Abstract
Purpose
The aim of this study was to evaluate early results of acetabular revisions of total hip replacement using fully cementless trabecular titanium (TT) acetabular modular implants (Delta Trabecular Titanium, Limacorporate, Udine, Italy).
Methods
Between March 2009 and May 2012 TT was used in 81 revisions. The mean age at the time of revision was 68 years (32–84 years). There were nine patients revised for type 1, 11 for type 2A, 27 for type 2B, six for type 2C, 15 for type 3A and 13 for type 3B acetabular defects according to the Paprosky classification. Frozen morselised bone allografts were used in 53 cases and bulk structural allografts in three cases. Clinical evaluations were made using a modified functional Merle d’Aubigné-Postel score. The mean follow-up period was 38.14 months (24–62 months).
Results
The mean pre-operative Merle d’Aubigné-Postel functional score was 4.7 and 9.8 at the time of last follow-up. There was one revision due to instability of the acetabular component. A cage system—Delta Revision TT—was successfully used in this case. Three cases with Paprosky type 3B defect showed cranial migration of the acetabular component by 6 mm, but stabilised after six months. No dislocations associated with acetabular surgery have occurred in the cohort. There have been no dissociations of the modular component. A fatigue fracture of the hemispherical module occurred in the revised case. No other hardware mechanical failures have been recorded.
Conclusions
TT cups, hemispherical modules and augments facilitate reliable and reproducible biological fixation in acetabular revision surgery with excellent results. Extended follow-up is necessary to evaluate the long-term performance of TT modular implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of total hip arthroplasties (THA) performed each year is increasing. A similar trend has also been observed for revision hip procedures [1]. Different materials, implant designs and sizes are available for THA acetabular revisions [2]. Special constructs are used for THA revision surgery with various success rates [3, 4].
Trabecular metal (TM) sets of implants for revision surgery and for complex primary cases were introduced at the end of the twentieth century. TM, porous structure tantalum cups and augments have been effectively used with good results [5–7].
The fully cementless acetabular implant made of pure trabecular titanium (TT) is a relatively new concept, designed to support bone during revision surgery or in complex primary THA. Delta Trabecular Titanium (Limacorporate spa, Udine, Italy) has been available in the form of the Delta TT cup since 2007. Delta One TT, a versatile cup, and Delta Revision TT, a versatile revision socket, were introduced in 2008. TT has exceptional biomechanical characteristics [8]. In vivo studies showed promising results and remarkably fast and complete osseointegration [9]. Similar clinical results are also anticipated from Delta TT implants. We are reporting on our early experience with TT cups in acetabular revision surgery.
Materials and methods
Since March 2009 patients have been prospectively enrolled for use of the Delta TT system for acetabular revisions. Until May 2012, 80 patients had received a total of 81 Delta TT implants. The mean follow-up period was 38.14 months (24–62). There were 30 men and 50 women in the group, with a mean age of 68.3 (32–84) years. The left side was operated on in 42 patients and the right side in 39. All of the implants used were cementless. Routine antibiotics and venous thrombosis prophylaxis were administered.
A supine patient position and anterolateral approach were used in 63 patients, supine position and an extended trochanteric osteotomy (ETO) in nine patients and in nine patients where primary surgery was done from a posterior approach a lateral decubitus position and posterior approach were used. The acetabular implant was used for different conditions: isolated acetabular component revision for aseptic loosening in 35 cases, revision of both acetabular and femoral components in 31 cases (Fig. 1), conversion of hemiarthroplasties for acetabular defect in three cases, Girdlestone hip (after both femoral and acetabular component explantation for septic loosening in a previous session) in eight cases (Fig. 2) and revision of the acetabular component for recurrent dislocation in four cases.
AP radiograph of a 72-year-old woman who formerly underwent four surgeries for septic complications of THA, Delta One TT with 12-mm HM, additional fixation screws and modular titanium revision stem. a 16 months after extraction of both components for septic complications, referred for revision, b postoperative radiograph, c 48 months after revision
Acetabular defects were classified according to Paprosky [10]. There were nine patients revised for type 1, 11 for type 2A, 27 for type 2B, six for type 2C, 15 for type 3A and 13 for type 3B acetabular defects. Patients revised for recurrent dislocation were graded as type 1.
