Abstract
Introduction
The standard therapy of intra-articular and extra-articular distal radius fractures consists of open reduction and stabilization using palmar osteosynthesis with an angularly stable plate. The integrity of the flexor pollicis longus tendon (FPLT) may be mechanically affected by the plate, with rupture rates between 1 and 12% reported in the literature, occurring during a postoperative time period from 4 to 120 months. The aim of this study was to investigate the position of the tendon in relation to the distal edge of the plate using high-resolution ultrasonic imaging.
Materials and methods
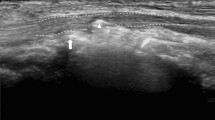
Nineteen patients undergoing osteosynthesis for distal radius fracture in 2015 with the Medartis® APTUS® FPL plate were included in this study. Of these, seven dropped out for various reasons. Therefore, twelve patients with a median age of 52 years (range 24–82 years) were included in the final analysis. High-frequency ultrasound was performed within a median of 28 (range 10–52) weeks by an experienced radiology specialist to locate the FPLT position in two separate wrist positions: (1) wrist held in 0° position and fingers extended and (2) wrist held in 45° of dorsal extension and actively flexed fingers II to V (functional position). For analysis, we used the axial ultrasound videos. Postoperative X-rays and CT scans were included for the analysis, especially the soft-tissue CT scan window for the exact localization of the FPLT. Dynamic ultrasound scanning was used to localize the FPLT in relation to the plate in 0° and functional position of the hand. Using CT scanning, the position of the plate relative to the bone was determined. In this way, we were able to correlate the functional FPLT position with the osseous structures of the distal radius.
Results
In all cases, the FPLT was positioned closer to the volar distal edge of the FPL plate in functional position than in 0° position. In four cases, the FPLT did not touch the plate at all and was shown to shift diagonally from radio-volar in ulno-dorsal direction during wrist movement from 0° to functional position, similarly to the sliding of the tendon in the assumed physiological motion sequence. In these cases, in the functional position the center of the FPLT was positioned slightly ulnarly of the center of the distal radius (i.e., less than 50% of the distal radius width measured from the radial border of DRUJ), and positioned more ulnarly than in all other cases (i.e., in which the FPLT came into contact with the plate). In the remaining two-thirds of the cases (eight patients), the FPLT touched the plate during wrist movement from 0° to functional position, shifted in dorsal direction and slid into the plate indentation, irrespective of whether the tendon entered the indentation from the radial or the ulnar side, and independent of the ulnoradial position of the plate. No signs of tendinopathy of the FPLT were found in any of the cases.
Conclusion
The results show that the indentation of the Medartis® APTUS® FPL plate reduces the tendon-plate contact and ideally even prevents it entirely. In particular, ulnar positioning of the plate lowers the risk of tendon-plate contact. If the FPLT touches the plate, the tendon pulls into the plate indentation, thus lowering the contact. Consequently, the Soong criteria are not applicable when a FPL plate is used.








Similar content being viewed by others
References
Mehling I, Meier M, Schlör U, Krimmer H (2007) Multidirektionale winkelstabile versorgung der instabilen distalen Radiusfraktur. Handchirurgie Mikrochirurgie Plast Chir 39:29–33. https://doi.org/10.1055/s-2007-964933
Figl M, Weninger P, Jurkowitsch J et al (2010) Unstable distal radius fractures in the elderly ratient-volar fixed-angle plate osteosynthesis prevents secondary loss of reduction. J Trauma Inj Infect Crit Care 68:992–998. https://doi.org/10.1097/TA.0b013e3181b99f71
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2016) Early rehabilitation of distal radius fractures stabilized by volar locking plate: a prospective randomized pilot study. J Wrist Surg 06:102–112. https://doi.org/10.1055/s-0036-1587317
Quadlbauer S, Leixnering M, Jurkowitsch J et al (2017) Volar radioscapholunate arthrodesis and distal scaphoidectomy after malunited distal radius fractures. J Hand Surg Am 42:754.e1–754.e8. https://doi.org/10.1016/j.jhsa.2017.05.031
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2017) Spontaneous radioscapholunate fusion after septic arthritis of the wrist: a case report. Arch Orthop Trauma Surg 137:579–584. https://doi.org/10.1007/s00402-017-2659-1
