Abstract
Purpose
Endoscopic sinus surgery (ESS) is a well-established treatment for chronic rhinosinusitis (CRS). However, ESS for frontal sinusitis remains complicated and challenging. The aim of this study was to identify the relationship between residual frontal recess cells and primary ESS failure in the frontal sinus.
Methods
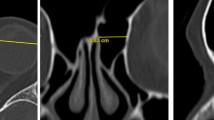
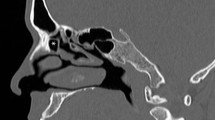
We prospectively collected information on 214 sides of 129 patients with CRS who underwent standard ESS from June 2010 to May 2011. To identify risk factors, we retrospectively analyzed clinical data and computed tomography (CT) images before and 3 months after surgery.
Results
The posterior side of the frontal recess cells remained relatively common: suprabullar cells (SBCs) were found in 12.2% (16 sides), suprabullar frontal cells (SBFCs) in 20.3% (12 sides), and supraorbital ethmoid cells in 23.7% (14 sides). In contrast, the anterior side of the frontal recess cells, agger nasi cells, supra agger cells, and supra agger frontal cells remained at < 10.0%. Frontal septal cells persisted in 25.0% (5 sides). The presence of residual frontal recess cells was an independent risk factor for postoperative frontal sinus opacification as were well-recognized risk factors such as nasal polyps, the peripheral eosinophil count, and the CT score. Among residual frontal recess cells, SBCs and SBFCs were independent risk factors for opacification.
Conclusions
Residual frontal recess cells, especially SBCs and SBFCs, were independent risk factors for postoperative opacification of the frontal sinus. Complete surgical excision of frontal recess cells may improve surgical outcomes.




Similar content being viewed by others
References
Van Alyea OE (1939) Ethmoid labyrinth: anatomic study, with consideration of the clinical significance of its structural characteristics. Arch Otolaryngol 29:881–902
Lund VJ, Stammberger H, Fokkens WJ et al (2014) European position paper on the anatomical terminology of the internal nose and paranasal sinuses. Rhinol Suppl 24:1–34
Wormald PJ, Hoseman W, Callejas C et al (2016) The International Frontal Sinus Anatomy Classification (IFAC) and Classification of the Extent of Endoscopic Frontal Sinus Surgery (EFSS). Int Forum Allergy Rhinol 6:677–696. https://doi.org/10.1002/alr.21738
Orlandi RR, Kennedy DW (2001) Revision endoscopic frontal sinus surgery. Otolaryngol Clin N Am 34:77–90. https://doi.org/10.1016/S0030-6665(05)70296-6
Bassiouni A, Naidoo Y, Wormald PJ (2012) When FESS fails: The inflammatory load hypothesis in refractory chronic rhinosinusitis. Laryngoscope 122:460–466. https://doi.org/10.1002/lary.22461
Valdes CJ, Bogado M, Samaha M (2014) Causes of failure in endoscopic frontal sinus surgery in chronic rhinosinusitis patients. Int Forum Allergy Rhinol 4:502–506. https://doi.org/10.1002/alr.21307
Ramadan HH (1999) Surgical causes of failure in endoscopic sinus surgery. Laryngoscope 109:27–29. https://doi.org/10.1097/00005537-199901000-00006
Bradley DT, Kountakis SE (2004) The role of agger nasi air cells in patients requiring revision endoscopic frontal sinus surgery. Otolaryngol Head Neck Surg 131:525–527. https://doi.org/10.1016/j.otohns.2004.03.038
Musy PY, Kountakis SE (2004) Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol 25:418–422. https://doi.org/10.1016/j.amjoto.2004.06.002
Otto KJ, DelGaudio JM (2010) Operative findings in the frontal recess at time of revision surgery. Am J Otolaryngol 31:175–180. https://doi.org/10.1016/j.amjoto.2008.12.006
Okushi T, Mori E, Nakayama T et al (2012) Impact of residual ethmoid cells on postoperative course after endoscopic sinus surgery for chronic rhinosinusitis. Auris Nasus Larynx 39:484–489. https://doi.org/10.1016/j.anl.2011.09.001