After acetabular component extraction and soft tissue removal, the residual acetabular cavity was reamed. Defects were evaluated and dressed by bone grafts. Fresh frozen sterile femoral head allografts from a tissue bank were used. Trabecular bone chips were prepared in a standardised manner to receive spongy bone block cubes of 4–5 mm each. Bone chips alone were used in 53 cases. Reverse reaming was performed until an even and firm bed on the bottom of the acetabulum was achieved, in which it was possible to implant a Delta TT construct. In three cases where a primary THA for post-dysplastic osteoarthritis (OA) was formerly placed into a high hip rotation, a bulk allograft was used. A femoral head bulk allograft shaped to fit the defect created by incorrect primary THA placement was fixed with two screws to the iliac bone. A stable rim for the Delta One TT implant was created in these three hips.
Trial implants corresponding to a specific Delta TT implant were used to fit to the prepared acetabulum. Delta TT were used in 19 patients, Delta One TT in 49 and Delta Revision TT in 13. Delta TT is a hemispherical cup, with the possibility of cup screw fixation to the acetabulum (cup screw fixation is possible for all of the Delta TT implants). Two to five screws were used in each case. Delta One TT (Fig. 1) is a cup, part of a hemisphere, reduced in size to fit in special conditions, usually in revision surgery and in dysplasia, with the possibility of expanding its outer shell surface with a so-called hemispherical module (HM). The HM is fixed together with two screws with the Delta One TT and with three screws in the Delta Revision TT implant. The interface between TT and HM is stable, and no cement is added between the junction. There are two sizes of HM with a height of 12 and 18 mm. Both heights of HM are available from a cup diameter of 50 mm in 4-mm increments for Delta One TT and Delta Revision TT. HM are made of pure TT. Delta Revision TT is a cage construct with a hook and three arms to obtain accessory stability of the implant. It is possible to achieve additional stability of the construct from outside of the acetabulum using screws through the holes of the arms. Three to five screws were used for the arm plate fixation. The whole spectrum of revision cup diameters was implanted (Table 1).
Fourteen HM were used with a height of 12 mm and two with a height of 18 mm. Fourteen HM were used with Delta One TT and two with Delta Revision TT. Delta TT implants were implanted in the direction in which maximal coverage by remnant bone was possible. Delta One TT and Delta Revision TT implants can be augmented with spacers, so additional coverage of the prosthetic head by 10–20° is enabled. Metal spacers with 10° coverage were used in five and with 20° in one case. Polyethylene (PE) inlays with additional 20° coverage were used in 21 surgeries. Metal spacers that lateralise the centre of rotation by 5 mm were used in three cases, metal spacers with 10° and + 5 mm in one and metal spacers with 20° + 5 mm in one, in which it was necessary to achieve stability of the total hip where the femoral component was not revised. All current designs of tribological surfaces were used, including five dual mobility articulations in specific diameters. Both PE and ceramic inlays were used in standard articulation head diameters of 28, 32, 36 and 40 mm (Table 2). No constrained liners were used.
Postoperatively, patients were advised to follow standard hip precautions. Touch weight-bearing was allowed after surgery for six weeks, after which partial weight-bearing was allowed, followed by full weight-bearing after 12 weeks. Patients were reviewed and X-rays were performed at six and 12 weeks, six months, 12 months and annually afterwards.
Vertical, medial and rotational migration of the acetabular cup were assessed, with the follow-up X-ray after six weeks as baseline. The following radiographic criteria were used to describe cup failure: migration of 5 mm either horizontally or vertically [11], radiolucent lines of 2 mm or more in all DeLee-Charnley zones, fracture of screws or variation of cup angle greater than 5°. Radiographs were screened for progressive radiolucent lines.
The functional Merle d’Aubigné-Postel score [12] modified by Charnley [13] was used for clinical evaluation. The score concedes a maximum of 6 points each for pain and walking ability, with a highest score of 12 points. A score of 11 and 12 points was regarded as a very good result, 10 points as a good result, 9 points as a medium result, 8 points as a fair result and 7 points and below as a poor result.
