Abstract
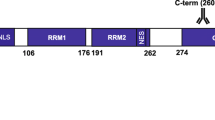
Alzheimer’s disease (AD) manifests with progressive memory loss and decline of spatial awareness and motor skills. Neurofibrillary tangles (NFTs) represent one of the pathological hallmarks of AD. Previous studies suggest that the enzyme prolyl-peptidyl cis–trans isomerase PIN1 [protein interacting with NIMA (never in mitosis A)-1] recognizes hyperphosphorylated tau (in NFTs) and facilitates its dephosphorylation, thereby recovering its function. This study aims to determine the frequency, severity and distribution of PIN1 immunoreactivity and its relationship to NFTs and other neuropathological markers of neurodegeneration such as amyloid-β (Aβ) plaques and transcription-responsive DNA-binding protein of M r 43 kDa (TDP-43). Immunohistochemical analysis of 194 patients (46 with AD, 43 with Parkinson’s disease/dementia with Lewy bodies, 12 with progressive supranuclear palsy/corticobasal degeneration, 36 with frontotemporal lobar degeneration, 21 with motor neuron disease and 34 non-demented (ND) individuals) revealed an increased frequency and severity of PIN1 immunoreactive inclusions in AD as compared to all diagnostic groups (P < 0.001). The hippocampal and cortical distribution of PIN1 granules was distinct from that of NFTs, Aβ and TDP-43 pathologies, though the frequency of neurons with PIN1 immunoreactivity increased with increasing NFT pathology. There was a progressive increase in PIN1 changes in ND individuals as the degree of AD-type pathological changes increased. Present findings indicate that PIN1 changes are a constant feature of AD pathology and could serve as a biomarker of the onset or spread of AD neuropathology independent of tau or Aβ.









Similar content being viewed by others
References
Alonso AC, Grundke-Iqbal I, Iqbal K (1996) Alzheimer’s disease hyperphosphorylated tau sequesters normal tau into tangles of filaments and disassembles microtubules. Nat Med 2:783–787
Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, Mann D, Tsuchiya K, Yoshida M, Hashizume Y, Oda T (2006) TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun 351:602–611
Arriagada PV, Growdon JH, Hedley-Whyte ET, Hyman BT (1992) Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. J Neuropathol Exp Neurol 42:631–639
Balastik M, Lim JL, Pastorino L, Lu KP (2007) Pin1 in Alzheimer’s disease: multiple substrates, one regulatory mechanism? BBA-Mol Basis Dis 1772:422–429
Ball MJ (1978) Topographic distribution of neurofibrillary tangles and granulovacuolar degeneration in hippocampal cortex of ageing and demented patients. A quantitative study. Acta Neuropathol 42:73–80
Bancher C, Brunner C, Lassmann H, Budka H, Jellinger K, Wiche G, Seitelberger F, Grundke-Iqbal I, Iqbal K, Wisniewski H (1989) Accumulation of abnormally phosphorylated τ precedes the formation of neurofibrillary tangles in Alzheimer’s disease. Brain Res 477:90–99
Blom ES, Giedraitis V, Zetterberg H, Fukumoto H, Blennow K, Hyman BT, Irizarry MC, Wahlund LO, Lannfelt L, Ingelsson M (2009) Rapid progression from mild cognitive impairment to Alzheimer’s disease in subjects with elevated levels of tau in cerebrospinal fluid and the APOE epsilon4/epsilon4 genotype. Dement Geriatr Cogn Disord 27:458–464
Bullock R (2004) Future directions in the treatment of Alzheimer’s disease. Expert Opin Investig Drugs 13:303–314
Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Del Tredici K (2006) Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol 112:389–404
Castellani RJ, Gupta Y, Siedlak SL, Harris PLR, Coller JM, Perry G, Zhu X, Tabaton M, Smith MA (2010) Granulovacuolar degeneration in aging and Alzheimer’s disease are the human homologue of stress granules precipitated by oxidative injury
Cleveland DW, Hwo SY, Kirschner MW (1977) Purification of tau, a microtubule-associated protein that induces assembly of microtubules from purified tubulin. J Mol Biol 116:207–225
Davidson Y, Amin H, Kelley T, Shi J, Tian J, Kumaran R, Lashley T, Lees AJ, DuPlessis D, Neary D, Snowden JS, Sikkink S, Pickering-Brown SM, Mann DMA (2009) TDP-43 in ubiquitinated inclusions in the inferior olives in frontotemporal lobar degeneration and in other neurodegenerative diseases: a degenerative process distinct from normal ageing. Acta Neuropathol 118:359–369
