Abstract
Purpose
Processed meat intake may adversely affect lung health, but data on asthma remains sparse. The magnitude of the processed meat–asthma association may also depend on other unhealthy behaviors. We investigated the association between processed meat intake and the asthma symptom score, and the combined role of unhealthy weight, smoking, low diet quality, and high processed meat intake on the asthma score.
Methods
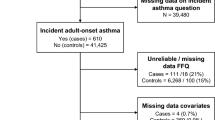
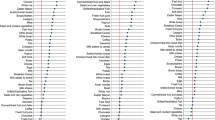
In 2017, 35,380 participants to the NutriNet-Santé cohort answered a detailed respiratory web-questionnaire. Asthma was defined by the asthma symptom score (sum of 5 questions; continuous variable). Based on repeated 24-h dietary records collected on a dedicated website, processed meat consumption was classified as 0, < 2, 2–5, > 5 servings/week. We examined the combined role of body mass index (BMI) (< 25 vs. ≥ 25 kg/m2), smoking (never vs. ever), diet quality score (highest vs. lowest), and processed meat (≤ 5 vs. > 5 servings/week) on the asthma symptom score.
Results
Participants were aged 54 on average (women: 75%, smokers: 49%, BMI ≥ 25: 32%, ≥ 1 asthma symptoms: 27%). After adjustment for confounders, processed meat intake was positively and significantly associated with asthma symptom score: odds ratios (ORs) (95% CI) for > 5 vs. 0 servings/week were 1.15 (1.04–1.27) in women; 1.23 (1.01–1.50) in men. Compared to participants with 0 unhealthy behaviors, ORs for the asthma symptom score among participants with the 4 combined unhealthy behaviors were 2.18 (1.91–2.48) in women; 2.70 (2.10–3.45) in men.
Conclusion
High processed meat consumption was associated with higher asthma symptoms, and combining overweight/obesity, smoking, low diet quality, with high processed meat intake was strongly associated with asthma symptoms.
Similar content being viewed by others
References
IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2018) Red Meat and Processed Meat. International Agency for Research on Cancer, Lyon (FR)
Larsson SC, Orsini N (2014) Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol 179:282–289. https://doi.org/10.1093/aje/kwt261
Micha R, Michas G, Mozaffarian D (2012) Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—an updated review of the evidence. Curr Atheroscler Rep 14:515–524. https://doi.org/10.1007/s11883-012-0282-8
Kaluza J, Wolk A, Larsson SC (2012) Red meat consumption and risk of stroke: a meta-analysis of prospective studies. Stroke 43:2556–2560. https://doi.org/10.1161/STROKEAHA.112.663286
Lippi G, Mattiuzzi C, Cervellin G (2016) Meat consumption and cancer risk: a critical review of published meta-analyses. Crit Rev Oncol Hematol 97:1–14. https://doi.org/10.1016/j.critrevonc.2015.11.008
Okubo H, Shaheen SO, Ntani G et al (2014) Processed meat consumption and lung function: modification by antioxidants and smoking. Eur Respir J 43:972–982. https://doi.org/10.1183/09031936.00109513
Varraso R, Jiang R, Barr RG et al (2007) Prospective study of cured meats consumption and risk of chronic obstructive pulmonary disease in men. Am J Epidemiol 166:1438–1445. https://doi.org/10.1093/aje/kwm235
Jiang R, Camargo CA, Varraso R et al (2008) Consumption of cured meats and prospective risk of chronic obstructive pulmonary disease in women. Am J Clin Nutr 87:1002–1008
Kaluza J, Harris H, Linden A, Wolk A (2018) Long-term unprocessed and processed red meat consumption and risk of chronic obstructive pulmonary disease: a prospective cohort study of women. Eur J Nutr. https://doi.org/10.1007/s00394-018-1658-5
Kaluza J, Larsson SC, Linden A, Wolk A (2016) Consumption of unprocessed and processed red meat and the risk of chronic obstructive pulmonary disease: a prospective cohort study of men. Am J Epidemiol 184:829–836. https://doi.org/10.1093/aje/kww101
Li Z, Rava M, Bédard A et al (2017) Cured meat intake is associated with worsening asthma symptoms. Thorax 72:206–212. https://doi.org/10.1136/thoraxjnl-2016-208375
