Abstract
Background
Prolonged surgical operative time is associated with postoperative adverse outcomes following total knee arthroplasty (TKA). Increasing operating room efficiency necessitates the accurate prediction of surgical operative time for each patient. One potential way to increase the accuracy of predictions is to use advanced predictive analytics, such as machine learning. The aim of this study is to use machine learning to develop an accurate predictive model for surgical operative time for patients undergoing primary total knee arthroplasty.
Methods
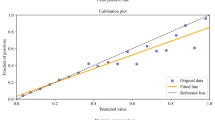
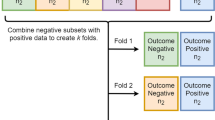
A retrospective chart review of electronic medical records was conducted to identify patients who underwent primary total knee arthroplasty at a tertiary referral center. Three machine learning algorithms were developed to predict surgical operative time and were assessed by discrimination, calibration and decision curve analysis. Specifically, we used: (1) Artificial Neural Networks (ANNs), (2) Random Forest (RF), and (3) K-Nearest Neighbor (KNN).
Results
We analyzed the surgical operative time for 10,021 consecutive patients who underwent primary total knee arthroplasty. The neural network model achieved the best performance across discrimination (AUC = 0.82), calibration and decision curve analysis for predicting surgical operative time. Based on this algorithm, younger age (< 45 years), tranexamic acid non-usage, and a high BMI (> 40 kg/m2) were the strongest predictors associated with surgical operative time.
Conclusions
This study shows excellent performance of machine learning models for predicting surgical operative time in primary total knee arthroplasty. The accurate estimation of surgical duration is important in enhancing OR efficiency and identifying patients at risk for prolonged surgical operative time.
Level of evidence
Level III, case control retrospective analysis.



Similar content being viewed by others
References
Halawi MJ, Molloy R, Barsoum WK (2016) Maximizing efficiency in the operating room for total joint artroplasty. Am J Orthop (Belle Mead NJ) 45:E233–E235
Attarian DE, Wahl JE, Wellman SS, Bolognesi MP (2013) Developing a high-efficiency operating room for total joint arthroplasty in an academic setting. Clin Orthop Relat Res 471:1832–1836. https://doi.org/10.1007/s11999-012-2718-4
Oganesyan R, Klemt C, Esposito J et al (2021) Knee arthroscopy prior to revision TKA Is associated with increased re-revision for stiffness. J Knee Surg. https://doi.org/10.1055/s-0040-1722662
Dexter F, Epstein RH (2005) Operating room efficiency and scheduling. Curr Opin Anesthesiol 18:195
Master N, Zhou Z, Miller D et al (2017) Improving predictions of pediatric surgical durations with supervised learning. Int J Data Sci Anal 4:35–52. https://doi.org/10.1007/s41060-017-0055-0
Larsson A (2013) The accuracy of surgery time estimations. Prod Plan Control 24:891–902. https://doi.org/10.1080/09537287.2012.666897
Tuwatananurak JP, Zadeh S, Xu X et al (2019) Machine learning can improve estimation of surgical case duration: a pilot study. J Med Syst. https://doi.org/10.1007/s10916-019-1160-5
Khanuja HS, Solano MA, Sterling RS et al (2019) Surgeon mean operative times in total knee arthroplasty in a variety of settings in a health system. J Arthroplasty 34:2569–2572. https://doi.org/10.1016/j.arth.2019.06.029
Wang Q, Goswami K, Shohat N et al (2019) Longer operative time results in a higher rate of subsequent periprosthetic joint infection in patients undergoing primary joint arthroplasty. J Arthroplasty 34:947–953. https://doi.org/10.1016/j.arth.2019.01.027
Bredow J, Boese CK, Flörkemeier T et al (2018) Factors affecting operative time in primary total hip arthroplasty: a retrospective single hospital cohort study of 7674 cases. Technol Health Care 26:857–866. https://doi.org/10.3233/THC-171015
Borjali A, Chen AF, Muratoglu OK et al (2020) Detecting total hip replacement prosthesis design on plain radiographs using deep convolutional neural network. J Orthop Res Off Publ Orthop Res Soc 38:1465–1471. https://doi.org/10.1002/jor.24617
Kunze KN, Karhade AV, Sadauskas AJ et al (2020) Development of machine learning algorithms to predict clinically meaningful improvement for the patient-reported health state after total hip arthroplasty. J Arthroplasty 35:2119–2123. https://doi.org/10.1016/j.arth.2020.03.019
