Abstract
Method
A Delphi study was conducted to obtain consensus on the most important criteria for the radiological evaluation of the reduction and fixation of the wrist and ankle. The Delphi study consisted of a bipartite online questionnaire, focusing on the interpretation of radiographs and CT scans of the wrist and the ankle. Questions addressed imaging techniques, aspects of the anatomy and fracture reduction and fixation. Agreement was expressed as the percentage of respondents with similar answers. Consensus was defined as an agreement of at least 90%.
Results
In three Delphi rounds, respectively, 64, 74 and 62 specialists, consisting of radiologists, trauma and orthopaedic surgeons from the Netherlands responded. After three Delphi rounds, consensus was reached for three out of 14 (21%) imaging techniques proposed, 11 out of the 13 (85%) anatomical aspects and 13 of the 22 (59%) items for the fracture reduction and fixation. This Delphi consensus differs from existing scoring protocols in terms of the greater number of anatomical aspects and aspects of fracture fixation requiring evaluation and is more suitable in clinical practice due to a lower emphasis on measurements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At present, there is no generally accepted scoring protocol for the radiological evaluation of the quality of wrist or ankle fracture reduction and fixation, despite various angle and distance measurements described in the literature. According to AO recommendations, anatomical fracture reduction is desired for an optimal clinical outcome of intra-articular fractures of the extremities [1]. For both ankle and wrist, there are also indications that anatomical fracture reduction gives a significantly better outcome [2–5]. Unfortunately, there is no consensus on which parameters predict symptomatic malunion and post-traumatic arthrosis most securely. Therefore, it remains unclear which criteria should be used to assess optimal fracture reduction and fixation.
For the wrist, the most common radiological parameters and their generally accepted thresholds for the reduction to be acceptable are radial shortening (<5 mm), radial inclination (>15°), sagittal tilt on lateral projection (between 15° dorsal tilt and 20° volar tilt), intra-articular step-off (<2 mm) of the radiocarpal joint and articular incongruity (<2 mm of the sigmoid notch of the distal radius) [6–9]. Various combinations and permutations of these indices have been converted into scoring systems [10, 11]. Most of these scoring systems lack clinical sensitivity, however, and are therefore used infrequently [10]. Two exceptions are the anatomical radiological classification for distal radial fractures according to Lidström and the deformity scoring system according to Gartland and Werley [12–14]. The latter contains an objective component, consisting of radiological, clinical and functional assessment, as well as a subjective evaluation [12]. Lidström’s classification evaluates the wrist after a Colles’ fracture and merely consists of the radiological assessment of dorsal angulation, radial length and radial inclination. The restoration of the anatomy of the distal radius is subsequently classified as a poor, fair, good or excellent result based on the aforementioned radiological measurements [13–15].
To assess fracture reduction of the ankle, different radiological evaluation methods are described in the literature. One of these methods is rank order analysis of the congruency, taking into consideration the entire fracture pattern [16]. In some studies different aspects such as anatomical reduction of the tibial articular surface, joint congruency, talar shift, talar tilt or syndesmotic diastasis were subjectively scored from perfect to poor [4, 17, 18]. Avodia et al. developed a classification method which included distance measurements of the malleoli and the tertius fragment, mortise widening, talar tilt and talar displacement [19]. This classification was adjusted by Teeny et al. [20, 21] by assigning points to the different items, generating an overall score.
Evaluation of fracture reduction is confounded by the high interobserver variance, especially in the evaluation of plain radiographs [6, 15, 20, 22]. Grainger et al. [23] showed interobserver agreement was higher for measurements of distances than for measurements of angles. In contrast, Kreder et al. demonstrated a particularly high interobserver variance for distance measurements of intra-articular step and gap. Because available evidence is scarce regarding which parameters of the anatomical reduction and fixation influence clinical outcome and inter-observer measurement variation is high, no internationally accepted criteria exist to judge the quality of fracture reduction and fixation. Currently the radiological evaluation of ankle and wrist fractures is based on the experience of the surgeon and/or radiologist and on their frame of reference. Well-defined criteria are fundamental to attain interobserver agreement and comparability between studies. The aim of this study was to obtain a practice-based consensus on the most important criteria for radiological evaluation of the fracture reduction and fixation of the wrist and ankle in the Netherlands.
