Abstract
Objective
The study was aimed to define trends, risk factors and perinatal outcome associated with shoulder dystocia (SD).
Methods
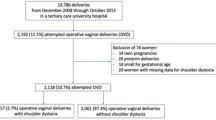
A population-based study comparing all singleton deliveries with and without SD was conducted. Statistical analysis was performed using multiple logistic regression analysis.
Results
Shoulder dystocia complicated 0.2% (n = 451) of all deliveries included in the study (n = 240,189). The rate of SD declined from 0.4% in 1988 to 0.13% in 2009. Independent risk factors for SD in a multivariable analysis were fetal macrosomia (birth-weight ≥ 4 kg; OR = 16.1; 95% CI 13.2–19.6, P < 0.001), failure of labor to progress during the second stage (OR = 2.4; 95% CI 1.5–3.7, P < 0.001), diabetes mellitus (OR = 1.8; 95% CI 1.4–2.3, P < 0.001) and advanced maternal age (years, OR = 1.02; 95% CI 1.001–1.03, P = 0.029). Perinatal mortality was significantly higher after SD as compared to the comparison group (6.2 vs. 1.4%, P <0.001). Another multivariable analysis, with perinatal mortality as the outcome variable, controlling for confounders such as maternal age, gestational age, diabetes mellitus, etc. was constructed; SD was noted as an independent risk factor for perinatal mortality (adjusted OR = 11.1; 95% CI 7.2–17.1, P < 0.001).
Conclusions
Shoulder dystocia, associated with macrosomia, labor dystocia, diabetes mellitus, and advanced maternal age, is an independent risk factor for perinatal mortality. In an era of increased rate of cesarean deliveries, and perhaps increased accuracy of birth weight estimation, the rate of shoulder dystocia gradually declines.

Similar content being viewed by others
References
Sokol RJ, Blackwell SC (2003) American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. ACOG practice bulletin: Shoulder dystocia. Number 40, November 2002. (Replaces practice pattern number 7, October 1997). Int J Gynaecol Obstet 80(1):87–92
Gottlieb AG, Galan HL (2007) Shoulder dystocia: an update. Obstet Gynecol Clin North Am 34(3):501–531
Gherman RB (2002) Shoulder dystocia: an evidence-based evaluation of the obstetric nightmare. Clin Obstet Gynecol 45(2):345–362
McFarland MB, Langer O, Piper JM, Berkus MD (1996) Perinatal outcome and the type and number of maneuvers in shoulder dystocia. Int J Gynaecol Obstet 55(3):219–224
Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH (1997) The McRoberts’ maneuver for the alleviation of shoulder dystocia: how successful is it? Obstet Gynecol 176(3):656–661
Gherman RB (2005) Shoulder dystocia: prevention and management. Obstet Gynecol Clin North Am 32(2):297–305
Sheiner E, Levy A, Hershkovitz R, Hallak M, Hammel RD, Katz M, Mazor M (2004) Determining factors associated with shoulder dystocia: a population-based study. Eur J Obstet Gynecol Reprod Biol 126(1):11–15
Ginsberg NA, Moisidis C (2001) How to predict recurrent shoulder dystocia. Obstet Gynecol 184(7):1427–1430
Bingham J, Chauhan SP, Hayes E, Gherman R, Lewis D (2010) Recurrent shoulder dystocia: a review. Obstet Gynecol Surv 65(3):183
Poggi SH, Stallings SP, Ghidini A, Spong CY, Deering SH, Allen RH (2003) Intrapartum risk factors for permanent brachial plexus injury. Obstet Gynecol 189(3):725–729
Gemer O, Bergman M, Segal S (1999) Labor abnormalities as a risk factor for shoulder dystocia. Acta Obstet Gynecol Scand 78(8):735
Inglis SR, Feier N, Chetiyaar JB, Naylor MH, Sumersille M, Cervellione KL, Predanic M (2011) Effects of shoulder dystocia training on the incidence of brachial plexus injury. Obstet Gynecol 204(4):322
Levy A, Sheiner E, Hammel RD, Hershkovitz R, Hallak M, Katz M, Mazor M (2006) Shoulder dystocia: a comparison of patients with and without diabetes mellitus. Arch Gynecol Obstet 273(4):203–206
ACOG Committee on Practice Bulletins–Obstetrics (2002) ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol 99(1):159–167
American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics (2001) ACOG practice bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 30, September 2001 (replaces Technical Bulletin Number 200, December 1994). Gestational diabetes. Obstet Gynecol 98(3):525–538
ACOG Committee on Practice Bulletins (2005) ACOG practice bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 60, March 2005. Pregestational diabetes mellitus. Obstet Gynecol 105(3):675–685
Menacker F, Hamilton BE (2010) Recent trends in cesarean delivery in the United States. CHS data brief, no 35. Centers for disease control and prevention national center for health statistics, Hyattsville
Spellacy WN, Miller S, Winegar A, Peterson PQ (1985) Macrosomia: maternal characteristics and infant complications. Obstet Gynecol 66:158–161
Robinson H, Tkatch S, Mayes DC, Bott N, Okun N (2003) Is maternal obesity a predictor of shoulder dystocia? Obstet Gynecol 101(1):24
Acknowledgments
Performed in part of Avishai Tsur MD requirements.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsur, A., Sergienko, R., Wiznitzer, A. et al. Critical analysis of risk factors for shoulder dystocia. Arch Gynecol Obstet 285, 1225–1229 (2012). https://doi.org/10.1007/s00404-011-2139-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-2139-8