Klemt C, Harvey MJ, Robinson MG et al (2022) Machine learning algorithms predict extended postoperative opioid use in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06812-4
Karhade AV, Schwab JH, Bedair HS (2019) Development of machine learning algorithms for prediction of sustained postoperative opioid prescriptions after total hip arthroplasty. J Arthroplasty 34:2272-2277.e1. https://doi.org/10.1016/j.arth.2019.06.013
Yeo I, Klemt C, Robinson MG et al (2022) The use of artificial neural networks for the prediction of surgical site infection following TKA. J Knee Surg. https://doi.org/10.1055/s-0041-1741396
Darst BF, Malecki KC, Engelman CD (2018) Using recursive feature elimination in random forest to account for correlated variables in high dimensional data. BMC Genet 19:1–6. https://doi.org/10.1186/s12863-018-0633-8
Karhade AV, Ogink PT, Thio QCBS et al (2019) Machine learning for prediction of sustained opioid prescription after anterior cervical discectomy and fusion. Spine J 19:976–983. https://doi.org/10.1016/j.spinee.2019.01.009
Mallow GM, Siyaji ZK, Galbusera F et al (2021) Intelligence-based spine care model: a new era of research and clinical decision-making. Glob Spine J 11:135–145. https://doi.org/10.1177/2192568220973984
Ben-Ari A, Chansky H, Rozet I (2017) Preoperative opioid use is associated with early revision after total knee arthroplasty: a study of male patients treated in the veterans affairs system. J Bone Joint Surg Am 99:1–9. https://doi.org/10.2106/JBJS.16.00167
Klemt C, Tirumala V, Barghi A et al (2022) Artificial intelligence algorithms accurately predict prolonged length of stay following revision total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06894-8
Cohen-Levy WB, Klemt C, Tirumala V et al (2022) Artificial neural networks for the prediction of transfusion rates in primary total hip arthroplasty. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04391-8
Klemt C, Tirumala V, Smith EJ et al (2020) Development of a preoperative risk calculator for re-infection following revision surgery for periprosthetic joint infection. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.08.004
Ferro CAT (2007) Comparing probabilistic forecasting systems with the Brier score. Weather Forecast 22:1076–1088. https://doi.org/10.1175/WAF1034.1
Mendez JH, Mehrani A, Randolph P, Stagg S (2019) Throughput and resolution with a next-generation direct electron detector. IUCrJ 6:1007–1013. https://doi.org/10.1107/S2052252519012661
Klemt C, Drago J, Tirumala V, Kwon Y-M (2021) Asymmetrical tibial polyethylene geometry-cruciate retaining total knee arthroplasty does not fully restore in-vivo articular contact kinematics during strenuous activities. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06384-9
Gabriel RA, Wu A, Huang CC et al (2016) National incidences and predictors of inefficiencies in perioperative care. J Clin Anesth 31:238–246. https://doi.org/10.1016/j.jclinane.2016.01.007
Timoney N, Procter L, Liau J et al (2016) The effects of surgeons and anesthesiologists on operating room efficiency. Interdiscip Neurosurg 5:38–42. https://doi.org/10.1016/j.inat.2016.06.001
Laskin DM, Abubaker AO, Strauss RA (2013) Accuracy of predicting the duration of a surgical operation. J Oral Maxillofac Surg 71:446–447. https://doi.org/10.1016/j.joms.2012.10.009
Wu A, Huang C-C, Weaver MJ, Urman RD (2016) Use of historical surgical times to predict duration of primary total knee arthroplasty. J Arthroplasty 31:2768–2772. https://doi.org/10.1016/j.arth.2016.05.038
Eijkemans MJC, van Houdenhoven M, Nguyen T et al (2010) Predicting the unpredictable: a new prediction model for operating room times using individual characteristics and the surgeon’s estimate. Anesthesiology 112:41–49. https://doi.org/10.1097/ALN.0b013e3181c294c2
Stepaniak PS, Heij C, Mannaerts GHH et al (2009) Modeling procedure and surgical times for current procedural terminology-anesthesia-surgeon combinations and evaluation in terms of case-duration prediction and operating room efficiency: a multicenter study. Anesth Analg 109:1232–1245. https://doi.org/10.1213/ANE.0b013e3181b5de07
Freeman NLB, McGinigle KL, Leese PJ (2019) Using electronic medical records to identify enhanced recovery after surgery cases. EGEMS (Washington, DC) 7:34
