Abstract
Introduction
Severe acetabular bone loss, both with or without pelvic discontinuity, remains a challenge in revision total hip arthroplasty (RTHA). The goal of our study was to evaluate the mid-term results for consecutive patients with Paprosky III acetabular bone loss with or without pelvic discontinuity who needed RTHA with custom-made acetabular implants and to compare the results to those of other studies.
Materials and methods
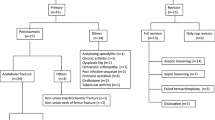
Sixty-eight (68) patients with severe acetabular bone loss (Paprosky Type IIIa and IIIb), who required RTHA, were included in our study. All prostheses were constructed on the basis of thin-layer computed tomography (CT) scans of the pelvis. The visual analogue scale (VAS), Harrison hip score (HHS), and clinical and radiographic follow-up assessments were used to evaluate the outcome.
Results
The average follow-up time was 43 months (range 1–120 months). Implant survival at last follow-up was 75% (51 of 68). Kaplan–Meier survival analysis, with explantation as the endpoint, revealed survival rates of 82.7% (3 years) and 77% (5 years). Patients with revision of the acetabular component only had a significant higher survival rate (p 0.012). Overall revision rate was 36.7%. Reinfection rate was 34.4%. Complications included 15 (22%) periprosthetic joint infections (PJI), 7 dislocations (10.2%), and 2 aseptic loosenings (2.9%). Mean VAS at last follow-up was 1.45 compared to 3.2 preoperatively, while mean HHS improved from 21.1 points preoperatively to 61 at last follow-up. The change in both scores was thus significant (p < 0.001).
Conclusion
Defect reconstruction with custom-made modular acetabular implants can be a good, nevertheless expensive, treatment option with clinically and radiologically satisfying results in comparison to recent studies in the literature. Nevertheless, high postoperative complication rates, especially in terms of PJI, remain a challenge.





Similar content being viewed by others
References
Khanduja V (2017) Total hip arthroplasty in 2017—current concepts and recent advances. Indian J Orthop 51:357–358. https://doi.org/10.4103/ortho.IJOrtho_367_17
Schmolders J, Friedrich MJ, Michel RD, Randau TM, Wimmer MD, Strauss AC, Kohlhof H, Wirtz DC, Gravius S (2015) Acetabular defect reconstruction in revision hip arthroplasty with a modular revision system and biological defect augmentation. Int Orthop 39:623–630. https://doi.org/10.1007/s00264-014-2533-5
Zuiderbaan HA, Visser D, Sierevelt IN, Penders J, Verhart J, Vergroesen DA (2018) Long-term clinical results of the Metasul metal-on-metal total hip arthroplasty: 12.6 years follow-up of 128 primary total hip replacements. HIP Int 28:330–335. https://doi.org/10.5301/hipint.5000574
Labek G, Thaler M, Janda W, Agreiter M, Stöckl B (2011) Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br 93-B:293–297. https://doi.org/10.1302/0301-620X.93B3.25467
Friedrich MJ, Schmolders J, Michel RD, Randau TM, Wimmer MD, Kohlhof H, Wirtz DC, Gravius S (2014) Management of severe periacetabular bone loss combined with pelvic discontinuity in revision hip arthroplasty. Int Orthop 38:2455–2461. https://doi.org/10.1007/s00264-014-2443-6
Gravius S, Pagenstert G, Weber O, Kraska N, Röhrig H, Wirtz DC (2009) Acetabular defect reconstruction in revision surgery of the hip. Autologous, homologous or metal? Orthop 38:729–740. https://doi.org/10.1007/s00132-009-1428-4
D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH (1989) Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop 243:126–137
Christie MJ, Barrington SA, Brinson MF, Ruhling ME, DeBoer DK (2001) Bridging massive acetabular defects with the triflange cup: 2- to 9-year results. Clin Orthop 393:216–227
Berasi CC, Berend KR, Adams JB, Ruh EL, Lombardi AV (2015) Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res 473:528–535. https://doi.org/10.1007/s11999-014-3969-z
Wimmer MD, Randau TM, Petersdorf S, Pagenstert GI, Weißkopf M, Wirtz DC, Gravius S (2013) Evaluation of an interdisciplinary therapy algorithm in patients with prosthetic joint infections. Int Orthop 37:2271–2278. https://doi.org/10.1007/s00264-013-1995-1
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Healy WL, Iorio R, Clair AJ, Pellegrini VD, Della Valle CJ, Berend KR (2016) Complications of total hip arthroplasty: standardized list, definitions, and stratification developed by the hip society. Clin Orthop Relat Res 474:357–364. https://doi.org/10.1007/s11999-015-4341-7