Schermann H, Kadar A, Dolkart O et al (2018) Repeated closed reduction attempts of distal radius fractures in the emergency department. Arch Orthop Trauma Surg 138:591–596. https://doi.org/10.1007/s00402-018-2904-2
Borisch N, Jacob HA (2015) Wrist kinematics after radiolunate arthrodesis. Arch Orthop Trauma Surg 135:1033–1041. https://doi.org/10.1007/s00402-015-2244-4
Xu W, Ni C, Yu R et al (2017) Risk factors for distal radius fracture in postmenopausal women. Orthopade 46:447–450. https://doi.org/10.1007/s00132-017-3403-9
Unglaub F, Langer MF, Hohendorff B et al (2017) Distale radiusfraktur. Orthopade 46:93–110. https://doi.org/10.1007/s00132-016-3347-5
Quadlbauer S, Pezzei C, Hintringer W et al (2018) Clinical examination of the distal radioulnar joint. Orthopade 47:628–636
Esenwein P, Sonderegger J, Gruenert J et al (2013) Complications following palmar plate fixation of distal radius fractures: a review of 665 cases. Arch Orthop Trauma Surg 133:1155–1162
Hohendorff B, Knappwerth C, Franke J et al (2018) Pronator quadratus repair with a part of the brachioradialis muscle insertion in volar plate fixation of distal radius fractures: a prospective randomised trial. Arch Orthop Trauma Surg 138:1479–1485. https://doi.org/10.1007/s00402-018-2999-5
Rubin G, Orbach H, Chezar A, Rozen N (2017) Treatment of physeal fractures of the distal radius by volar intrafocal Kapandji method: surgical technique. Arch Orthop Trauma Surg 137:49–54. https://doi.org/10.1007/s00402-016-2592-8
Gabl M, Arora R, Klauser AS, Schmidle G (2016) Characteristics of secondary arthrofibrosis after intra-articular distal radius fracture. Arch Orthop Trauma Surg 136:1181–1188. https://doi.org/10.1007/s00402-016-2490-0
Krimmer H, Unglaub F, Langer MF, Spies CK (2016) The distal radial decompression osteotomy for ulnar impingement syndrome. Arch Orthop Trauma Surg 136:143–148. https://doi.org/10.1007/s00402-015-2363-y
Krimmer H (2018) [Treatment of the ulnar impingement syndrome in the distal radioulnar joint]. Orthopade 47:684–687. https://doi.org/10.1007/s00132-018-3592-x
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2018) Early complications and radiological outcome after distal radius fractures stabilized by volar angular stable locking plate. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-018-3051-5
Drobetz H, Kutscha-Lissberg E (2003) Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop 27:1–6. https://doi.org/10.1007/s00264-002-0393-x
Casaletto JA, Machin D, Leung R, Brown DJ (2009) Flexor Pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg (European) 34:471–474. https://doi.org/10.1177/1753193408100964
Asadollahi S, Keith PPA (2013) Flexor tendon injuries following plate fixation of distal radius fractures: a systematic review of the literature. J Orthop Traumatol 14:227–234. https://doi.org/10.1007/s10195-013-0245-z
Erhart S, Toth S, Kaiser P et al (2018) Comparison of volarly and dorsally displaced distal radius fracture treated by volar locking plate fixation. Arch Orthop Trauma Surg 138:879–885. https://doi.org/10.1007/s00402-018-2925-x
Naito K, Sugiyama Y, Igeta Y et al (2014) Irreducible dislocation of the thumb interphalangeal joint due to displaced flexor pollicis longus tendon: case report and new reduction technique. Arch Orthop Trauma Surg 134:1175–1178. https://doi.org/10.1007/s00402-014-2024-6
Ulrich D, Piatkowski A, Pallua N (2011) Anterior interosseous nerve syndrome: retrospective analysis of 14 patients. Arch Orthop Trauma Surg 131:1561–1565. https://doi.org/10.1007/s00402-011-1322-5
Agnew SP, Ljungquist KL, Huang JI (2015) Danger zones for flexor tendons in volar plating of distal radius fractures. J Hand Surg Am 40:1102–1105. https://doi.org/10.1016/j.jhsa.2015.02.026
Matityahu AM, Lapalme SN, Seth A et al (2013) How placement affects force and contact pressure between a volar plate of the distal radius and the flexor pollicus longus tendon: a biomechanical investigation. J Hand Surg Eur 38:144–150. https://doi.org/10.1177/1753193412453436
Figl M, Weninger P, Liska M et al (2009) Volar fixed-angle plate osteosynthesis of unstable distal radius fractures: 12 months results. Arch Orthop Trauma Surg 129:661–669. https://doi.org/10.1007/s00402-009-0830-z
Kuen FC, Khalid M, Gogi N et al (2008) The mend of the bend-flexor pollicis longus tendon has an additional pulley distal to its point of angulation. Clin Anat 21:427–432. https://doi.org/10.1002/ca.20637
Ham SJ, Konings JG, Wolf RFE, Mooyaart EL (1993) Functional anatomy of the soft tissues of the hand and wrist: in vivo excursion measurement of the flexor pollicis longus-tendon using MRI. Magn Reson Imaging 11:163–167. https://doi.org/10.1016/0730-725X(93)90020-E