Methods
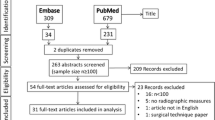
The Delphi method, developed by the Rand Corporation, is considered an effective way to measure and obtain group consensus [24–27]. It is a structured, anonymous and repeated process requiring experts to respond to non-leading, unambiguous statements on items pertinent to the topic [25]. To assess the level of agreement on useful criteria in the radiological evaluation of the ankle and wrist, a list of items was composed based on literature data and on the experience of the surgeons and radiologists. These items were divided into three main topics: (1) imaging technique, (2) evaluation of anatomical aspects of the operated joint, (3) fracture reduction and position of the fixation material.
Invited medical specialists
In the daily routine of many hospitals, different disciplines are involved in the radiological evaluation of ankles and wrists in fracture surgery. In the Netherlands, both trauma and orthopaedic surgeons perform fracture surgery [28]. In order to achieve a broad-based consensus, we approached 225 Dutch medical specialists, including 75 trauma surgeons, 80 orthopaedic surgeons and 70 radiologists. This sample was chosen from surgeons and radiologists working in university hospitals (8) and training and non-training hospitals (12). Because radiologists and surgeons in university hospitals have a super-specialisation, we only approached radiologists from university hospitals that had expertise in skeletal evaluation and surgeons with expertise in open reduction and internal fixation (ORIF) of fractures of the extremities. In the training and non-training hospitals, all radiologists, trauma surgeons and orthopaedic surgeons were invited to participate. The same specialists were invited to participate in the three Delphi rounds.
Delphi procedure
Three Delphi rounds involving an online questionnaire were scheduled. The invitations, consisting of a statement to motivate participation in this study, an explanation of the Delphi procedure and a link to the URL of the online questionnaire, were sent by email. The private e-mail addresses were obtained from most specialists (n = 177). Other emails inviting participation were sent to the secretary of the particular department, who then forwarded the e-mail to the specialists. If the specialist did not reply, up to three reminders were sent every 2 weeks. The complete questionnaires, translated in English, can be found on the internet (online resources 1–3).
The first questionnaire consisted of two parts. The first part contained questions about the ankle, while the second part pertained to the wrist. The questionnaire included both multiple-choice and open questions about the aforementioned criteria. The imaging questions were intended to identify how often the imaging modalities and techniques were used by the respondents in case of a suspected fracture and after fracture surgery. In the open questions the specialists were asked to provide a top-six list of aspects of the joint which, in their opinion, required evaluation. In the remaining open questions, the respondents were given the opportunity to include remarks and suggestions for other criteria. Pictures of the different measurements were added for clarification.
The second questionnaire was constructed using the results of the first questionnaire, incorporating remarks and suggestions. As with the first questionnaire, this was a bipartite questionnaire with one section relating to the ankle and the other relating to the wrist. A histogram presenting the relevant results from the first questionnaire was included in the introduction of each question. Multiple-choice questions were used to ask about imaging techniques, the evaluation of the joint and reduction and fixation. Questions about the evaluation of aspects of the joint anatomy were divided into a main question about the importance of a particular aspect of the joint and a sub-question on how to evaluate this aspect.
The third questionnaire was fuelled by the results of the second questionnaire and consisted of questions on which no consensus was reached yet. These questions were posed in the same manner and same order as the second questionnaire. In the introduction the respondents were urged to reach agreement. If agreement on an item had been reached in the second questionnaire, this was reported and no new, similar question was posed.
Statistical analysis
The number of similar answers was divided by the number of respondents and expressed as a percentage. For the criteria concerning imaging technique and reduction and fixation, consensus was defined as an agreement of at least 90%. For the main evaluation of aspects of the anatomy, consensus was also defined as 90% agreement. Because there are different ways of assessing these aspects, a lower consensus was expected and therefore consensus on the sub-question on how to assess a particular anatomical aspect was defined as an agreement of at least 80%.