Roessler PP, Jaenisch M, Kuhlmann M, Wacker M, Johannes Wagenhäuser P, Gravius S, Wirtz DC (2018) The augment-and-modular-cage revision system for reconstruction of severe acetabular defects—two-year clinical and radiographic results. Int Orthop. https://doi.org/10.1007/s00264-018-4271-6
Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ (2012) Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res 470:428–434. https://doi.org/10.1007/s11999-011-2126-1
Schwarzkopf R, Ihn HE, Ries MD (2015) Pelvic discontinuity: modern techniques and outcomes for treating pelvic disassociation. HIP Int 25:368–374. https://doi.org/10.5301/hipint.5000270
De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK (2019) Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplasty 34:2511–2518. https://doi.org/10.1016/j.arth.2019.05.032
Goodman GP, Engh CA Jr (2016) The custom triflange cup: build it and they will come. Bone Jt J 98-B:68–72. https://doi.org/10.1302/0301-620X.98B.36354
Wind MA, Swank ML, Sorger JI (2013) Short-term results of a custom Triflange acetabular component for massive acetabular bone loss in revision THA. Orthopedics 36:e260–e265. https://doi.org/10.3928/01477447-20130222-11
De Meo F, Cacciola G, Bellotti V, Bruschetta A, Cavaliere P (2018) Trabecular Titanium acetabular cups in hip revision surgery: mid-term clinical and radiological outcomes. HIP Int 28:61–65. https://doi.org/10.1177/1120700018812992
Steno B, Kokavec M, Necas L (2015) Acetabular revision arthroplasty using trabecular titanium implants. Int Orthop 39:389–395. https://doi.org/10.1007/s00264-014-2509-5
Gallart X, Fernández-Valencia JA, Riba J, Bori G, García S, Tornero E, Combalía A (2016) Trabecular titaniumTM cups and augments in revision total hip arthroplasty: clinical results, radiology and survival outcomes. HIP Int 26:486–491. https://doi.org/10.5301/hipint.5000378
Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI (2018) Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Jt J 100-B:1442–1448. https://doi.org/10.1302/0301-620X.100B11.BJJ-2018-0481.R1
Schmolders J, Koob S, Schepers P, Pennekamp PH, Gravius S, Wirtz DC, Placzek R, Strauss AC (2017) Lower limb reconstruction in tumor patients using modular silver-coated megaprostheses with regard to perimegaprosthetic joint infection: a case series, including 100 patients and review of the literature. Arch Orthop Trauma Surg 137:149–153. https://doi.org/10.1007/s00402-016-2584-8
Pilge H, Gradl G, von Eisenhart-Rothe R, Gollwitzer H (2012) Incidence and outcome after infection of megaprostheses. HIP Int 22:83–90. https://doi.org/10.5301/HIP.2012.9576
Artiaco S, Boggio F, Colzani G, Titolo P, Zoccola K, Bianchi P, Bellomo F (2015) Megaprostheses in the revision of infected total hip arthroplasty. Clinical series and literature review. Bull Hosp Jt Dis 2013 73:229–232
Keswani A, Chi D, Lovy AJ, London DA, Cagle PJ, Parsons BO, Bosco JA (2019) Risk factors for and timing of adverse events after revision total shoulder arthroplasty. Shoulder Elb 11:332–343. https://doi.org/10.1177/1758573218780517
DeBoer DK, Brinson MR, Morrison IC (2007) Revision total hip arthroplasty for pelvic discontinuity. Revis Total HIP Arthroplasty 89:835–840. https://doi.org/10.2106/JBJS.F.00313
Myncke I, van Schaik D, Scheerlinck T (2017) Custom-made triflanged acetabular components in the treatment of major acetabular defects. Short-term results and clinical experience. Acta Orthop Belg 83:341–350
Jones CW, Choi DS, Sun P, Chiu Y-F, Lipman JD, Lyman S, Bostrom MPG, Sculco PK (2019) Clinical and design factors influence the survivorship of custom flange acetabular components. Bone Jt J 101-B:68–76. https://doi.org/10.1302/0301-620X.101B6.BJJ-2018-1455.R1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have a conflict of interest. No benefits directly or indirectly related to the subject matter of this article have been or will be received from a commercial party.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Formal consent is not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fröschen, F.S., Randau, T.M., Hischebeth, G.T.R. et al. Mid-term results after revision total hip arthroplasty with custom-made acetabular implants in patients with Paprosky III acetabular bone loss. Arch Orthop Trauma Surg 140, 263–273 (2020). https://doi.org/10.1007/s00402-019-03318-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03318-0