Pekkanen J (2005) Operational definitions of asthma in studies on its aetiology. Eur Respir J 26:28–35. https://doi.org/10.1183/09031936.05.00120104
Sunyer J, Pekkanen J, Garcia-Esteban R et al (2007) Asthma score: predictive ability and risk factors. Allergy 62:142–148. https://doi.org/10.1111/j.1398-9995.2006.01184.x
Sugiura H, Ichinose M (2011) Nitrative stress in inflammatory lung diseases. Nitric Oxide Biol Chem 25:138–144. https://doi.org/10.1016/j.niox.2011.03.079
Ma J, Xiao L (2013) Association of general and central obesity and atopic and nonatopic asthma in US adults. J Asthma Off J Assoc Care Asthma 50:395–402. https://doi.org/10.3109/02770903.2013.770014
Accordini S, Janson C, Svanes C, Jarvis D (2012) The role of smoking in allergy and asthma: lessons from the ECRHS. Curr Allergy Asthma Rep 12:185–191. https://doi.org/10.1007/s11882-012-0260-9
Garcia-Larsen V, Del Giacco SR, Moreira A et al (2016) Asthma and dietary intake: an overview of systematic reviews. Allergy 71:433–442. https://doi.org/10.1111/all.12800
Li Z, Kesse-Guyot E, Dumas O et al (2017) Longitudinal study of diet quality and change in asthma symptoms in adults, according to smoking status. Br J Nutr 117:562–571. https://doi.org/10.1017/S0007114517000368
Han Y-Y, Forno E, Shivappa N et al (2018) The dietary inflammatory index and current wheeze among children and adults in the United States. J Allergy Clin Immunol Pract 6:834–841.e2. https://doi.org/10.1016/j.jaip.2017.12.029
Andrianasolo RM, Kesse-Guyot E, Adjibade M et al (2018) Associations between dietary scores with asthma symptoms and asthma control in adults. Eur Respir J. https://doi.org/10.1183/13993003.02572-2017
Hercberg S, Castetbon K, Czernichow S et al (2010) The Nutrinet-Santé Study: a web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 10:242. https://doi.org/10.1186/1471-2458-10-242
Lassale C, Castetbon K, Laporte F et al (2015) Validation of a Web-based, self-administered, non-consecutive-day dietary record tool against urinary biomarkers. Br J Nutr 113:953–962. https://doi.org/10.1017/S0007114515000057
Lassale C, Castetbon K, Laporte F et al (2016) Correlations between fruit, vegetables, fish, vitamins, and fatty acids estimated by web-based nonconsecutive dietary records and respective biomarkers of nutritional status. J Acad Nutr Diet 116:427–438.e5. https://doi.org/10.1016/j.jand.2015.09.017
Le Moullec N, Deheeger M, Preziosi P et al (1996) Validation of the photo manual used for the collection of dietary data in the SU.VI.MAX. study 31:158–164
Nutrinet-Santé Etude (2013) Table de composition des aliments de l’étude Nutrinet-Santé (Nutrinet-Santé Study Food Composition Database). Economica, Paris. ISBN 978-2-7178-6537-0
Chiuve SE, Fung TT, Rimm EB et al (2012) Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 142:1009–1018. https://doi.org/10.3945/jn.111.157222
Burney PG, Luczynska C, Chinn S, Jarvis D (1994) The European community respiratory health survey. Eur Respir J 7:954–960
Kauffmann F, Dizier MH, Pin I et al (1997) Epidemiological study of the genetics and environment of asthma, bronchial hyperresponsiveness, and atopy: phenotype issues. Am J Respir Crit Care Med 156:S123–S129. https://doi.org/10.1164/ajrccm.156.4.12tac9
Rage E, Siroux V, Künzli N et al (2009) Air pollution and asthma severity in adults. Occup Environ Med 66:182–188. https://doi.org/10.1136/oem.2007.038349
Jacquemin B, Sunyer J, Forsberg B et al (2009) Association between modelled traffic-related air pollution and asthma score in the ECRHS. Eur Respir J 34:834–842. https://doi.org/10.1183/09031936.00138208
Cerveri I, Cazzoletti L, Corsico AG et al (2012) The impact of cigarette smoking on asthma: a population-based international cohort study. Int Arch Allergy Immunol 158:175–183. https://doi.org/10.1159/000330900
Vizcaya D, Mirabelli MC, Antó J-M et al (2011) A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup Environ Med 68:914–919. https://doi.org/10.1136/oem.2010.063271
Lassale C, Péneau S, Touvier M et al (2013) Validity of web-based self-reported weight and height: results of the Nutrinet-Santé study. J Med Internet Res 15:e152. https://doi.org/10.2196/jmir.2575