Results
Response rate
The first Delphi round started in August 2007. There were 64 respondents (Table 1). The experience as a specialist ranged from 0 years to more than 20 years, spread almost equally across five groups of years of experience (0–5; 5–10; 10–15;15–20; >20 years). As summarized in Table 1, 141 specialists did not respond to the questionnaire, giving no reason for non-participation. Specialists, who replied that they did not want to participate, were removed from our mailing list. Reasons given for not participating were the lack of relevance of the wrist or ankle to their field of interest or lack of time. In the reminders of the first Delphi round we included a small incentive to reply (a dinner cheque was to be raffled), but with little result.
The second round started in January 2008 and the third in May 2008, using the same mailing list as the first round. In these rounds, respectively, 72 and 62 specialists responded to our questionnaire. A total of 42 specialists completed all three questionnaires.
Agreement regarding radiological evaluation of the wrist
An overview of the consensus on radiological evaluation of the wrist is given in Table 2. Posterior-Anterior (PA) radiographs and lateral radiographs are the required imaging techniques for the standard evaluation of the wrist. Consensus on these items was reached already in the second Delphi round. Although the majority of the respondents indicated that an oblique PA-view or a radiograph of the contralateral wrist is not required in the standard evaluation, this majority did not reach the 90% cut-off value. A small majority stated that both preoperative and postoperative CT scans are only required selectively. Reported indications for a preoperative CT scan included the need for greater insight into complicated intra-articular fractures or optimal operation planning. Indications for a postoperative CT scan included uncertainty about the fracture reduction or position of the fixation material.
For the evaluation of the wrist in general, no consensus could be reached on the necessity of measurements when assessing the anatomy of the wrist. The same held true for visual assessment. Consensus was already reached in the second Delphi round for all but one of the proposed evaluation criteria. Consensus could not be reached on the need to assess the relationship between the radius and the (meta)carpal bones, although there was 86% agreement on the importance of this aspect. In terms of the relationship between radial and ulnar length, it is interesting to note that consensus was only reached on the importance of measuring dorsal angulation. For other measurements associated with this criterion, such as ulnar variance, radial length and radial angulation, no consensus was reached. For carpal height ratio, carporadial distance ratio and carpo-ulnar distance there was consensus that these items are not required in the evaluation of the wrist. No consensus could be reached on measurement of the radioulnar distance, ulnar translocation and the scapholunar angle. The respondents indicated that all evaluation criteria could be assessed visually.
In terms of fracture reduction and position of fixation material in the wrist, consensus was only reached in the second Delphi round on the need to evaluate the absence of intra-articular steps, gaps and bone fragments. Only a minority of specialists believed it was necessary to assess the absence of these aspects if it existed extra-articular. Consensus was reached on the importance of evaluating the position of plates and screw length. Unexpectedly, agreement on the evaluation of the bicortical presence of screws dropped from 86% in the second round to 73% in the third Delphi round. Evaluation of the absence of protruding screws and/or K-wires was only considered relevant for intra-articular protrusion. However, no consensus could be reached on how to assess intra-articular protrusion, although 79% of the respondents agreed evaluation could be performed visually.
Agreement regarding radiological evaluation of the ankle
An overview of the consensus is given in Table 3. In terms of the imaging techniques required for standard evaluation of the ankle, consensus was only reached on the standard use of the lateral radiograph (100%). Although the 90% cut-off was not reached for the importance of a mortise view (79%), it was preferred over an AP view, either an AP view or a mortise view, or both. A small majority (65%) preferred not to take radiographs of the contralateral ankle. For both the preoperative and postoperative CT scan, opinions were divided between no CT scans at all and selective CT scans. The indications mentioned here were the same as those given for the wrist.