Davidson Y, Kelley T, Mackenzie IRA, Pickering-Brown SM, Du Plessis D, Neary D, Snowden JS, Mann DMA (2007) Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol 113:521–533
De Estable-Puig RF, De Estable-Puig JF (1975) Vacuolar degeneration in neurons of aging rats. Virchows Arch B Cell Path 17:337–346
Dickson DW, Liu WK, Kress Y, Ku J, DeJesus O, Yen SH (1993) Phosphorylated tau immunoreactivity of granulovacuolar bodies (GVB) of Alzheimer’s disease: localization of two amino terminal tau epitopes in GVB. Acta Neuropathol 85:463–470
Fagan AM, Mintun MA, Mach RH, Lee SY, Dence CS, Shah AR, LaRossa GN, Spinner ML, Klunk WE, Mathis CA (2006) Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Aβ42 in humans. Ann Neurol 59:512–519
Forsberg A, Engler H, Almkvist O, Blomquist G, Hagman G, Wall A, Ringheim A, Långström B, Nordberg A (2008) PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol Aging 29:1456–1465
Gendron TF, Petrucelli L (2009) The role of tau in neurodegeneration. Mol Neurodegener 4:13–29
Gotz J, Chen F, Barmettler R, Nitsch RM (2001) Tau filament formation in transgenic mice expressing P301L tau. J Biol Chem 276:529–534
Hashemzadeh-Bonehi L, Phillips RG, Cairns NJ, Mosaheb S, Thorpe JR (2006) Pin1 protein associates with neuronal lipofuscin: potential consequences in age-related neurodegeneration. Exp Neurol 199:328–338
Hendrie HC (1998) Epidemiology of dementia and Alzheimer’s disease. Amer J Geriatr Psychiatr 6:19–21
Hirano A, Dembitzer HM, Kurland LT, Zimmerman HM (1968) The fine structure of some intraganglionic alterations. Neurofibrillary tangles, granular vacuolar bodies and ‘rod-like’ structures as seen in Guam amyotrophic lateral sclerosis and parkinsonism dementia complex. J Neuropathol Exp Neurol 27:169–182
Holzer M, Gärtner U, Stöbe A, Härtig W, Gruschka H, Brückner MK, Arendt T (2002) Inverse association of Pin1 and tau accumulation in Alzheimer’s disease hippocampus. Acta Neuropathol 104:471–481
Khatoon S, Grundke-Iqbal I, Iqbal K (1992) Brain levels of microtubule-associated protein tau are elevated in Alzheimer’s disease: a radioimmuno-slot-blot assay for nanograms of the protein. J Neurochem 59:750–753
Landau S, Harvey D, Madison C, Reiman E, Foster N, Aisen P, Petersen R, Shaw L, Trojanowski J, Jack C Jr, Weiner MW, Jagust WJ (2010) Comparing predictors of conversion and decline in mild cognitive impairment. Neurology 75:230–238
Lewis J, McGowan E, Rockwood J, Melrose H, Nacharaju P, Van Slegtenhorst M, Gwinn-Hardy K, Murphy MP, Baker M, Yu X (2000) Neurofibrillary tangles, amyotrophy and progressive motor disturbance in mice expressing mutant (P301L) tau protein. Nat Genet 25:402–405
Lim J, Ping Lu K (2005) Pinning down phosphorylated tau and tauopathies. BBA-Mol Basis Dis 1739:311–322
Liou YC, Sun A, Ryo A, Zhou XZ, Yu ZX, Huang HK, Uchida T, Bronson R, Bing G, Li X (2003) Role of the prolyl isomerase Pin1 in protecting against age-dependent neurodegeneration. Nature 424:556–561
Lu KP, Zhou XZ (2007) The prolyl isomerase PIN1: a pivotal new twist in phosphorylation signalling and disease. Nat Rev Mol Cell Biol 8:904–916
Lu PJ, Wulf G, Zhou XZ, Davies P, Lu KP (1999) The prolyl isomerase Pin1 restores the function of Alzheimer-associated phosphorylated tau protein. Nature 399:784–788
Maddalena A, Papassotiropoulos A, Muller-Tillmanns B, Jung HH, Hegi T, Nitsch RM, Hock C (2003) Biochemical diagnosis of Alzheimer disease by measuring the cerebrospinal fluid ratio of phosphorylated tau protein to {beta}-amyloid peptide42. Arch Neurol 60:1202–1206
Mackenzie IRA, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, Kovacs GG, Ghetti B, Halliday G, Holm IE, Ince PG, Kamphourst W, Revesz T, Rozemuller AJM, Kumar-Singh S, Akiyama H, Baborie A, Spins S, Dickson DW, Trojanowski JQ, Mann DMA (2009) Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: consensus recommendations. Acta Neuropathol 117:15–18
