Abstract
Purpose
To estimate the risk of shoulder dystocia (SD) in pregnancies with/without maternal diabetes or obesity; to identify antenatal maternal and fetal ultrasound-derived risk factors and calculate their contributions.
Methods
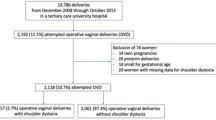
A multicenter retrospective analysis of 13,428 deliveries in three tertiary hospitals (2014–2017) with fetal ultrasound data ≤ 14 days prior to delivery (n = 7396). Inclusion criteria: singleton pregnancies in women ≥ 18 years old; vertex presentation; vaginal delivery at ≥ 37 weeks of gestation. Estimated fetal weight (EFW) and birth weight (BW) were categorized by steps of 250 g. To evaluate risk factors, a model was performed using ultrasound data with SD as the dependent variable.
Results
Diabetes was present in 9.3%; BMI ≥ 30 kg/m2 in 10.4% and excessive weight gain in 39.8%. The total SD rate was 0.9%, with diabetes 2.0% and with obesity 1.9%. These increased with BW 4250–4499 g compared to 4000–4249 g in women with diabetes (12.1% vs 1.9%, P = 0.010) and without (6.1% vs 1.6%, P < 0.001) and at the same BW threshold for women with obesity (9.6% vs 0.6%, P = 0.002) or without (6.4% vs 1.8%, P < 0.001). Rates increased similarly for EFW at 4250 g and for AC–HC at 2.5 cm. Independent risk factors for SD were EFW ≥ 4250 g (OR 3.8, 95% CI 1.5–9.4), AC–HC ≥ 2.5 cm (OR 3.1, 95% CI 1.3–7.5) and diabetes (OR 2.2, 95% CI 1.2–4.0). HC/AC ratio, obesity, excessive weight gain and labor induction were not significant.
Conclusion
Independent of diabetes, which remains a risk factor for SD, a significant increase may be expected if the EFW is ≥ 4250 g and AC–HC is ≥ 2.5 cm.


Similar content being viewed by others
Availability of data and material
The data that support the findings of the study are available on reasonable request from the corresponding author.
Code availability
IBM SPSS Statistics Version 25.0 (Armonk, NY, USA).
References
Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM (2006) Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol 195(3):657–672. https://doi.org/10.1016/j.ajog.2005.09.007
Overland EA, Vatten LJ, Eskild A (2014) Pregnancy week at delivery and the risk of shoulder dystocia: a population study of 2,014,956 deliveries. Br Int J Obstet Gynaecol (BJOG) 121(1):34–41. https://doi.org/10.1111/1471-0528.12427
Committee on Practice Bulletins—Obstetrics (2017) Practice bulletin no 178: shoulder dystocia. Obstet Gynecol 129(5):e123–e133. https://doi.org/10.1097/aog.0000000000002043
Michelotti F, Flatley C, Kumar S (2018) Impact of shoulder dystocia, stratified by type of manoeuvre, on severe neonatal outcome and maternal morbidity. Aust N Z J Obstet Gynaecol 58(3):298–305. https://doi.org/10.1111/ajo.12718
Tsur A, Sergienko R, Wiznitzer A, Zlotnik A, Sheiner E (2012) Critical analysis of risk factors for shoulder dystocia. Arch Gynecol Obstet 285(5):1225–1229. https://doi.org/10.1007/s00404-011-2139-8
Chauhan SP, Laye MR, Lutgendorf M, McBurney JW, Keiser SD, Magann EF, Morrison JC (2014) A multicenter assessment of 1177 cases of shoulder dystocia: lessons learned. Am J Perinatol 31(5):401–406. https://doi.org/10.1055/s-0033-1350056
Gherman RB (2002) Shoulder dystocia: an evidence-based evaluation of the obstetric nightmare. Clin Obstet Gynecol 45(2):345–362
Ouzounian JG (2016) Shoulder dystocia: incidence and risk factors. Clin Obstet Gynecol 59(4):791–794. https://doi.org/10.1097/grf.0000000000000227
Acker DB, Sachs BP, Friedman EA (1985) Risk factors for shoulder dystocia. Obstet Gynecol 66(6):762–768
Dodd JM, Catcheside B, Scheil W (2012) Can shoulder dystocia be reliably predicted? Aust N Z J Obstet Gynaecol 52(3):248–252. https://doi.org/10.1111/j.1479-828X.2012.01425.x
