Abstract
Background
Recent data has suggested that primary anastomosis (PA), with or without a diverting loop ileostomy (DLI), is a safe option for the treatment of acute complicated diverticulitis. This study aimed to evaluate risk factors associated with anastomotic leak in patients who underwent a sigmoid colectomy with PA and to determine whether a DLI was protective against a clinically significant anastomotic leak.
Methods
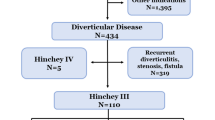
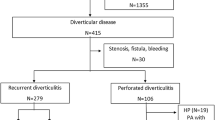
Patients with acute complicated diverticulitis who underwent a laparoscopic or open sigmoid colectomy with PA, with or without a DLI, were identified in the NSQIP PUF(2016–2017). The rates of anastomotic leak, receipt of DLI, and type of leak management were compared. Multivariate logistic regression was performed.
Results
There were 497 patients identified. Seventy-nine(15.9%) patients had a DLI, while 418 (84.1%) did not. Twenty-six anastomotic leaks were identified (5.2%). On multivariate analysis, current smoking (OR 4.02; 95% CI 1.44–11.26) and chronic steroid use (OR 3.84; 95% CI 1.16–12.69) were significantly associated with an increased risk of leak. Of the 26 patients with anastomotic leaks, 5 (19.2%) had a DLI. There was no significant difference in the rate of leak between those with a DLI(5; 6.3%) and those without(21; 5.3%; p = 0.59). Patients who had a DLI were significantly less likely to experience an anastomotic leak requiring re-operation (p < 0.01).
Conclusions
Regardless of the presence of a DLI, chronic steroid use and smoking are associated with an increased risk of anastomotic leak in patients with acute complicated diverticulitis undergoing colectomy with PA. The presence of a diverting loop ileostomy is protective against re-operation.


Similar content being viewed by others
References
Lee JM, Bai P, Chang J, El Hechi M et al (2019) Hartmann's procedure vs primary anastomosis with diverting loop ileostomy for acute diverticulitis: nationwide analysis of 2,729 emergency surgery patients. J Am Coll Surg 229:48
Salem L, Flum DR (2004) Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum 47(11):1953–1964
Bridoux V (2017) Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial. JACS (J Am College Surg) 225(6):798–805
Lambrichts DPV, Vennix S, Musters GD et al (2019) Hartmann’s procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol 4(8):599–610. https://doi.org/10.1016/S2468-1253(19)30174-8
Gachabayov M, Oberkofler CE, Tuech JJ, Hahnloser D, Bergamaschi R (2018) Resection with primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a systematic review and meta-analysis. Colorectal Dis 20(9):753–770. https://doi.org/10.1111/codi.14237
Cirocchi R, Afshar S, Shaban F et al (2018) Perforated sigmoid diverticulitis: Hartmann’s procedure or resection with primary anastomosis-a systematic review and meta-analysis of randomised control trials. Tech Coloproctol 22(10):743–753. https://doi.org/10.1007/s10151-018-1819-9
Hall J, Hardiman K, Lee S et al (2020) The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum 63:728–747. https://doi.org/10.1097/DCR.0000000000001679
Nikolian VC, Kamdar NS, Regenbogen SE et al (2017) Anastomotic leak after colorectal resection: a population-based study of risk factors and hospital variation. Surgery 161(6):1619–1627
Murray AC, Chiuzan C, Kiran RP (2016) Risk of anastomotic leak after laparoscopic versus open colectomy. Surg Endosc 30(12):5275–5282
Midura EF, Hanseman D, Davis BR et al (2015) Risk factors and consequences of anastomotic leak after colectomy. Dis Colon Rectum 58(3):333–338. https://doi.org/10.1097/DCR.0000000000000249
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85:355–358. https://doi.org/10.1046/j.1365-2168.1998.00615.x
Alves A, Panis Y, Pocard M et al (1999) Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg 189:554–559. https://doi.org/10.1016/S1072-7515(99)00207-0
Eckmann C, Kujath P, Schiedeck THK et al (2004) Anastomotic leakage following low anterior resection: results of a standardized diagnostic and therapeutic approach. Int J Colorectal Dis 19:128–133. https://doi.org/10.1007/s00384-003-0498-8
Kang CY, Halabi WJ, Chaudhry OO et al (2013) Risk factors for anastomotic leakage after anterior resection for rectal cancer. JAMA Surg 148(1):65–71. https://doi.org/10.1001/2013.jamasurg.2
Leester B, Asztalos I, Polnyib C (2002) Septic complications after low anterior rectal resection—is diverting stoma still justified? Acta Chir Iugosl 49(2):67–71
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246(2):207–214. https://doi.org/10.1097/SLA.0b013e3180603024
Shaban F, Carney K, McGarry K, Holtham S (2018) Perforated diverticulitis: to anastomose or not to anastomose? A systematic review and meta-analysis. Int J Surg 58:11–21
Sparreboom CL, van Groningen JT, Lingsma HF et al (2018) Different risk factors for early and late colorectal anastomotic leakage in a nationwide audit. Dis Colon Rectum 61(11):1258–1266
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary? Langenbecks Arch Surg 400:145–152. https://doi.org/10.1007/s00423-015-1275-1
Ondrula DP, Nelson RL, Prasad ML et al (1992) Multifactorial index of preoperative risk factors in colon resections. Dis Colon Rectum 35:117–122. https://doi.org/10.1007/BF02050665
McKenna NP, Bews KA, Cima RR et al (2020) Development of a risk score to predict anastomotic leak after left-sided colectomy: which patients warrant diversion? J Gastrointest Surg 24:132–143
Boyce SA, Harris C, Stevenson A, Lumley J, Clark D (2017) Management of low colorectal anastomotic leakage in the laparoscopic era: more than a decade of experience. Dis Colon Rectum 60(8):807–814. https://doi.org/10.1097/DCR.0000000000000822
Cauley CE, Ruchin BS, Bordeianou L (2018) Use of primary anastomosis with diverting ileostomy in patients with acute diverticulitis requiring urgent operative intervention. Dis Col Rectum 61(5):586–592
Baucom RB, Poulose BK, Herline AJ et al (2015) Smoking as a dominant risk factor for anastomotic leak after left colon resection. Am J Surgery 210(1):1–5
Richards CH, Campbell V, Ho C et al (2012) Smoking is a major risk factor for anastomotic leak in patients undergoing low anterior resection. Colorect Dis 14(5):628–633
Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P (2002) Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg 26(4):499–502. https://doi.org/10.1007/s00268-001-0256-4
Phan K, Oh L, Ctercteko G et al (2019) Does a stoma reduce the risk of anastomotic leak and need for re-operation following low anterior resection for rectal cancer: systematic review and meta-analysis of randomized controlled trials. J Gastrointest Oncol 10(2):179–187. https://doi.org/10.21037/jgo.2018.11.07
Hawkins AT, Dharmarajan S, Wells KK et al (2016) Does diverting loop ileostomy improve outcomes following open ileo-colic anastomoses? A Nationwide Analysis. J Gastrointest Surg 20:1738–1743
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Hoffman, R.L., Consuegra, H., Long, K. et al. Anastomotic leak in patients with acute complicated diverticulitis undergoing primary anastomosis: risk factors and the role of diverting loop ileostomy. Int J Colorectal Dis 36, 1543–1550 (2021). https://doi.org/10.1007/s00384-021-03957-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03957-z