bupivacaine plus dexamethasone-soaked nasal packing after endoscopic nasal surgery. J Craniofac Surg 30(4):1174–1177. https://doi.org/10.1097/scs.0000000000005227
Sclafani AP, Kim M, Kjaer K, Kacker A, Tabaee A (2019) Postoperative pain and analgesic requirements after septoplasty and rhinoplasty. Laryngoscope 129(9):2020–2025. https://doi.org/10.1002/lary.27913
Gozeler MS, Sakat MS, Kilic K, Ozmen O, Can A, Ince I (2018) Does a single-dose preemptive intravenous ibuprofen have an effect on postoperative pain relief after septorhinoplasty? Am J Otolaryngol 39(6):726–730. https://doi.org/10.1016/j.amjoto.2018.07.023
Estebe JP (2017) Intravenous lidocaine. Best Pract Res Clin Anaesthesiol 31(4):513–521. https://doi.org/10.1016/j.bpa.2017.05.005
Swenson BR, Gottschalk A, Wells LT, Rowlingson JC, Thompson PW, Barclay M, Sawyer RG, Friel CM, Foley E, Durieux ME (2010) Intravenous lidocaine is as effective as epidural bupivacaine in reducing ileus duration, hospital stay, and pain after open colon resection: a randomized clinical trial. Reg Anesth Pain Med 35(4):370–376. https://doi.org/10.1097/AAP.0b013e3181e8d5da
Kuo CP, Jao SW, Chen KM, Wong CS, Yeh CC, Sheen MJ, Wu CT (2006) Comparison of the effects of thoracic epidural analgesia and iv infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth 97(5):640–646. https://doi.org/10.1093/bja/ael217
Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL (2007) Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology 106(1):11–18. https://doi.org/10.1097/00000542-200701000-00007(discussion 15–16)
Lauwick S, Kim DJ, Mistraletti G, Carli F (2009) Functional walking capacity as an outcome measure of laparoscopic prostatectomy: the effect of lidocaine infusion. Br J Anaesth 103(2):213–219. https://doi.org/10.1093/bja/aep103
Choi GJ, Kang H, Ahn EJ, Oh JI, Baek CW, Jung YH, Kim JY (2016) Clinical efficacy of ıntravenous lidocaine for thyroidectomy: a prospective, randomized, double-blind, placebo-controlled trial. World J Surg 40(12):2941–2947. https://doi.org/10.1007/s00268-016-3619-6
Cui W, Li Y, Li S, Wang R, Li J (2010) Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil-based anaesthesia. Eur J Anaesthesiol 27(1):41–46. https://doi.org/10.1097/EJA.0b013e32832d5426
Greenwood E, Nimmo S, Paterson H, Homer N, Foo I (2019) Intravenous lidocaine infusion as a component of multimodal analgesia for colorectal surgery-measurement of plasma levels. Perioper Med (Lond) 8:1. https://doi.org/10.1186/s13741-019-0112-4
Calatayud J, Gonzalez A (2003) History of the development and evolution of local anesthesia since the coca leaf. Anesthesiology 98(6):1503–1508. https://doi.org/10.1097/00000542-200306000-00031
Fredrick DS, Boersma RB (1979) Lidocaine infusions: effect of duration and method of discontinuation on recurrence of arrhythmias and pharmacokinetic variables. Am J Hosp Pharm 36(6):778–781
Masic D, Liang E, Long C, Sterk EJ, Barbas B, Rech MA (2018) Intravenous lidocaine for acute pain: a systematic review. Pharmacotherapy 38(12):1250–1259. https://doi.org/10.1002/phar.2189
Omar E, Wallon G, Bauer C, Axiotis G, Bouix C, Soubirou JL, Aubrun F (2019) Evaluation of intravenous lidocaine in head and neck cancer surgery: study protocol for a randomized controlled trial. Trials 20(1):220. https://doi.org/10.1186/s13063-019-3303-x
Song X, Sun Y, Zhang X, Li T, Yang B (2017) Effect of perioperative intravenous lidocaine infusion on postoperative recovery following laparoscopic cholecystectomy—a randomized controlled trial. Int J Surg 45:8–13. https://doi.org/10.1016/j.ijsu.2017.07.042
Kim TH, Kang H, Hong JH, Park JS, Baek CW, Kim JY, Jung YH, Kim HK (2011) Intraperitoneal and intravenous lidocaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. Surg Endosc 25(10):3183–3190. https://doi.org/10.1007/s00464-011-1684-3
Carabalona JF, Delwarde B, Duclos A, Le Goff MC, Moulsma M, Citterio-Quentin A, Bouffard Y, Rimmele T (2018) Serum concentrations of lidocaine during bariatric surgery. Anesth Analg. https://doi.org/10.1213/ane.0000000000003905
Soto G, Naranjo Gonzalez M, Calero F (2018) Intravenous lidocaine infusion. Rev Esp Anestesiol Reanim 65(5):269–274. https://doi.org/10.1016/j.redar.2018.01.004
Yon JH, Choi GJ, Kang H, Park JM, Yang HS (2014) Intraoperative systemic lidocaine for pre-emptive analgesics in subtotal gastrectomy: a prospective, randomized, double-blind, placebo-controlled study. Can J Surg 57(3):175–182. https://doi.org/10.1503/cjs.009613
Kim KT, Cho DC, Sung JK, Kim YB, Kang H, Song KS, Choi GJ (2014) Intraoperative systemic infusion of lidocaine reduces postoperative pain after lumbar surgery: a double-blinded, randomized, placebo-controlled clinical trial. Spine J 14(8):1559–1566. https://doi.org/10.1016/j.spinee.2013.09.031
Terkawi AS, Sharma S, Durieux ME, Thammishetti S, Brenin D, Tiouririne M (2015) Perioperative lidocaine infusion reduces the incidence of post-mastectomy chronic pain: a double-blind, placebo-controlled randomized trial. Pain Physician 18(2):E139–E146
Dewinter G, Moens P, Fieuws S, Vanaudenaerde B, Van de Velde M, Rex S (2017) Systemic lidocaine fails to improve postoperative morphine consumption, postoperative recovery and quality of life in patients undergoing posterior spinal arthrodesis. A double-blind, randomized, placebo-controlled trial. Br J Anaesth 118(4):576–585. https://doi.org/10.1093/bja/aex038
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of present study declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ates, İ., Aydin, M.E., Ahiskalioglu, A. et al. Postoperative analgesic efficacy of perioperative intravenous lidocaine infusion in patients undergoing septorhinoplasty: a prospective, randomized, double-blind study. Eur Arch Otorhinolaryngol 277, 1095–1100 (2020). https://doi.org/10.1007/s00405-020-05801-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05801-6