Duchman KR, Pugely AJ, Martin CT et al (2017) Operative time affects short-term complications in total joint arthroplasty. J Arthroplasty 32:1285–1291. https://doi.org/10.1016/j.arth.2016.12.003
Bartek MA, Saxena RC, Solomon S et al (2019) Improving operating room efficiency: machine learning approach to predict case-time duration. J Am Coll Surg 229:346-354.e3. https://doi.org/10.1016/j.jamcollsurg.2019.05.029
Wu A, Weaver MJ, Heng MM, Urman RD (2017) Predictive model of surgical time for revision total hip arthroplasty. J Arthroplasty 32:2214–2218. https://doi.org/10.1016/j.arth.2017.01.056
Sutradhar R, Barbera L (2020) Comparing an artificial neural network to logistic regression for predicting ED visit risk among patients with cancer: a population-based cohort Study. J Pain Symptom Manage 60:1–9. https://doi.org/10.1016/j.jpainsymman.2020.02.010
Myers TG, Ramkumar PN, Ricciardi BF et al (2020) Artificial intelligence and orthopaedics. J Bone Jt Surg. https://doi.org/10.2106/jbjs.19.01128
Ramkumar PN, Karnuta JM, Navarro SM et al (2019) Deep learning preoperatively predicts value metrics for primary total knee arthroplasty: development and validation of an artificial neural network model. J Arthroplasty 34:2220-2227.e1. https://doi.org/10.1016/j.arth.2019.05.034
Silber JH, Rosenbaum PR, Zhang X, Even-Shoshan O (2007) Influence of patient and hospital characteristics on anesthesia time in medicare patients undergoing general and orthopedic surgery. Anesthesiology 106:356–364. https://doi.org/10.1097/00000542-200702000-00025
Sodhi N, Anis HK, Gold PA et al (2019) Operative times can predict and are correlated with lengths-of-stay in primary total knee arthroplasty: a nationwide database study. J Arthroplasty 34:1328–1332. https://doi.org/10.1016/j.arth.2019.03.024
Liabaud B, Patrick DAJ, Geller JA (2013) Higher body mass index leads to longer operative time in total knee arthroplasty. J Arthroplasty 28:563–565. https://doi.org/10.1016/j.arth.2012.07.037
Girardi FM, Liu J, Guo Z et al (2019) The impact of obesity on resource utilization among patients undergoing total joint arthroplasty. Int Orthop 43:269–274. https://doi.org/10.1007/s00264-018-4059-8
Mufarrih SH, Malik AT, Qureshi NQ et al (2018) The effect of tranexamic acid in unilateral and bilateral total knee arthroplasty in the South Asian population: A retrospective cohort study. Int J Surg 52:25–29. https://doi.org/10.1016/j.ijsu.2018.02.005
Stoicea N, Moran K, Mahmoud A-R et al (2018) Tranexamic acid use during total hip arthroplasty: A single center retrospective analysis. Medicine (Baltimore) 97:e10720. https://doi.org/10.1097/MD.0000000000010720
Guerreiro JPF, Badaro BS, Balbino JRM et al (2017) Application of tranexamic acid in total knee arthroplasty - prospective randomized trial. Open Orthop J 11:1049–1057. https://doi.org/10.2174/1874325001711011049
Helm JM, Swiergosz AM, Haeberle HS et al (2020) Machine learning and artificial intelligence: definitions, applications, and future directions. Curr Rev Musculoskelet Med 13:69–76. https://doi.org/10.1007/s12178-020-09600-8
Surace P, Sultan AA, George J et al (2019) The association between operative time and short-term complications in total hip arthroplasty: an analysis of 89,802 surgeries. J Arthroplasty 34:426–432. https://doi.org/10.1016/j.arth.2018.11.015
Ravi B, Jenkinson R, O’Heireamhoin S et al (2019) Surgical duration is associated with an increased risk of periprosthetic infection following total knee arthroplasty: a population-based retrospective cohort study. EClinicalMedicine 16:74–80. https://doi.org/10.1016/j.eclinm.2019.09.015
Bonner BE, Castillo TN, Fitz DW et al (2019) Preoperative opioid use negatively affects patient-reported outcomes after primary total hip arthroplasty. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-18-00658
Funding
This study did not receive any funding. All authors report no conflict of interest or financial disclosures. There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article. The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent.
Informed consent was obtained for the retrospective patient chart review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yeo, I., Klemt, C., Melnic, C.M. et al. Predicting surgical operative time in primary total knee arthroplasty utilizing machine learning models. Arch Orthop Trauma Surg 143, 3299–3307 (2023). https://doi.org/10.1007/s00402-022-04588-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04588-x