In contrast with the evaluation of the wrist, there was 86% agreement that the general assessment of the ankle could be performed visually. A majority of the respondents (58%) considered that angle and distance measurements were not relevant to the general assessment. Consensus was already reached in the second Delphi round for all but one of the proposed evaluation criteria, namely the rotation of the talus (only 50% agreement). For the congruency of the joint and the symmetry of the joint space, there was even a consensus of 100%. Measurement of the distance between the tibia and fibula was not considered relevant, nor was the measurement of the talocrural angle to determine the length of the fibula. No consensus could be reached for the need to draw Shentons’ line to determine joint congruency, to perform measurements of the width of the joint space or to measure the overlap of the tibia and fibula on a mortise projection. The respondents felt that all the evaluation criteria could be assessed visually, except for the rotation of the fibula. Although there was consensus on the importance of evaluating the rotation of the fibula, no consensus could be reached on how this should be carried out. Although a 68% majority believed that measurement of the proposed Axial Malleolar Index (AMI) was not necessary for the evaluation of the rotation of the fibula, 61% also stated visual assessment was not sufficient. No further suggestions were given, however, on how to evaluate this aspect.
The results of the evaluation of the fracture reduction and fixation material in the ankle were similar to those in the wrist. The only exception was that for the ankle there was a consensus of 92% on the importance of assessing the bicortical presence of screws and/or K-wires.
Discussion
In the three Delphi rounds, approximately one-third of the specialists responded. This appears to be a low response rate, although the actual number of respondents is considerable compared with other Delphi studies in which a maximum of 55 respondents were reported [25, 29, 30]. Reasons for the low response rate could be the timing of the questionnaire (during the summer holidays); the inability to obtain all private email addresses and the difficulty senior specialists might have with using the internet. When we consider the reasons given for not participating in this consensus, it is unlikely that non-responders would have had significantly different opinions to those of the responders. In fact, those willing to participate have been shown to be representative of other colleagues in terms of qualifications, experience and speciality [31]. Therefore, it can be assumed that the results of this Delphi consensus are representative of radiologists, orthopaedic surgeons and trauma surgeons in the Netherlands.
In this Delphi study, consensus was reached on how to evaluate fracture reduction and fixation of the wrist and the ankle. Consensus on which items not to evaluate was scarce. Although full consensus could not be attained, a high level of agreement was reached as to the evaluation of the anatomy of the wrist and ankle. In the evaluation of fracture reduction, intra-articular aspects were considered important for both the wrist and the ankle. The attained consensus is that fixation should be assessed using three of the five proposed criteria for the wrist and four of the five criteria proposed for the ankle. There was little increase in agreement after the second Delphi round and for some items consensus even decreased after the second Delphi round. This suggests that no further agreement would have been reached if more Delphi rounds would have been conducted.
However, this Delphi study also showed that opinions differ in the imaging techniques that are required in the evaluation of especially the ankle. Consensus was reached for only one out of eight imaging techniques for the ankle. The fact that the threshold of 90% agreement for consensus could not be reached for either an AP- or a mortise projection is remarkable. Although undesirable, it can be due to the fact that in Dutch clinical practice not always a clear distinction is being made between the mortise and AP projection. An AP projection of the ankle in Dutch guidelines is often described with 20° endorotation [32]. Another explanation can possibly be found in a difference between the desired imaging strategy and practical limitations. In clinical practice it is not always possible to have an accurate mortise or AP projection due to the patient’s inability to endorotate because of the injury. In these cases, the injury can usually be properly diagnosed based on the physical exam, even with a suboptimal mortise or AP projection.
For additional imaging like a CT-scan, opinions were ambivalent for both the wrist and the ankle. This may reflect the difference in imaging policy between different hospitals or even between different specialists within a hospital, despite recommendations given by the AO foundation for standard and additional imaging [1]. Our results largely correspond with their recommendations for the standard imaging of the wrist, but not for the ankle.
All items concerning intra-articular fracture reduction and position of the fixation material were incorporated in the final consensus for both the ankle and the wrist. In concordance with the AO recommendations, respondents tended to consider extra-articular fracture reduction and position of the fixation material to be less important, but no consensus could be reached on any of these items [1]. AO recommendations also make little mention of extra-articular fracture reduction other than to emphasise the need to strive for alignment.