Santos P, Hefele JG, Ritter G, Darden J, Firneno C, Hendrich A (2018) Population-based risk factors for shoulder dystocia. J Obstet Gynecol Neonatal Nurs 47(1):32–42. https://doi.org/10.1016/j.jogn.2017.11.011
Zhang C, Wu Y, Li S, Zhang D (2018) Maternal prepregnancy obesity and the risk of shoulder dystocia: a meta-analysis. Br Int J Obstet Gynaecol (BJOG) 125(4):407–413. https://doi.org/10.1111/1471-0528.14841
Hill MG, Cohen WR (2016) Shoulder dystocia: prediction and management. Womens Health (Lond) 12(2):251–261. https://doi.org/10.2217/whe.15.103
Robson M (2019) Shoulder dystocia: Is it time to think differently? Aust N Z J Obstet Gynaecol 59(5):605–607. https://doi.org/10.1111/ajo.13060
Langer O, Berkus MD, Huff RW, Samueloff A (1991) Shoulder dystocia: should the fetus weighing greater than or equal to 4000 grams be delivered by cesarean section? Am J Obstet Gynecol 165(4 Pt 1):831–837
Institute of M, National Research Council Committee to Reexamine IOMPWG (2009) The national academies collection: reports funded by national institutes of health. In: Rasmussen KM, Yaktine AL (eds) Weight gain during pregnancy: reexamining the guidelines. National Academies Press (US) National Academy of Sciences, Washington. https://doi.org/10.17226/12584
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva A, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Voigt M, Rochow N, Schneider KT, Hagenah HP, Scholz R, Hesse V, Wittwer-Backofen U, Straube S, Olbertz D (2014) New percentile values for the anthropometric dimensions of singleton neonates: analysis of perinatal survey data of 2007–2011 from all 16 states of Germany. Z Geburtshilfe Neonatol 218(5):210–217. https://doi.org/10.1055/s-0034-1385857
Landmann E, Reiss I, Misselwitz B, Gortner L (2006) Ponderal index for discrimination between symmetric and asymmetric growth restriction: percentiles for neonates from 30 weeks to 43 weeks of gestation. J Matern Fetal Neonatal Med 19(3):157–160. https://doi.org/10.1080/14767050600624786
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK (1985) Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol 151(3):333–337. https://doi.org/10.1016/0002-9378(85)90298-4
Snijders RJ, Nicolaides KH (1994) Fetal biometry at 14–40 weeks’ gestation. Ultrasound Obstet Gynecol 4(1):34–48. https://doi.org/10.1046/j.1469-0705.1994.04010034.x
Duryea EL, Casey BM, McIntire DD, Twickler DM (2017) The FL/AC ratio for prediction of shoulder dystocia in women with gestational diabetes. J Matern Fetal Neonatal Med 30(19):2378–2381. https://doi.org/10.1080/14767058.2016.1249842
Secher AL, Bytoft B, Tabor A, Damm P, Mathiesen ER (2015) Fetal sonographic characteristics associated with shoulder dystocia in pregnancies of women with type 1 diabetes. Acta Obstet Gynecol Scand 94(10):1105–1111. https://doi.org/10.1111/aogs.12707
Burkhardt T, Schmidt M, Kurmanavicius J, Zimmermann R, Schaffer L (2014) Evaluation of fetal anthropometric measures to predict the risk for shoulder dystocia. Ultrasound Obstet Gynecol 43(1):77–82. https://doi.org/10.1002/uog.12560
Robinson R, Walker KF, White VA, Bugg GJ, Snell KIE, Jones NW (2020) The test accuracy of antenatal ultrasound definitions of fetal macrosomia to predict birth injury: a systematic review. Eur J Obstet Gynecol Reprod Biol 246:79–85. https://doi.org/10.1016/j.ejogrb.2020.01.019
Endres L, DeFranco E, Conyac T, Adams M, Zhou Y, Magner K, O’Rourke L, Bernhard KA, Siddiqui D, McCormick A, Abramowicz J, Merkel R, Jawish R, Habli M, Floman A, Magann EF, Chauhan SP (2015) Association of fetal abdominal-head circumference size difference with shoulder dystocia: a multicenter study. AJP Rep 5(2):e099-104. https://doi.org/10.1055/s-0035-1548544