Results
A total of 80 patients were included in the study, in which 81 acetabular components were revised using TT implants. A 69-year-old man died after myocardial infarction on the fifth postoperative day after revision surgery for Girdlestone hip and was excluded from the study. One patient died of unrelated causes 37 months postoperatively and was included in the study. The mean follow-up period was 38.14 months (24–62) and was complete.
The mean preoperative modified Merle d’Aubigné-Postel functional score was 4.77 and 9.78 at last follow-up. Of the patients, 22 (27.5 %) achieved a very good, 21 (26.25 %) a good and 27 (33.75 %) a medium result, respectively. A fair functional result, mainly due to walking ability, was observed in ten patients (12.5 %). A mean pain score of 5.45 (range 3–6) and a mean walking score of 4.33 (3–6) were recorded at last follow-up.
There has been one revision in the postoperative period due to instability of the acetabular component. A cage system—Delta Revision TT—was successfully used for revision. During acetabular revision of a Paprosky type 2B defect, inadequate bone support was obtained. The remaining host acetabular bone was of poor quality, sclerotic and without signs of haemorrhage at revision. Cancellous bone allografts were used; the acetabulum and the superolateral defect were shaped to fit the implant. Delta One TT size 50 with a 12-mm HM and 20° metal augment was used, additional fixation was achieved using three cancellous screws and relatively stable implantation was achieved. On the postoperative X-ray and during follow-up at weeks six and 12 an unstable situation with acetabular protrusion was observed. HM fracture occurred in the line of the HM screw holes for additional fixation. During re-revision we found a protruded acetabular component with the medial part of the HM, the lateral broken part of the HM being fully osseointegrated and so were the allografts around the former superolateral defect. The Delta One TT with the medial fractured part of the HM were extracted, and the incorporated lateral part was left in situ. Reaming to 58 mm, adding a small amount of spongy bone allograft with reverse reaming and implanting a Delta Revision TT 58 without additional HM or augments led to and uneventful recovery. A stable situation was achieved, no migration was noted and full weight-bearing was allowed at 12 weeks after re-revision.
Except for one case of recurrent instability, appearing 13 months after revision surgery of both components, in which femoral component subsidence was the reason for dislocation, no other dislocations occurred. The patient was treated with revision of the femoral component with an uncemented modular stem. The acetabular component at the time of re-revision was stable, without necessity for replacement.
There was no case of acetabular perioperative fracture. There were no more cases of modular prosthesis disengagement or component breakage. No PE or ceramic liner dislocations were observed. Symptomatic venous thrombosis or pulmonary embolism did not occur. No deep infection was noted. Radiographic evaluation of postoperative X-rays was analysed in all of the revised cases, comparing the postoperative roentgenogram at baseline with controls at subsequent follow-up visits.
Three hips with Paprosky type 3B defect in which a Delta Revision TT construct was used with massive allograft bone grafting showed cranial migration of the acetabular component on the 12-week follow-up roentgenogram. In all three cases, the cranial migration achieved 6 mm and stabilised at this level after 6 months. At the latest follow-up, no signs of radiographic cup loosening were present. No progressive radiolucent lines were present. All implanted HM showed signs of full osseointegration.
Discussion
Addressing acetabular bone defects at the time of revision of the THA is the key factor for a successful outcome in hip revision surgery. TT Delta cups are a new implant type designed to solve diverse acetabular bone defects. Their use in acetabular revisions has not been reported previously.
Primary stability achieved during surgery and in the early postoperative period, followed by secondary stability after bone ingrowth in cases of uncemented acetabular implants, are the goals of treatment. Cementless acetabular revision implants show better performance compared to cemented revision implants [14–16]. Good results in hip revisions have been published using cementless hemispherical cups in defects with minimal bone deficiency, and also in cases where structural support was reconstructed with or without the use of structural allografts [10]. To increase biological fixation of conventional metal cups various surface coatings are used. These bioactive surfaces enable only bone ongrowth on the cup. Mesenchymal stem cells (MSC) improved acetabular bone graft healing. Revisions for major bone loss using allografts supercharged with MSC diminished the re-revision rate compared to a control group by 30 % [17].
Oblong revision cups prevent the use of bulky allografts in acetabular defects. Midterm results showing reliable primary fixation and computed tomography-documented osseointegration with specially designed oblong revision cups and good clinical results have been published recently [18].