Sometimes, conflicting answers arose due to the way in which the questions were phrased. There were questions on how to evaluate the aspects of the wrist or ankle anatomy. Respondents could choose to answer either ‘yes’ or ‘no’, but did not have to choose between the different evaluation methods. For example, in the evaluation of the relationship between the length of the radius and the ulna, respondents indicated that measurement of dorsal angulation was important, but they also reported that it could be assessed visually. In contrast, assessment of rotation of the fibula was considered important, but no consensus could be reached on how this should be evaluated. The majority of the specialists did not think this could be determined visually, nor did they think that it could be determined by measuring the axial malleolar index on a CT scan. In the third Delphi round, the respondents were asked to provide suggestions on how to evaluate the rotation, but none were given. As a result, it was not possible to propose a method to evaluate rotation of the fibula.
Traditionally, the various scoring systems available have been based on radiographic measurements [3, 4, 6–11, 14, 17–19, 22, 33]. This is also true for the AO requirements for an acceptable fracture reduction of the wrist. These requirements are articular incongruity of less than 2 mm, radial shortening of less than 5 mm and residual dorsal tilt of less than 10°. For the ankle, one of the measurements mentioned is that of the talocrural angle [1]. It is interesting to note that in our consensus, with the exception of dorsal tilt measurement, no consensus could be reached on the necessity of most measurements. Moreover, there was actually consensus that some measurements were not necessary when assessing the ankle and wrist. According to this consensus, most of the aspects of the wrist and ankle anatomy can be assessed visually. This view is in marked contrast to the evaluation of the anatomy as described in the literature, but better usable in clinical practice. In addition, our respondents considered more aspects important in the evaluation of the wrist and ankle than the aforementioned scoring systems do. This implies that these scoring systems, either evidence-based or expert-based, do not reflect routine radiological practice in the Netherlands. Therefore, we suggest a more practice-based scoring protocol in which the different items can be evaluated visually. A Delphi study involving international specialists will have to be performed to investigate whether the results of this Dutch Delphi study are also representative for other countries regarding their routine policies and radiological evaluation. Consensus on imaging policy and radiological assessment of the wrist and ankle is important for creating more uniformity in the standard care of fractures of the wrist and ankle, within and between countries.
Conclusion
By means of this Delphi study based on the clinical experience of specialists from different disciplines in the Netherlands, a broad consensus has been reached on how to evaluate wrist and ankle fracture reduction and fixation. In contrast with previous scoring systems, measurements do not take a prominent place in our findings. Therefore, we suggest a more practice-based scoring protocol, based on this consensus, in which the different items can be evaluated visually. This scoring protocol can be used as an educational tool, but can also be used to increase uniformity in the radiological evaluation of the wrist and ankle in clinical practice.