Ashwal E, Berezowsky A, Orbach-Zinger S, Melamed N, Aviram A, Hadar E, Yogev Y, Hiersch L (2018) Birthweight thresholds for increased risk for maternal and neonatal morbidity following vaginal delivery: a retrospective study. Arch Gynecol Obstet 298(6):1123–1129. https://doi.org/10.1007/s00404-018-4924-0
Ehrenberg HM, Mercer BM, Catalano PM (2004) The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol 191(3):964–968. https://doi.org/10.1016/j.ajog.2004.05.052
Feghali MN, Catov JM, Zantow E, Mission J, Caritis SN, Scifres CM (2019) Timing of gestational weight gain and adverse perinatal outcomes in overweight and obese women. Obstet Gynecol 133(5):962–970. https://doi.org/10.1097/aog.0000000000003234
Maresh MJ, Holmes VA, Patterson CC, Young IS, Pearson DW, Walker JD, McCance DR (2015) Glycemic targets in the second and third trimester of pregnancy for women with type 1 diabetes. Diabetes Care 38(1):34–42. https://doi.org/10.2337/dc14-1755
Doty MS, Al-Hafez L, Chauhan SP (2016) Sonographic examination of the fetus vis-à-vis shoulder dystocia: a vexing promise. Clin Obstet Gynecol 59(4):795–802. https://doi.org/10.1097/grf.0000000000000241
Tsur A, Batsry L, Toussia-Cohen S, Rosenstein MG, Barak O, Brezinov Y, Yoeli-Ullman R, Sivan E, Sirota M, Druzin ML, Stevenson DK, Blumenfeld YJ, Aran D (2019) Development and validation of a machine learning model for prediction of shoulder dystocia. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.21878
Palatnik A, Grobman WA, Hellendag MG, Janetos TM, Gossett DR, Miller ES (2016) Predictors of shoulder dystocia at the time of operative vaginal delivery. Am J Obstet Gynecol 215(5):624.e621-624.e625. https://doi.org/10.1016/j.ajog.2016.06.001
Acknowledgements
We would like to thank the team of midwives, nurses and physicians from the three participating obstetrics wards for their support in caring for pregnant women and recording clinical data.
Funding
The authors did not receive any funding for the present work.
Author information
Authors and Affiliations
Contributions
JV study design, data collection, data analysis, interpretation of study findings, manuscript writing and editing. CAED data analysis and interpretation, manuscript editing. LD, HV data collection, manuscript editing. CK, WH, BR, DS, MA-D manuscript editing. MJAM interpretation of study findings, manuscript editing. UMS-G study design, data analysis, interpretation of study findings, manuscript editing. All authors approved the final draft for publication.
Corresponding author
Ethics declarations
Conflict of interest
UMS-G received remuneration for lectures by pharmaceutical companies (Novo Nordisk, Berlin-Chemie, Sanofi-Aventis). MJAM received an honorarium from Novo Nordisk for chairing the Drug Monitoring Committee on a trial comparing two of their long-acting insulins in type 1 diabetes. The remaining authors report no conflict of interest. The contributing authors are solely responsible for the content of the manuscript.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki and received ethical approval (Eth-33/16 Berlin Medical Association).
Consent to participate
The need for individual written consent was waived by the local Ethics Committee of Berlin Medical Association in view of the retrospective nature of the study. All data were stored and analyzed anonymously.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vetterlein, J., Doehmen, C.A.E., Voss, H. et al. Antenatal risk prediction of shoulder dystocia: influence of diabetes and obesity: a multicenter study. Arch Gynecol Obstet 304, 1169–1177 (2021). https://doi.org/10.1007/s00404-021-06041-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06041-7