Abstract
Introduction
New technologies exist which may assist surgeons to better predict final intra-operative joint balance. Our objectives were to compare the impact of (1) a predictive digital joint tensioning tool on intra-operative joint balance; and (2) joint balance and flexion joint laxity on patient-reported outcomes.
Materials and methods
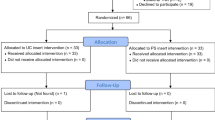
Two-hundred Eighty patients received posterior cruciate ligament sacrificing TKA with ultra-congruent tibial inserts using a robotic-assisted navigation platform. Patients were divided into those in which a Predictive Plan with a digital joint-tensioning device was used (PP) and those in which it was not (NPP), in all cases final post-operative joint gaps were collected immediately before final implantation. Demographics and KOOS were collected pre-operatively. KOOS, complications and satisfaction were collected at 3, 6 and 12 months post-operatively. Optimal balance difference between PP and NPP was defined and compared using area-under-the-curve analysis (AUC). Outcomes were then compared according to the results from the AUC.
Results
AUC analysis yielded a balance threshold of 1.5 mm, in which the PP group achieved a higher rate of balance throughout flexion compared to the NPP group: extension: 83 vs 52%; Midflexion: 82 vs 55%; Flexion 89 vs 68%; Flexion to Extension 80 vs 49%; p ≤ 0.003. Higher KOOS scores were observed in knees balanced within 1.5 mm across all sub-scores at various time points, however, differences did not exceed the minimum clinically important difference (MCID). Patients with > 1.5 mm flexion laxity medially or laterally had an increased likelihood of 2.2 (1.1–4.4) and 2.5 (1.3–4.8), respectively, for failing to achieve the Patient Acceptable Symptom State for KOOS Pain at 12 months. Patient satisfaction was high in both the PP and NPP groups (97.4 and 94.7%, respectively).
Conclusions
Use of a predictive joint tensioning tool improved the final balance in TKA. Improved outcomes were found in balanced knees; however, this improvement did not achieve the MCID, suggesting further studies may be required to define optimal balance targets. Limiting medial and lateral flexion laxity resulted in an increased likelihood of achieving the Patient Acceptable Symptom State for KOOS Pain.





Similar content being viewed by others
References
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD, Suarez JC, Higuera-Rueda CA, Barsoum WK (2019) Are patients more satisfied with a balanced TKA? J Arthroplasty 34(7):S195–S200
Hirschmann MT, Becker R, Tandogan R, Vendittoli P-A, Howell S (2019) Alignment in TKA: what has been clear is not anymore! Knee Surg Sports Traumatol Arthrosc 27:2037–2039
Kappel A, Laursen M, Nielsen PT, Odgaard A (2019) Relationship between outcome scores and knee laxity following total knee arthroplasty: a systematic review. Acta Orthop 90(1):46–52
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty 29(5):955–960
Scuderi GR, Komistek RD, Dennis DA, Insall JN (2003) The impact of femoral component rotational alignment on condylar lift-off. Clin Orthop Relat R 410:148–154
Clarke HD, Scuderi GR (2003) Flexion instability in primary total knee replacement. J Knee Surg 16(2):123–128
Howell SM, Shelton TJ, Hull ML (2018) Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty 33:3678–3684
McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 101(3):331–339
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H, Matsuda S (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24(6):1478–1484
Shelton TJ, Howell SM, Hull ML (2019) Is there a force target that predicts early patient-reported outcomes after kinematically aligned TKA? Clin Orthop Relat R 477(5):1200–1207
Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y, Furu M, Ito H, Matsuda S (2018) Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138(8):1143–1150
Nakahara H, Okazaki K, Hamai S, Okamoto S, Kuwashima U, Higaki H, Iwamoto Y (2015) Does knee stability in the coronal plane in extension affect function and outcome after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23(6):1693–1698
MacDessi SJ, Wood JA, Diwan AD, Harris IA (2020) Surgeon-defined assessment is a poor predictor of knee balance in total knee arthroplasty: a prospective, multicenter study. Knee Surg Sports Traumatol Arthrosc 29:498–506
Elmallah RK, Mistry JB, Cherian JJ, Chughtai M, Bhave A, Roche MW, Mont MA (2016) Can we really “feel” a balanced total knee arthroplasty? J Arthroplasty 31(9):102–105
Nagle M, Glynn A (2019) Midflexion instability in primary total knee arthroplasty: a review article. J Knee Surg 33(05):459–465
Siddiqi A, Smith T, McPhilemy JJ, Ranawat AS, Sculco PK, Chen AF (2020) Soft-tissue balancing technology for total knee arthroplasty. J Bone Joint Surg Am 8(1):1–15
Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C (2019) Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplasty Today 5(3):334–340