Custom triflange acetabular components (CTAC) were designed for managing bone defects without using massive structural bone allografts. CTAC are an option to solve major bone defects in revision surgery. Their price, time delay needed for manufacturing, limited options of cup orientation and limited choice of bearing surfaces are drawbacks to widespread use of this device [19]. Modular acetabular reconstructive cups will overcome some of the drawbacks of CTAC prostheses. Very good long-term results using modular cups have been published recently [20], though generalisation of the study outcome might be limited to an Asian patient population.
Data for tantalum trabecular metal uncemented cups have been available since 2005 [5], showing good stability and ingrowth of the prosthesis. The revision rate in this group was relatively high: seven revisions in 60 patients were done, five for dislocation and one each for initial cup movement and for aseptic loosening. Most of the cups (55/60) were implanted without ancillary screws. Application of modular TM cups expanded indications for use of TM in the presence of major acetabular bone loss. Good survival rates of TM shells have been demonstrated even in revisions for severe bone loss [21, 22]. The concept of a cancellous porous metal surface enabling bone ingrowth was demonstrated [21, 23].
TM demonstrated supreme material and biomechanical properties in the last decade [23]. These tantalum implants are clearly beneficial compared to previously used roof reinforcement rings and cages in the presence of a large acetabular defect [24, 25].
Tantalum porous surface cups have shown lower mechanical failure rates compared to hydroxyapatite-coated titanium cups in minor bone defects (6 and 8 %, respectively); this was more pronounced in hips with major bone deficiency (12 % for tantalum and 24 % for titanium cups) [26]. The same study reported that 80 % of tantalum cups failed in the first six months after revision surgery as opposed to 82 % of titanium cups that failed after six months or later. These findings support the beneficial osseointegration properties of trabecular metal in comparison to hydroxyapatite-coated titanium shells.
The recently published results of TM shells, with or without porous metal augments, show survival rates of 87–99.2 %; the mean follow-up in these studies was 36–74 months [21, 27]. Systematic literature reviews show revision rates for TM compared with revision rings were significantly reduced [25].
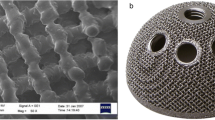
Titanium is a light transition metal with low density and high strength. Titanium alloys have been successfully used for decades for orthopaedic and dental prostheses. TT is a specific hexagonal space porous material with high osteoinductive and osteoconductive properties and biocompatibility that lead to rapid and extensive bone ingrowth into the material [8, 9]. Special attributes of TT—its porosity, high friction coefficient, tensile strength and high corrosion resistance—are extraordinary material characteristics that enable the use of TT in situations where bone defects in weight-bearing skeletal parts are required. Data on superiority of the material properties of TT over current orthopaedic implant materials, including other trabecular structured materials, have been published [8, 28]. TT enables high primary stability of revision acetabular implants with its high endurance, rapid bone ingrowth and possibility of fast restitution of full weight-bearing.
Delta TT implants, which are produced from TT, are produced by electron beam melting technology. That means a Delta TT acetabular implant has no coating, but the acetabular component has a solid structure on cross section. There are three types of Delta TT acetabular components:hemispherical Delta TT cup (the only one that may not be used together with HM) , Delta One TT, a versatile cup offering enhanced coverage in special, i.e. dysplastic or revision cases, and Delta Revision TT, a cup-cage construct for massive bone loss. Delta One TT and Delta Revision TT can be combined together with a so-called HM. The HM can be placed in three positions on the superolateral part of the cup to fill the acetabular defect. Connexion between the cup and HM is secured by screws and no acrylic cement is used on their junction. Screw fixation from inside of the TT component is possible to gain additional implant stability. Compared to bone graft TT HM has no risk of collapse due to bone resorption. Reducing the use of bulk bone allografts in major acetabular bone loss by TT HM seems to be one of the reasons for the lower subsequent re-revision rate in our study.
Inserts can be used to add coverage of 10 or 20°. There is an option to lateralise the centre of rotation on the side of the cup by 5 mm in each of the cases; this enables additional offset tissue tensioning, a facility appreciated in situations where the femoral component is not revised. All current bearing surfaces can be used, in all standard diameters, including double mobility. The modularity of the Delta TT enables one to use ceramic inserts in different diameters, even if additional coverage up to 20° is required. This ample armamentarium addresses most of the situations for secure acetabular revision and reduced the dislocation rate in our study, even without using constrained liners. Material properties associated with TT are high friction and high porosity, therefore minimising micromotion and diminishing possible fibrous tissue formation around the revision implant. Thermal necrosis and possible cement disruption are reduced by the cementless design.