(2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i–xii, 1–253
Hagströmer M, Oja P, Sjöström M (2006) The international physical activity questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr 9:755–762
Black AE (2000) Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord J Int Assoc Study Obes 24:1119–1130
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39(Suppl 1):5–41
Yuan YC (2000) Multiple imputation for missing data: concepts and new development. In: Proceedings of the twenty-fifth annual SAS users group international conference, SAS Institute, Cary NC, pp 267–25
Ricciardolo FLM, Di Stefano A, Sabatini F, Folkerts G (2006) Reactive nitrogen species in the respiratory tract. Eur J Pharmacol 533:240–252. https://doi.org/10.1016/j.ejphar.2005.12.057
Vlassara H, Cai W, Goodman S et al (2009) Protection against loss of innate defenses in adulthood by low advanced glycation end products (AGE) intake: role of the antiinflammatory AGE receptor-1. J Clin Endocrinol Metab 94:4483–4491. https://doi.org/10.1210/jc.2009-0089
Zhang W-C, Zheng X-J, Du L-J et al (2015) High salt primes a specific activation state of macrophages, M(Na). Cell Res 25:893–910. https://doi.org/10.1038/cr.2015.87
Ley SH, Sun Q, Willett WC et al (2014) Associations between red meat intake and biomarkers of inflammation and glucose metabolism in women. Am J Clin Nutr 99:352–360. https://doi.org/10.3945/ajcn.113.075663
Lv J, Yu C, Guo Y et al (2017) Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J Am Coll Cardiol 69:1116–1125. https://doi.org/10.1016/j.jacc.2016.11.076
Aleksandrova K, Pischon T, Jenab M et al (2014) Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med 12:168. https://doi.org/10.1186/s12916-014-0168-4
Grosso G, Micek A, Godos J et al (2017) Health risk factors associated with meat, fruit and vegetable consumption in cohort studies: a comprehensive meta-analysis. PLoS One 12:e0183787. https://doi.org/10.1371/journal.pone.0183787
McAloney K, Graham H, Law C, Platt L (2013) A scoping review of statistical approaches to the analysis of multiple health-related behaviours. Prev Med 56:365–371. https://doi.org/10.1016/j.ypmed.2013.03.002
Haut Conseil de la Santé Publique (2017) Statement related to the revision of the 2017–2021 French Nutrition and Health Programme’s dietary guidelines for adults. HCSP Paris 2017
Acknowledgements
The authors thank Younes Esseddik, Thi Hong Van Duong, Paul Flanzy, Régis Gatibelza and Jagatjit Mohinder (computer scientists), Cédric Agaesse (dietitian), Julien Allègre, Nathalie Arnault, Laurent Bourhis and Fabien Szabo de Edelenyi, PhD (data-manager/biostatisticians), Fatoumata Diallo, MD (Physician) for their technical contribution to the NutriNet-Santé study. We thank all the volunteers of the NutriNet-Santé cohort.
Funding
The NutriNet-Santé Study was supported by the following public institutions: Ministère de la Santé, Santé Publique France, Institut National de la Santé et de la Recherche Médicale, Institut National de la Recherche Agronomique, Conservatoire National des Arts et Métiers and Université Paris 13. RMA was supported by a doctoral fellowship from the Ecole Doctorale Galilée, Paris 13 University, Sorbonne Paris Cité.
Author information
Authors and Affiliations
Contributions
RMA, PG and RV designed and conducted the research; SH, MT, NDP, AM, EKG, PG and RV provided essential reagents or provided essential materials; RMA and RV analysed data or performed statistical analysis; RMA, PG and RV wrote the manuscript and had primary responsibility for final content; RMA, SH, MT, NDP, MA, EKG, PG and RV were involved in interpreting the results and editing the manuscript for important intellectual content; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Andrianasolo, R.M., Hercberg, S., Touvier, M. et al. Association between processed meat intake and asthma symptoms in the French NutriNet-Santé cohort. Eur J Nutr 59, 1553–1562 (2020). https://doi.org/10.1007/s00394-019-02011-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-02011-7