Abstract
Introduction
Failure rates after arthroscopic rotator cuff repair remain high. Platelet-rich plasma has gained interest as a potential biological augmentation to enhance bone–tendon healing. The purpose of this study is to evaluate the clinical and structural outcomes of repeated PRP application on rotator cuff repair.
Materials and methods
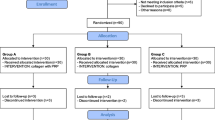
Thirty-six patients underwent arthroscopic reconstruction, using knotless anchor double-row repair. Eighteen patients [10 female, 8 male; 61.2 (±9.2) years] received two applications of PRP—directly subsequent to the repair and 7 days postoperatively. Eighteen patients [11 male, 7 female; 61.4 (±6.5) years] who solely received the same technique of rotator cuff repair were matched for age. The subjective shoulder value, WORC, and the Constant–Murley score were used for clinical evaluation. MRI was performed for tendon integrity, and cuff appearances were graded according to the Sugaya classification.
Results
We prospectively evaluated the PRP group with a minimum follow-up of 24 months. Clinical results did not show significantly differences in comparison to patients with isolated rotator cuff repair concerning CS (79 ± 13 vs. 77 ± 13; P = 0.6), SSV (90 ± 14 vs. 88 ± 16; P = 0.5) or WORC Score (90 ± 18 vs. 86 ± 20; P = 0.2). At the final follow-up, MRI showed retears in 11 % of the PRP and in 28 % of the control group (P = 0.4).
Conclusions
Knotless-anchor double-row repair shows good to excellent clinical results with an acceptable retear rate. Additional two-staged PRP application failed to significantly improve clinical parameters. Even though there was a trend for lower retear rates in the PRP group, it did not achieve statistical difference.
Level of evidence
Level III, Retrospective comparative study.


Similar content being viewed by others
References
Scheibel M (2012) Recurrent defects of the rotary cuff: causes and therapeutic strategies. Oper Orthop Traumatol 24:458–467. doi:10.1007/s00064-012-0179-2
Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA (2012) Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy 28:429–439. doi:10.1016/j.arthro.2011.10.018
McCarrel TM, Mall NA, Lee AS, Cole BJ, Butty DC, Fortier LA (2014) Considerations for the use of platelet-rich plasma in orthopedics. Sports Med 44:1025–1036. doi:10.1007/s40279-014-0195-5
Blair P, Flaumenhaft R (2009) Platelet alpha-granules: basic biology and clinical correlates. Blood Rev 23:177–189. doi:10.1016/j.blre.2009.04.001
Arnoczky SP, Delos D, Rodeo SA (2011) What is platelet-rich plasma? Oper Tech Sports Med 19:142–148. doi:10.1097/JSA.0b013e3182999712
Everts PAM, Knape JTA, Weibrich G, Schönberger JPAM, Hoffmann J, Overdevest EP, Box HAM, van Zundert A (2006) Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol 38:174–187
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Bateman JE (1963) The diagnosis and treatment of ruptures of the rotator cuff. Surg Clin North Am 43:1523–1530
Wang A, McCann P, Colliver J, Koh E, Ackland T, Joss B, Zheng M, Breidahl B (2015) Do postoperative platelet-rich plasma injections accelerate early tendon healing and functional recovery after arthroscopic supraspinatus repair? A randomized controlled trial. Am J Sports Med 43:1430–1437. doi:10.1177/0363546515572602
Scott A, Khan KM, Roberts CR, Cook JL, Duronio V (2004) What do we mean by the term “inflammation”? A contemporary basic science update for sports medicine. Br J Sports Med 38:372–380. doi:10.1136/bjsm.2004.011312
Tidball JG (2005) Inflammatory processes in muscle injury and repair. Am J Physiol-Regul Integr Comp Physiol 288:R345–R353. doi:10.1152/ajpregu.00454.2004
Huber W, Hofstaetter JG, Hanslik-Schnabel B, Posch M, Wurnig C (2005) Translation and psychometric testing of the Western Ontario Rotator Cuff Index (WORC) for use in Germany. Z Orthop Ihre Grenzgeb 143:453–460. doi:10.1055/s-2005-836677
Gilbart MK, Gerber C (2007) Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 16:717–721. doi:10.1016/j.jse.2007.02.123
Constant CR, and Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Sugaya H, Maeda K, Matsuki K, Moriishi J (2005) Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy 21:1307–1316. doi:10.1016/j.arthro.2005.08.011