Mackenzie IRA, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, Kovacs GG, Ghetti B, Halliday G, Holm IE, Ince PG, Kamphourst W, Revesz T, Rozemuller AJM, Kumar-Singh S, Akiyama H, Baborie A, Spins S, Dickson DW, Trojanowski JQ, Mann DMA (2010) Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol 119:1–4
Mann DM (1978) Granulovacuolar degeneration in pyramidal cells of the hippocampus. Acta Neuropathol 42:149–151
McKhann GM, Albert MS, Grossman M, Miller B, Dickson D, Trojanowski JQ (2001) Clinical and pathological diagnosis of frontotemporal dementia: report of the Work Group on Frontotemporal Dementia and Pick’s Disease. Arch Neurol 58:1803–1809
Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, Bruce J, Schuck T, Grossman M, Clark CM (2006) Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314:130–133
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, Freedman M, Kertesz A, Robert PH, Albert M (1998) Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 51:1546–1554
Piao YS, Wakabayashi K, Kakita A, Yamada M, Hayashi S, Morita T, Ikuta F, Oyanagi K, Takahashi H (2003) Neuropathology with clinical correlations of sporadic amyotrophic lateral sclerosis: 102 autopsy cases examined between 1962 and 2000. Brain Pathol 13:10–22
Price J, Davis P, Morris J, White D (1991) The distribution of plaques, tangles and related immunohistochemical markers in healthy aging and Alzheimer’s disease. Neurobiol Aging 12:295–312
Ramakrishnan P, Dickson DW, Davies P (2003) Pin1 colocalization with phosphorylated tau in Alzheimer’s disease and other tauopathies. Neurobiol Dis 14:251–264
Reynolds CH, Garwood CJ, Wray S, Price C, Kellie S, Perera T, Zvelebil M, Yang A, Sheppard PW, Varndell IM (2008) Phosphorylation regulates tau interactions with Src homology 3 domains of phosphatidylinositol 3-kinase, phospholipase C gamma 1, Grb2, and Src family kinases. J Biol Chem 283:18177–18186
Rocca W, Bonaiuto S, Lippi A, Luciani P, Turtu F, Cavarzeran F, Amaducci L (1990) Prevalence of clinically diagnosed Alzheimer’s disease and other dementing disorders: a door-to-door survey in Appignano, Macerata Province, Italy. Neurology 40:626–631
Shi J, Shaw CL, Richardson AMT, Bailey K, Tian J, Varma AR, Neary D, Snowden JS, Mann DMA (2005) Histopathological changes underlying frontotemporal lobar degeneration with clinicopathological correlation. Acta Neuropathol 110:501–512
Tomlinson BE, Kitchener D (1971) Granulovacuolar degeneration of hippocampal pyramidal cells. J Pathol 106:165–185
Tapiola T, Alafuzoff I, Herukka SK, Parkkinen L, Hartikainen P, Soininen H, Pirttila T (2009) Cerebrospinal fluid {beta}-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol 66:382–389
Vincent I, Zheng JH, Dickson DW, Kress Y, Davies P (1998) Mitotic phosphoepitopes precede paired helical filaments in Alzheimer’s disease. Neurobiol Aging 19:287–296
Wallin AK, Hansson O, Blennow K, Londos E, Minthon L (2009) Can CSF biomarkers or pre-treatment progression rate predict response to cholinesterase inhibitor treatment in Alzheimer’s disease? Int J Geriatr Psychiatry 24:638–647
Acknowledgments
We wish to thank the Academic Cultural Office of Kuwait, London, and the Ministry of Higher Education, Kuwait, who kindly provided grant support for this work. We thank The UK Parkinson’s Disease Society Tissue Bank, the Thomas Willis Brain Bank, Oxford and Dr Eileen H Bigio (Northwestern Alzheimer Disease Center, AG13854, Northwestern University, Chicago, USA) who kindly provided some of the tissue samples employed in this study. We acknowledge the Alzheimer’s Research Trust and Alzheimer’s Society through the Brains for Dementia Research Initiative for supporting the work of the Manchester and Oxford Brain Banks. MME received financial support from the National Institute for Health Research (NIHR) via the Oxford Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dakson, A., Yokota, O., Esiri, M. et al. Granular expression of prolyl-peptidyl isomerase PIN1 is a constant and specific feature of Alzheimer’s disease pathology and is independent of tau, Aβ and TDP-43 pathology. Acta Neuropathol 121, 635–649 (2011). https://doi.org/10.1007/s00401-011-0798-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-011-0798-y