To our knowledge this is the first time that results of TT implants have been presented. The follow-up period is relatively short with a mean of 38.14 months. However, a favourable long-term outcome is expected because of the low perioperative and postoperative complication rate and favourable clinical and radiological scores.
Of 80 observed procedures, bone allografts were used in 56 of the cases. Substantial bone healing and bone remodelling were seen on both sides of the TT cup and host bone interface. Three cases of acetabular cup subsidence to 6 mm were noted in the Delta Revision TT cup-cage construct. They stabilised six months after revision surgery and progression was not registered at subsequent radiological controls. In one case a revision was required. During re-revision 12 weeks after the index revision procedure, the lateral broken part of the HM was found fully osseointegrated and supportive. The medial broken part was extracted and the lateral part was left in situ. During the second revision massive allograft bone chips were impacted. Delta Revision TT was implanted and revision led to successful recovery. Revision of a fully osseointegrated TT component under unavoidable conditions, like septic complications, would be a demanding procedure. We would advise the use of appropriate instruments for cementless acetabular component explantation.
Our results using TT implants for aseptic loosening are similar [22] or superior [5, 7, 29] to results published on TM [5]. Concerns of a high dislocation rate following revision hip procedures are justified. Optimal cup placement into the safe zone during acetabular revision for severe bone loss is difficult to obtain [30]; therefore, supplemental cup reorientation with a modular acetabular prosthesis is advantageous. The only late dislocation in our study was revised due to femoral revision stem subsidence. No acetabular revision in our study using the modular acetabular TT implant for dislocation seems to show that adequate joint stability was achieved. Comparing the TM data on revision for dislocation, the modular TT implant shows better performance [5, 7, 22, 29, 31]. There have been no septic complications registered in the whole study group, which again favours use of TT over TM implants [7, 22, 31]. TT cups in revision surgery show good osseointegration without signs of cup instability. There have been no inferior results in cups where HM were used, and no failures due to cup modularity design were noticed.
The results of acetabular reconstruction using the Delta TT are encouraging. TT cups, HM and augments facilitate reliable and reproducible biological fixation in acetabular revision surgery. Despite this long-term follow-up of the cases presented, it is necessary to obtain a deeper perspective of the long-term behaviour of TT modular implants.
References
Necas L, Katina S, Uhlarova J, Colton CL (2013) Survival analysis of total hip and knee arthroplasty in Slovakia 2003–2011. Acta Chir Orthop Traumatol Cech 80(Suppl):9–67
Jain S, Grogan RJ, Giannoudis PV (2014) Options for managing severe acetabular bone loss in revision hip arthroplasty. A systematic review. Hip Int 24:109–122
Gill TJ, Sledge JB, Müller ME (1998) The Bürch-Schneider anti-protrusio cage in revision total hip arthroplasty: indications, principles and long-term results. J Bone Joint Surg Br 80:946–953
Herrera A, Martínez AA, Cuenca J, Canales V (2006) Management of types III and IV acetabular deficiencies with the longitudinal oblong revision cup. J Arthroplasty 21:857–864
Unger AS, Lewis RJ, Gruen T (2005) Evaluation of porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty 20:1002–1009
Paprosky WG, Sporer SS, Murphy BP (2007) Addressing severe bone deficiency: what a cage will not do. J Arthroplasty 22(4 Suppl 1):111–115
Abolghasemian M, Tangsataporn S, Sternheim A, Backstein D, Safir O, Gross AE (2013) Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint J 95-B:166–172
Marin E, Fusi S, Pressaco M, Paussa L, Fedrizzi L (2010) Characterization of cellular solids in TiAl4V for orthopaedic implant applications: trabecular titanium. J Mech Behav Biomed Mater 3:373–381