Pauly S, Gerhardt C, Scheibel M (2015) Sehnenheilung nach Rotatorenmanschettenrekonstruktion. Obere Extremität 10:17–23. doi:10.1007/s11678-015-0305-5
Filardo G, Kon E, Roffi A, Di Matteo B, Merli ML, Marcacci M (2015) Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc 23(9):2459–2474. doi:10.1007/s00167-013-2743-1
Mazzocca AD, McCarthy MBR, Chowaniec DM, Cote MP, Romeo AA, Bradley JP, Arciero RA, Beitzel K (2012) Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am 94:308–316. doi:10.2106/JBJS.K.00430
Castricini R, Longo UG, De Benedetto M, Panfoli N, Pirani P, Zini R, Maffulli N, Denaro V (2011) Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. Am J Sports Med 39:258–265. doi:10.1177/0363546510390780
Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P (2011) Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg 20:518–528. doi:10.1016/j.jse.2011.02.008
Bergeson AG, Tashjian RZ, Greis PE, Crim J, Stoddard GJ, Burks RT (2012) Effects of platelet-rich fibrin matrix on repair integrity of at-risk rotator cuff tears. The Am J Sports Med 40:286–293. doi:10.1177/0363546511424402
Rodeo SA, Delos D, Williams RJ, Adler RS, Pearle A, Warren RF (2012) The effect of platelet-rich fibrin matrix on rotator cuff tendon healing: a prospective, randomized clinical study. Am J Sports Med 40:1234–1241. doi:10.1177/0363546512442924
Vavken P, Sadoghi P, Palmer M, Rosso C, Mueller AM, Szoelloesy G, Valderrabano V (2015) Platelet-rich plasma reduces retear rates after arthroscopic repair of small- and medium-sized rotator cuff tears but is not cost-effective. Am J Sports Med. doi:10.1177/0363546515572777
Barber FA, Hrnack SA, Snyder SJ, Hapa O (2011) Rotator cuff repair healing influenced by platelet-rich plasma construct augmentation. Arthroscopy 27:1029–1035. doi:10.1016/j.arthro.2011.06.010
Vavken P, Saad FA, Murray MM (2010) Age dependence of expression of growth factor receptors in porcine ACL fibroblasts. J Orthop Res 28:1107–1112. doi:10.1002/jor.21111
Kluger R, Bock P, Mittlböck M, Krampla W, Engel A (2011) Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med 39:2071–2081. doi:10.1177/0363546511406395
Hug K, Gerhardt C, Haneveld H, Scheibel M (2014) Arthroscopic knotless-anchor rotator cuff repair: a clinical and radiological evaluation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3026-1
Gerhardt C, Hug K, Pauly S, Marnitz T, Scheibel M (2012) Arthroscopic single-row modified mason-allen repair versus double-row suture bridge reconstruction for supraspinatus tendon tears: a matched-pair analysis. Am J Sports Med 40:2777–2785. doi:10.1177/0363546512462123
Gerhardt C, Scheibel M (2012) Arthroskopische Doppelreihenrekonstruktion bei Rotatorenmanschettenruptur. Arthroskopie 25:103–110. doi:10.1007/s00142-011-0667-7
Pauly S, Fiebig D, Kieser B, Albrecht B, Schill A, Scheibel M (2011) Biomechanical comparison of four double-row speed-bridging rotator cuff repair techniques with or without medial or lateral row enhancement. Knee Surg Sports Traumatol Arthrosc 19:2090–2097. doi:10.1007/s00167-011-1517-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
All authors would like to state that no outside funding or grants were received that assisted in the study.
Conflict of interest
Markus Scheibel and Christian Gerhardt are consultants for Arthrex. Upon that, Clemens Gwinner, Christian Gerhardt, Hendrik Haneveld, Markus Scheibel, their immediate family, and any research foundation with which they are affiliated state, that they have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Ethical statement
Institutional Review Board approval was provided by University Hospital Ethics Commission; No. EA1/264/15.
Additional information
C. Gwinner and C. Gerhardt contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Gwinner, C., Gerhardt, C., Haneveld, H. et al. Two-staged application of PRP in arthroscopic rotator cuff repair: a matched-pair analysis. Arch Orthop Trauma Surg 136, 1165–1171 (2016). https://doi.org/10.1007/s00402-016-2499-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2499-4