Connelly JW, Galea VP, Rojanasopondist P, Matuszak SJ, Ingelsrud LH, Nielsen CS, Bragdon CR, Huddleston JI III, Malchau H, Troelsen A (2019) Patient acceptable symptom state at 1 and 3 years after total knee arthroplasty: thresholds for the Knee Injury and Osteoarthritis Outcome Score (KOOS). J Bone Joint Surg Am 101(11):995–1003
Jawhar A, Hutter K, Scharf H-P (2016) Outcome in total knee arthroplasty with a medial-lateral balanced versus unbalanced gap. J Orthopaed Res 24(3):298–301
Mehliß V, Leira MS, Olaizola AS, Scior W, Graichen H (2019) Proven accuracy for a new dynamic gap measurement in navigated TKA. Knee Surg Sports Traumatol Arthrosc 27(4):1189–1195
Chia Z-Y, Pang H-N, Tan M-H, Yeo S-J (2018) Gap difference in navigated TKA: a measure of the imbalanced flexion-extension gap. SICOT-J 4:30
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF (2008) Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biometrical J 50(3):419–430
Roos E (2019) KOOS FAQs. http://www.koos.nu/index.html. Accessed Dec 13 2019
Joseph J, Simpson P, Whitehouse SL, English HW, Donnelly WJ (2013) The use of navigation to achieve soft tissue balance in total knee arthroplasty—a randomised clinical study. Knee 20(6):401–406
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW (2017) Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty 32(12):3854–3860. https://doi.org/10.1016/j.arth.2017.07.021
Wakelin EA, Shalhoub S, Lawrence JM, Keggi JM, DeClaire JH, Randall AL, Ponder CE, Koenig JA, Lyman S, Plaskos C (2021) Improved total knee arthroplasty pain outcome when joint gap targets are achieved throughout flexion. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06482-2
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR), AOA, Adelaide (2020), p 221. https://aoanjrr.sahmri.com/annual-reports-2020. Accessed 16 Nov 2020
Ishii Y, Noguchi H, Sato J, Ishii H, Toyabe S-i (2019) Mediolateral coronal laxity does not correlate with knee range of motion after total knee arthroplasty. Arch Orthop Trauma Surg 139(6):851–858. https://doi.org/10.1007/s00402-019-03161-3
Kornuijt A, Das D, Sijbesma T, de Vries L, van der Weegen W (2018) Manipulation under anesthesia following total knee arthroplasty: a comprehensive review of literature. Musculoskelet Surg 102(3):223–230
Knapp P, Weishuhn L, Pizzimenti N, Markel DC (2020) Risk factors for manipulation under anaesthesia after total knee arthroplasty. Bone Joint J 102(6 Suppl A):66–72
Crawford DA, Adams JB, Berend KR, Lombardi AV (2020) Low complication rates in outpatient total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28(5):1458–1464
Jeon S-W, Kim K-I, Song SJ (2019) Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty 34(8):1656–1661
Vermue H, Lambrechts J, Tampere T, Arnout N, Auvinet E, Victor J (2020) How should we evaluate robotics in the operating theatre? a systematic review of the learning curve of robot-assisted knee arthroplasty. Bone Joint J 102(4):407–413
Deering EM, Hu SY, Abdulkarim A (2019) Does tourniquet use in TKA increase postoperative pain? A systematic review and meta-analysis. Clin Orthop Relat R 477(3):547
Jones CW, Jacobs H, Shumborski S, Talbot S, Redgment A, Brighton R, Walter WL (2020) Sagittal stability and implant design affect patient reported outcomes after Total knee Arthroplasty. J Arthroplasty 35(3):747–751
Abdel MP, Ollivier M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW (2018) Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. JBJS 100(6):472–478
Nodzo SR, Franceschini V, Della Valle AG (2017) Intraoperative load-sensing variability during cemented, posterior-stabilized total knee arthroplasty. J Arthroplasty 32(1):66–70
van der Linde JA, Leong AK (2019) Does bone cement influence soft tissue balancing in total knee arthroplasty? Knee 26(2):405–409
Funding
Funding for this study was provided by Corin Group Plc.
Author information
Authors and Affiliations
Contributions
EW, SS: paid employees of Corin. CP: paid employee, stock options in Corin. JL: paid consultant and speaker to Corin and Stryker. JK: paid consultant, speaker and research support from Corin. JD: paid consultant, speaker and research support Corin, Smith and Nephew and Zimmer Biomet. Royalties from Zimmer Biomet. AR: paid consultant, speaker and research support to Corin. CEP: paid consultant, speaker, research support and Royalties from Corin. Paid consultant to Styker and Med 7. Share holder of Joint Development LLC. JAK: paid consultant, research support, paid speaker and royalties from Corin. SL: paid consultant from Corin and Cell Source (Tokyo).
Corresponding author
Ethics declarations
Ethical approval
IRB approval for this study was obtained from New England Institutional Review Board, No: 120170260.
Informed consent
Informed consent was obtained from all participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keggi, J.M., Wakelin, E.A., Koenig, J.A. et al. Impact of intra-operative predictive ligament balance on post-operative balance and patient outcome in TKA: a prospective multicenter study. Arch Orthop Trauma Surg 141, 2165–2174 (2021). https://doi.org/10.1007/s00402-021-04043-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04043-3