Benazzo F, Botta L, Scaffino MF et al (2014) Trabecular titanium can induce in vitro osteogenic differentiation of human adipose derived stem cells without osteogenic factors. J Biomed Mater Res A 102:2061–2071. doi:10.1002/jbm.a.34875
Paprosky WG, Perona PG, Lawrence JM (1994) Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 9:33–44
Massin P, Schmidt L, Engh CA (1989) Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty 4:245–251
D’Aubigne RM, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36:451–475
Charnley J (1979) Low friction arthroplasty. Theory and practice. Springer, New York
Paprosky WG, Magnus RE (1991) Classification and treatment of the failed acetabulum: a systematic approach. Contemp Orthop 22:121–130
Paprosky WG, Bradford MS, Younger TI (1994) Acetabular reconstruction with massive allograft and cementless prosthesis. Chir Organi Mov 79:379–386
Pulido L, Rachala SR, Cabanela ME (2011) Cementless acetabular revision: past, present and future. Revision total hip arthroplasty: the acetabular side using cementless implants. Int Orthop 35:289–298
Hernigou P, Pariat J, Queinnec S et al (2014) Supercharging irradiated allografts with mesenchymal stem cells improves acetabular bone grafting in revision arthroplasty. Int Orthop. doi:10.1007/s00264-014-2285-2
Št’astný E, Trč T, Handl M et al (2014) Mid-term results of revision total hip arthroplasty using the oval-shaped uncemented Trč-Cingr cup. Int Orthop 38:935–940
Dennis DA (2003) Management of massive acetabular defects in revision total hip arthroplasty. J Arthroplasty 18(Suppl):121–125
Sakai T, Ohzono K, Nishii T et al (2013) Modular acetabular reconstructive cup in acetabular revision total hip arthroplasty at a minimum ten year follow-up. Int Orthop 37:605–610
Davies JH, Laflamme GY, Delisle J, Fernandes J (2011) Trabecular metal used for major bone loss in acetabular hip revision. J Arthroplasty 26:1245–1250
Flecher X, Sporer S, Paprosky W (2008) Management of severe bone loss in acetabular revision using a trabecular metal shell. J Arthroplasty 23:949–955
Macheras GA, Papageloupoulos PJ, Kateros K, Kostakos AT, Baltas D, Karachalios TS (2006) Radiological evaluation of the metal-bone interface of a porous tantalum monoblock acetabular component. J Bone Joint Surg Br 88:304–309
Jaffari SM, Bender B, Coyle C et al (2010) Do tantalum and titanium cups show similar results in revision hip arthroplasty? Clin Orthop Relat Res 468:459–465
Beckmann NA, Weiss S, Klotz MC, Gondan Mm Jaeger S, Bitsch RG (2014) Loosening after acetabular revision: comparison of trabecular metal and reinforcement rings. A systematic review. J Arthroplasty 29:229–235
Meneghini RM, Meyer C, Buckley CA, Hanssen AD, Lewallen DG (2010) Mechanical stability of novel highly porous metal acetabular components in revision total hip arthroplasty. J Arthroplasty 25:337–341
Skyttä ET, Eiskelinen A, Paavolainen PO, Remes VM (2011) Early results of 827 trabecular metal revision shells in acetabular revision. J Arthroplasty 26:342–345
Shultz TR, Blaha JD, Gruen TA, Norman TL (2006) Cortical bone viscoelasticity and fixation strength of press-fit femoral stems: finite element model. J Biomech Eng 128:7–12
Simon JP, Bellemans J (2009) Clinical and radiological evaluation of modular trabecular metal acetabular cups. Short-term results in 64 hips. Acta Orthop Belg 75:623–630
Choi H, Anderson A, Foster S et al (2013) Acetabular cup positioning in revision total hip arthroplasty with Paprosky type III defects: Martell radiographic analysis. Int Orthop 37:1905–1910
Sternheim A, Backstein D, Kuzyk PRT, Goshua G, Berkowich Y, Safir O, Gross AE (2012) Porous metal revision shells for management of contained acetabular bone defects at a mean follow-up of six years: a comparison between up to 50% bleeding host bone contact and more than 50% contact. J Bone Joint Surg Br 94:158–162
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Steno, B., Kokavec, M. & Necas, L. Acetabular revision arthroplasty using trabecular titanium implants. International Orthopaedics (SICOT) 39, 389–395 (2015). https://doi.org/10.1007/s00264-014-2509-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2509-5