Abstract
Purpose
To evaluate the relationship between the uterine size measured by pelvic magnetic resonance and reproductive outcome in women with a unicornuate uterus.
Methods
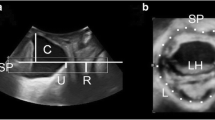
This was a retrospective study including 140 patients affiliated with unicornuate uterus diagnosed by the pelvic MR prior to their first pregnancy in the Obstetrics and Gynecology Hospital of Fudan University from April 2010 to December 2017. All the length of the unicornuate uterus were re-measured and recorded by skilled radiologists during the study period. We divided all the 140 participants with complete pelvic MR imaging into four groups by the best reproductive outcomes, which refers to Group 1 (primary infertility, n = 21), Group 2 ( < 24 weeks’ gestation, n = 34), Group 3 (preterm delivery, 24–35 weeks’ gestation, n = 13), Group 4 ( ≥ 35 weeks’ gestation, n = 72), followed them up and then analyzed the data.
Results
Measurements of 140 patients with hemi-uteri were retrieved for analysis. The mean length of the uterine was 4.90 ± 0.56 cm. There were no significant differences in the uterine cavity length, cervical length, endometrial thickness and uterine wall thickness between the four groups while the uterine length (P = 0.001) was statistically significant. Women with uterine lengths ≥ 4.5 cm were more likely to experience full-term delivery compared with the other group (P = 0.001). Ordinal multiple logistic regression analysis showed that the uterine length [OR = 9.03 (95% CI: 2.90–28.13)] and uterine cavity length [OR = 0.32 (95% CI: 0.06–2.04)] were independent protective factors for better obstetric outcomes
Conclusion
The uterine length is a reliable prognostic factor for the gestational week of delivery and an appropriate antenatal surveillance factor of women with unicornuate uterus.


Similar content being viewed by others
References
White-Walker S (2000) Before we are born: essentials of embroyology and birth defects. J Midwifery Women's Health 45(2):192. https://doi.org/10.1016/S1526-9523(99)00025-2
Sawada M, Kakigano A, Matsuzaki S, Takiuchi T, Mimura K, Kumasawa K, Endo M, Ueda Y, Yoshino K, Kimura T (2018) Obstetric outcome in patients with a unicornuate uterus after laparoscopic resection of a rudimentary horn. J Obstet Gynaecol Res. https://doi.org/10.1111/jog.13622
Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A (2011) The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update 17(6):761–771. https://doi.org/10.1093/humupd/dmr028
The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, mullerian anomalies and intrauterine adhesions (1988). Fertil Steril 49 (6):944-955. doi:10.1016/s0015-0282(16)59942-7
Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Brolmann H, Gianaroli L, Campo R (2013) The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 28(8):2032–2044. https://doi.org/10.1093/humrep/det098
Zyla MM, Wilczynski J, Nowakowska-Glab A, Maniecka-Bryla I, Nowakowska D (2015) Pregnancy and delivery in women with uterine malformations. Adv Clin Exp Med 24(5):873–879. https://doi.org/10.17219/acem/23171
Venetis CA, Papadopoulos SP, Campo R, Gordts S, Tarlatzis BC, Grimbizis GF (2014) Clinical implications of congenital uterine anomalies: a meta-analysis of comparative studies. Reprod Biomed Online 29(6):665–683. https://doi.org/10.1016/j.rbmo.2014.09.006
Reichman D, Laufer MR, Robinson BK (2009) Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril 91(5):1886–1894. https://doi.org/10.1016/j.fertnstert.2008.02.163
Reichman DE, Laufer MR (2010) Congenital uterine anomalies affecting reproduction. Best Pract Res Clin Obstet Gynaecol 24(2):193–208. https://doi.org/10.1016/j.bpobgyn.2009.09.006
Francisco Raga CB, Remohi Jose, Bonilla-Musoles F, Simo ́n C, Pellicer A (1997) Reproductive impact of congenital Mu ̈llerian anomalies. Hum Reprod 12(10):2277–2281
Egbase PE, Al-Sharhan M, Grudzinskas JG (2000) Influence of position and length of uterus on implantation and clinical pregnancy rates in IVF and embryo transfer treatment cycles. Hum Reprod 15(9):1943–1946
Hawkins LK, Correia KF, Srouji SS, Hornstein MD, Missmer SA (2013) Uterine length and fertility outcomes: a cohort study in the IVF population. Hum Reprod 28(11):3000–3006. https://doi.org/10.1093/humrep/det344
Cenksoy PO, Ficicioglu C, Yesiladali M, Akcin OA, Kaspar C (2014) The importance of the length of uterine cavity, the position of the tip of the inner catheter and the distance between the fundal endometrial surface and the air bubbles as determinants of the pregnancy rate in IVF cycles. Eur J Obstet Gynecol Reprod Biol 172:46–50. https://doi.org/10.1016/j.ejogrb.2013.09.023