References
Ruedi TP, Buckley RE, Moran CG (2007) AO Principles of Fracture Management, 2nd edn. Thieme Medical Publishers, New York
Catalano LW III, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J Jr (1997) Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am 79(9):1290–1302
Goldfarb CA, Rudzki JR, Catalano LW, Hughes M, Borrelli J Jr (2006) Fifteen-year outcome of displaced intra-articular fractures of the distal radius. J Hand Surg Am 31(4):633–639
Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM (2002) Results of ankle fractures with involvement of the posterior tibial margin. J Trauma 53(1):55–60
Lloyd J, Elsayed S, Hariharan K, Tanaka H (2006) Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int 27(10):793–796
Cole RJ, Bindra RR, Evanoff BA, Gilula LA, Yamaguchi K, Gelberman RH (1997) Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiography versus computed tomography. J Hand Surg Am 22(5):792–800
Goldfarb CA, Yin Y, Gilula LA, Fisher AJ, Boyer MI (2001) Wrist fractures: what the clinician wants to know. Radiology 219(1):11–28
Knirk JL, Jupiter JB (1986) Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 68(5):647–659
Mann FA, Wilson AJ, Gilula LA (1992) Radiographic evaluation of the wrist: what does the hand surgeon want to know? Radiology 184(1):15–24
Jaremko JL, Lambert RG, Rowe BH, Johnson JA, Majumdar SR (2007) Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol 62(1):65–72
Jeong GK, Kaplan FT, Liporace F, Paksima N, Koval KJ (2004) An evaluation of two scoring systems to predict instability in fractures of the distal radius. J Trauma 57(5):1043–1047
Gartland JJ Jr, Werley CW (1951) Evaluation of healed Colles’ fractures. J Bone Joint Surg Am 33-A(4):895–907
Lidstrom A (1955) Typical radius fracture. Nord Med 54(43):1621–1625
Sarmiento A, Pratt GW, Berry NC, Sinclair WF (1975) Colles’ fractures. Functional bracing in supination. J Bone Joint Surg Am 57(3):311–317
van Eerten PV, Lindeboom R, Oosterkamp AE, Goslings JC (2008) An X-ray template assessment for distal radial fractures. Arch Orthop Trauma Surg 128(2):217–221
DeCoster TA, Willis MC, Marsh JL, Williams TM, Nepola JV, Dirschl DR et al (1999) Rank order analysis of tibial plafond fractures: does injury or reduction predict outcome? Foot Ankle Int 20(1):44–49
Jaskulka RA, Ittner G, Schedl R (1989) Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma 29(11):1565–1570
Musgrave DJ, Fankhauser RA (1998) Intraoperative radiographic assessment of ankle fractures. Clin Orthop Relat Res 351:186–190
Ovadia DN, Beals RK (1986) Fractures of the tibial plafond. J Bone Joint Surg Am 68(4):543–551
Grose A, Gardner MJ, Hettrich C, Fishman F, Lorich DG, Asprinio DE et al (2007) Open reduction and internal fixation of tibial pilon fractures using a lateral approach. J Orthop Trauma 21(8):530–537
Teeny SM, Wiss DA (1993) Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res 292:108–117
Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF (1996) X-ray film measurements for healed distal radius fractures. J Hand Surg Am 21(1):31–39
Grainger AJ, Duryea J, Elliott JM, Genant HK (2002) The evaluation of a new digital semi-automated system for the radiological assessment of distal radial fractures. Skeletal Radiol 31(8):457–463
Brown B (1968) Delphi process: A methodology used for the elicitation of opinions of experts. www.rand.org; Report No.: P-3925
Holey EA, Feeley JL, Dixon J, Whittaker VJ (2007) An exploration of the use of simple statistics to measure consensus and stability in Delphi studies. BMC Med Res Methodol 7:52
Huisstede BM, Miedema HS, Verhagen AP, Koes BW, Verhaar JA (2007) Multidisciplinary consensus on the terminology and classification of complaints of the arm, neck and/or shoulder. Occup Environ Med 64(5):313–319
Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J et al (1998) Consensus development methods, and their use in clinical guideline development. Health Technol Assess 2(3):i–i88
Goslings JC, Ponsen KJ, Luitse JS, Jurkovich GJ (2006) Trauma surgery in the era of nonoperative management: the Dutch model. J Trauma 61(1):111–114
Almansa C, Rey E, Bolanos E, Palma M, Alvarez SA, az-Rubio M (2007) Spanish physicians point of view on irritable bowel syndrome (IBS). Results of a Delphi survey. Rev Esp Enferm Dig 99(4):210–217
Bakx R, Emous M, Legemate DA, Machado M, Zoetmulder FA, van Tets WF et al (2006) Categorization of major and minor complications in the treatment of patients with resectable rectal cancer using short-term pre-operative radiotherapy and total mesorectal excision: a Delphi round. Colorectal Dis 8(4):302–308
McKee M, Priest P, Ginzler M, Black N (1991) How representative are members of expert panels? Qual Assur Health Care 3(2):89–94
Brink P, Mourik Jv, Öner F, Simmermacher R, Verheyen C, Werken Cvd (2007) Letsels van de enkel en de voet. Letsels van het steun- en bewegingsapparaat. Elsevier Gezondheidszorg, Maarssen, pp 261–266
Schneiders W, Biewener A, Rammelt S, Rein S, Zwipp H, Amlang M (2006) Distal radius fracture. Correlation between radiological and functional results. Unfallchirurg 109(10):837–844
Acknowledgments
The authors thank the following participants in the Delphi study for their contribution in obtaining this consensus (in alphabetical order):
K.A. Bartlema, MD
L.F.M. Beenen, MD PhD
G.I.J.M. Beerthuizen, MD PhD
M. Bemelman, MD
B.P. Bertelink, MD
J.H.J.M. Bessems, MD
A.F.A. van Beurden, MD
J. Biert, MD PhD
F.W. Bloemers, MD PhD
A.L. Boerboom, MD
P.H. Breedveld, MD
M.W.G.A. Bronkhorst, MD
G. Bronsema, MD
R.W. Brouwer, MD PhD
S.K. Bulstra, MD PhD
L.A. Burghard, MD
A. Dalen, MD
R.L. Diercks, MD PhD
B.A. van Dijkman, MD
H.A.J. Dijkstra, MD
R.A. Droog, MD PhD
C. van Egmond, MD
L.H.G.J. Elmans, MD
C. Faber, MD
M.L.M. Falke, MD
A.J. Frima, MD
J.P. Frölke, MD PhD
A.Z. Ginai, MD PhD
J.W.H. Gabriëls, MD
J.C. Goslings, MD PhD
W. Haagh, MD
B.L.E.F. ten Have, MD
J.S. Harbers, MD
R. Haverlag, MD
W.H.J.C. van Heeswijk, MD
H.J.L van der Heide, MD PhD
M.P. Heijboer, MD
S.H. van Helden, MD PhD
W.R. Hogeboom, MD PhD
M. Holla, MD
B. Huisman, MD PhD
P.F.J. Houben, MD
P.F. Hulstaert, MD
I.M.C. Jansen, MD
J.M.G.T. Jenner, MD PhD
Th.E.A.M. de Jong, MD
M.C. de Jonge, MD
A.J.M. Karthaus, MD PhD
R.P. Karthaus, MD
P. Kloen, MD PhD
K.A. Kolkman, MD
E. Krug, MD
P.H.W. Lubbert, MD PhD
P.A. van Luijt, MD
M. Maas, MD PhD
P.G.M. Maathuis, MD PhD
A.K. Mostert, MD PhD
H. Mul, MD
H.J. Oostenbroek, MD
P.P. Oprel, MD
P. Patka, MD PhD
K.J. Ponsen, MD PhD
S. Ploem, MD
P.A.M. Raaijmakers, MD
H. Rath, MD
S.J. Rhemrev, MD
M.G. Romijn, MD
G.R. Schaap, MD PhD
M.U. Schafroth, MD PhD
I.B. Schippers, MD PhD
R.K.J. Simmermacher, MD PhD
W. van der Stappen, MD
E. Tan, MD PhD
J.L. Turkenburg, MD PhD
A. van der Veen, MD PhD
B. Veenings, MD
J.P.A.M. Verbruggen, MD PhD
C.C.P.M. Verheyen, MD PhD
M.H.J. Verhofstad, MD PhD
E.J.J.M. Verleisdonk, MD PhD
L.M.M. Vogels, MD
A.B. van Vugt, MD
M. Waleboer, MD
A.D.P. van Walsum, MD PhD
R. Weijers, MD PhD
K.W. Wendt, MD PhD
M.M.E.H. Witbreuk, MD
C.A.J. van der Worp, MD
Conflict of interest
All authors declare to have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Beerekamp, M.S., Haverlag, R., Ubbink, D.T. et al. How to evaluate the quality of fracture reduction and fixation of the wrist and ankle in clinical practice: a Delphi consensus. Arch Orthop Trauma Surg 131, 739–746 (2011). https://doi.org/10.1007/s00402-010-1198-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1198-9