Sandow MJ, Fisher TJ, Howard CQ, Papas S (2014) Unifying model of carpal mechanics based on computationally derived isometric constraints and rules-based motion—the stable central column theory. J Hand Surg Eur 39:353–363. https://doi.org/10.1177/1753193413505407
Nanno M, Sawaizumi T, Kodera N et al (2015) Ultrasound evaluation of the transverse movement of the flexor pollicis longus tendon on the distal radius during wrist and finger motion in healthy volunteers. J Nippon Med Sch 82:220–228. https://doi.org/10.1272/jnms.82.220
Kaufman KR, An KN, Litchy WJ et al (1999) In-vivo function of the thumb muscles. Clin Biomech 14:141–150. https://doi.org/10.1016/S0268-0033(98)00058-8
Young RW (2003) Evolution of the human hand: the role of throwing and clubbing. J Anat 202:165–174
Lee JC, Healy FJC (2005) Anatomy of the wrist and hand. Radiographics 25:1577–1590. https://doi.org/10.1148/rg.256055028
Bianchi S, Martinoli C, Montet X, Fasel JHD (2003) Hand- und handwurzel-ultraschall. Radiologe 43:831–840
The Association for American Ultrasound (2012) AIUM practice parameter for the performance of a musculoskeletal ultrasound examination. Am Inst Ultrasound Med 31:301–498
Olubaniyi BO, Bhatnagar G, Vardhanabhuti V et al (2013) Comprehensive musculoskeletal sonographic evaluation of the hand and wrist. J Ultrasound Med 32:901–914
Müller ME, Koch P, Nazarian S, Schatzker J (1990) Tibia/Fibula = 4. In the comprehensive classification of fractures of long bones. Springer, Berlin, pp 148–191
Soong M, Earp BE, Bishop G et al (2011) Volar locking plate implant prominence and flexor tendon rupture. J Bone Jt Surg Ser A 93:328–335. https://doi.org/10.2106/JBJS.J.00193
Herisson O, Delaroche C, Maillot-Roy S et al (2017) Comparison of lateral and skyline fluoroscopic views for detection of prominent screws in distal radius fractures plating: results of an ultrasonographic study. Arch Orthop Trauma Surg 137:1357–1362. https://doi.org/10.1007/s00402-017-2759-y
Diwersi N, Babst R, Link B-C (2016) Miniplates as augmentation implants in osteosynthesis of complex distal radial fractures. Oper Orthop Traumatol 28:402–406. https://doi.org/10.1007/s00064-016-0469-1
Lutz M, Erhart S, Deml C, Klestil T (2016) Arthroskopisch gesteuerte Osteosynthese der dislozierten intraartikulären distalen Radiusfraktur. Oper Orthop Traumatol 28:279–290. https://doi.org/10.1007/s00064-016-0448-6
Pillukat T, Fuhrmann R, Windolf J, van Schoonhoven J (2016) Die palmare winkelstabile plattenosteosynthese bei extensionsfrakturen des distalen radius. Oper Orthop Traumatol 28:47–64. https://doi.org/10.1007/s00064-015-0433-5
Schmidle G, Arora R, Gabl M (2012) Ulnar shortening with the ulna osteotomy locking plate. Oper Orthop Traumatol 24:284–292. https://doi.org/10.1007/s00064-011-0037-7
Tünnerhoff H-G (2018) Suture techniques for TFCC. Orthopade 47:655–662. https://doi.org/10.1007/s00132-018-3595-7
Wolfe SW, Crisco JJ, Orr CM, Marzke MW (2006) The dart-throwing motion of the wrist: is it unique to humans? J Hand Surg Am 31:1429–1437. https://doi.org/10.1016/j.jhsa.2006.08.010
Garg R, Kraszewski AP, Stoecklein HH et al (2014) Wrist kinematic coupling and performance during functional tasks: effects of constrained motion. J Hand Surg Am 39:634–642.e1. https://doi.org/10.1016/j.jhsa.2013.12.031
Mann FA, Kang SW, Gilula LA (1992) Normal palmar tilt: is dorsal tilting really normal? J Hand Surg Am 17:315–317. https://doi.org/10.1016/0266-7681(92)90120-Q
Napier JR (1956) The prehensile movements of the human hand. J Bone Joint Surg Br 38–B:902–913
Kara A, Celik H, Bankaoglu M et al (2016) Ultrasonic evaluation of the flexor pollicis longus tendon following volar plate fixation for distal radius fractures. J Hand Surg Am 41:374–380. https://doi.org/10.1016/j.jhsa.2015.11.022
Funding
Linda Schlickum, M.D. attended the International Bone Research Association (IBRA) scholarship program C for carrying out this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Linda Schlickum, M.D. attended the International Bone Research Association (IBRA) scholarship program C for carrying out this study. All other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional review board approval was obtained for this study.
Rights and permissions
About this article
Cite this article
Schlickum, L., Quadlbauer, S., Pezzei, C. et al. Three-dimensional kinematics of the flexor pollicis longus tendon in relation to the position of the FPL plate and distal radius width. Arch Orthop Trauma Surg 139, 269–279 (2019). https://doi.org/10.1007/s00402-018-3081-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3081-z