Chun SS, Chung MJ, Chong GO, Park KS, Lee TH (2010) Relationship between the length of the uterine cavity and clinical pregnancy rates after in vitro fertilization or intracytoplasmic sperm injection. Fertil Steril 93(2):663–665. https://doi.org/10.1016/j.fertnstert.2009.08.067
Grimbizis GF, Di Spiezio SA, Saravelos SH, Gordts S, Exacoustos C, Van Schoubroeck D, Bermejo C, Amso NN, Nargund G, Timmerman D, Athanasiadis A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Tarlatzis B, Farquharson R, Gianaroli L, Campo R (2016) The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. Hum Reprod 31(1):2–7. https://doi.org/10.1093/humrep/dev264
Sheth SS, Hajari AR, Lulla CP, Kshirsagar D (2017) Sonographic evaluation of uterine volume and its clinical importance. J Obstet Gynaecol Res 43(1):185–189. https://doi.org/10.1111/jog.13189
Mastrolia SA, Baumfeld Y, Hershkovitz R, Yohay D, Trojano G, Weintraub AY (2018) Independent association between uterine malformations and cervical insufficiency: a retrospective population-based cohort study. Arch Gynecol Obstet 297(4):919–926. https://doi.org/10.1007/s00404-018-4663-2
Kaveh M, Mehdizadeh Kashi A, Sadegi K, Forghani F (2018) Pregnancy in non-communicating rudimentary horn of a unicornuate uterus. Int J Fertil Steril 11(4):318–320. https://doi.org/10.22074/ijfs.2018.5022
Kanno Y, Suzuki T, Nakamura E, Goya K, Nishijima Y, Shinoda M, Hayashi M, Izumi S (2014) Successful term delivery after laparoscopic resection of a non-communicating rudimentary horn in a patient with a unicornuate uterus: a case report. Tokai J Exp Clin Med 39(2):59–63
Lin PC, Bhatnagar KP, Nettleton GS, Nakajima ST (2002) Female genital anomalies affecting reproduction. Fertil Steril 78(5):899–915
Jayasinghe Y, Rane A, Stalewski H, Grover S (2005) The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 105(6):1456–1467. https://doi.org/10.1097/01.AOG.0000161321.94364.56
Pados G, Tsolakidis D, Athanatos D, Almaloglou K, Nikolaidis N, Tarlatzis B (2014) Reproductive and obstetric outcome after laparoscopic excision of functional, non-communicating broadly attached rudimentary horn: a case series. Eur J Obstet Gynecol Reprod Biol 182:33–37. https://doi.org/10.1016/j.ejogrb.2014.08.023
Fox NS, Roman AS, Stern EM, Gerber RS, Saltzman DH, Rebarber A (2014) Type of congenital uterine anomaly and adverse pregnancy outcomes. J Matern Fetal Neonatal Med 27(9):949–953. https://doi.org/10.3109/14767058.2013.847082
Liu J, Wu Y, Xu S, Su D, Han Y, Wu X (2017) Retrospective evaluation of pregnancy outcomes and clinical implications of 34 Han Chinese women with unicornuate uterus who received IVF-ET or ICSI-ET treatment. J Obstet Gynaecol 37(8):1020–1024. https://doi.org/10.1080/01443615.2017.1318266
Li X, Ouyang Y, Yi Y, Lin G, Lu G, Gong F (2017) Pregnancy outcomes of women with a congenital unicornuate uterus after IVF-embryo transfer. Reprod Biomed Online 35(5):583–591. https://doi.org/10.1016/j.rbmo.2017.07.015
Akar ME, Bayar D, Yildiz S, Ozel M, Yilmaz Z (2005) Reproductive outcome of women with unicornuate uterus. Aust N Z J Obstet Gynaecol 45(2):148–150. https://doi.org/10.1111/j.1479-828X.2005.00346.x
Hawkins LK, Missmer SA, Correia KF, Hornstein MD (2014) Assessment of pregnancy-associated, within-woman change in uterine length. J Matern-Fetal Neo M 27(10):989–993. https://doi.org/10.3109/14767058.2013.853732
Donderwinkel PF, Dorr JP, Willemsen WN (1992) The unicornuate uterus: clinical implications. Eur J Obstet Gynecol Reprod Biol 47(2):135–139. https://doi.org/10.1016/0028-2243(92)90043-X
Acknowledgements
The authors thank the Obstetrics and Gynecology Hospital of Fudan University for supporting in statistical analyses. The authors are grateful to Yuan He for her advice on the data analysis. The authors thank DXJ and KHQ for carefully reviewing the article.
Funding
This study was supported by the Chinese National Nature Sciences Foundation [grant number 81471416 and 81771524].
Author information
Authors and Affiliations
Contributions
XQL: project development, data management, data analysis, and manuscript writing. HJQ: project development and data management. XYZ: data collection. SFZ: project development. YH: data analysis. KQH: data management. JXD: manuscript revise and project development. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All the authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of the Department of Gynecology, the Obstetrics and Gynecology Hospital of Fudan University [2018–18] and informed consent was obtained from each individual.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Xq., Qian, Hj., Zhang, Xy. et al. Analysis of the reproductive outcomes and the size of the unicornuate uterus measured by magnetic resonance imaging and their relationship. Arch Gynecol Obstet 299, 1321–1330 (2019). https://doi.org/10.1007/s00404-019-05106-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05106-y