Asaka D, Nakayama T, Hama T et al (2011) Risk factors for complications of endoscopic sinus surgery for chronic rhinosinusitis. Am J Rhinol Allergy 26:61–64. https://doi.org/10.2500/ajra.2012.26.3711
Fokkens WJ, Lund VJ, Mullol J et al (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 23:3 (preceding table of contents 1–298)
Orlandi RR, Kingdom TT, Hwang PH et al (2016) International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 6(Suppl 1):S22–S209. https://doi.org/10.1002/alr.21695
Moriyama H (2001) Endoscopic modification of the Takahashi technique. In: Kennedy DW (ed) Diseases of the sinuses: diagnosis and management. B.C. Decker Inc, London, pp 235–244
Moriyama H (1991) The technique of endoscopic surgery and diagnosis of frontal recess and sinus disease under local anesthesia. J Otolaryngol 20:382–384
Okushi T, Yoshikawa M, Otori N et al (2012) Evaluation of symptoms and QOL with calcium alginate versus chitin-coated gauze for middle meatus packing after endoscopic sinus surgery. Auris Nasus Larynx 39:31–37. https://doi.org/10.1016/j.anl.2011.02.008
Moriyama H, Yanagi K, Ohtori N, Fukami M (1995) Evaluation of endoscopic sinus surgery for chronic sinusitis: post-operative erythromycin therapy. Rhinology 33:166–170
Kennedy DW, Kuhn FA, Hamilos DL et al (2005) Treatment of chronic rhinosinusitis with high-dose oral terbinafine: a double blind, placebo-controlled study. Laryngoscope 115:1793–1799. https://doi.org/10.1097/01.mlg.0000175683.81260.26
Okushi T, Nakayama T, Morimoto S et al (2013) A modified Lund-Mackay system for radiological evaluation of chronic rhinosinusitis. Auris Nasus Larynx 40:548–553. https://doi.org/10.1016/j.anl.2013.04.010
Goldstein GH, Kennedy DW (2013) Long-term successes of various sinus surgeries: a comprehensive analysis. Curr Allergy Asthma Rep 13:244–249. https://doi.org/10.1007/s11882-012-0336-6
Matsuwaki Y, Ookushi T, Asaka D et al (2008) Chronic rhinosinusitis: risk factors for the recurrence of chronic rhinosinusitis based on 5-year follow-up after endoscopic sinus surgery. Int Arch Allergy Immunol 146(Suppl 1):77–81. https://doi.org/10.1159/000126066
Nakayama T, Yoshikawa M, Asaka D et al (2011) Mucosal eosinophilia and recurrence of nasal polyps—new classification of chronic rhinosinusitis. Rhinology 49:3–396. https://doi.org/10.4193/Rhino10.261
Tokunaga T, Sakashita M, Haruna T et al (2015) Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 70:995–1003. https://doi.org/10.1111/all.12644
Batra PS, Tong L, Citardi MJ (2013) Analysis of comorbidities and objective parameters in refractory chronic rhinosinusitis. Laryngoscope 123 Suppl 7:S1–S11. https://doi.org/10.1002/lary.24418
Gregurić T, Trkulja V, Baudoin T et al (2017) Association between computed tomography findings and clinical symptoms in chronic rhinosinusitis with and without nasal polyps. Eur Arch Otorhinolaryngol 274:2165–2173. https://doi.org/10.1007/s00405-016-4446-y
Friedman M, Bliznikas D, Vidyasagar R et al (2006) Long-term results after endoscopic sinus surgery involving frontal recess dissection. Laryngoscope 116:573–579. https://doi.org/10.1097/01.MLG.0000202086.18206.C8
Acknowledgements
We thank Angela Morben, DVM, ELS, from Edanz Group (http://www.edanzediting.com/ac), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest relevant to this report.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Nakayama, T., Asaka, D., Kuboki, A. et al. Impact of residual frontal recess cells on frontal sinusitis after endoscopic sinus surgery. Eur Arch Otorhinolaryngol 275, 1795–1801 (2018). https://doi.org/10.1007/s00405-018-5003-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5003-7