Abstract
Objective
To evaluate comparative outcomes of temporary loop ileostomy closure during or after adjuvant chemotherapy following rectal cancer resection.
Methods
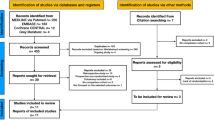
We systematic searched MEDLINE, EMBASE, CINAHL, CENTRAL, the World Health Organization International Clinical Trials Registry, ClinicalTrials.gov, ISRCTN Register and bibliographic reference lists. Overall perioperative complications, anastomotic leak, surgical site infection, ileus and length of hospital stay were the evaluated outcome parameters. Combined overall effect sizes were calculated using fixed effects or random effects models.
Results
We identified 4 studies reporting a total of 436 patients comparing outcomes of temporary loop ileostomy closure during (n = 185) or after (n = 251) adjuvant chemotherapy following colorectal cancer resection. There was no significant difference in overall perioperative complications (OR 1.39; 95% CI 0.82–2.36, p = 0.22), anastomotic leak (OR 2.80; 95% CI 0.47–16.56, p = 0.26), surgical site infection (OR 1.97; 95% CI 0.80–4.90, p = 0.14), ileus (OR 1.22; 95% CI 0.50–2.96, p = 0.66) or length of hospital stay (MD 0.02; 95% CI − 0.85–0.89, p = 0.97) between two groups. Between-study heterogeneity was low in all analyses.
Conclusions
The meta-analysis of the best, albeit limited, available evidence suggests that temporary loop ileostomy closure during adjuvant chemotherapy following rectal cancer resection may be associated with comparable outcomes to the closure of ileostomy after adjuvant chemotherapy. We encourage future research to concentrate on the completeness of chemotherapy and quality of life which can determine the appropriateness of either approach.


Similar content being viewed by others
References
Meyer JE, Narang T, Schnoll-Sussman FH, Pochapin MB, Christos PJ, Sherr DL (2010) Increasing incidence of rectal cancer in patients aged younger than 40 years: an analysis of the surveillance, epidemiology, and end results database. Cancer 116:4354–4359
Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H, Working Group ‘Colon/Rectum Carcinoma’ (2005) Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg 92(9):11137–11142
Heald RJ (1995) Total mesorectal excision is optimal surgery for rectal cancer: a Scandinavian consensus. Br J Surg 82(10):1297–1299
Nicholls RJ, Hall C (1996) Treatment of non-disseminated cancer of the lower rectum. Br J Surg 83(1):15–18
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246(2):207–214
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev 12(5):CD006878
Bakx R, Busch OR, Bemelman WA, Veldink GJ, Slors JF, van Lanschot JJ (2004) Morbidity of temporary loop ileostomies. Dig Surg 21(4):277–281
Tsunoda A, Nakao K, Hiratsuka K, Tsunoda Y, Kusano M (2007) Prospective analysis of quality of life in the first year after colorectal cancer surgery. Acta Oncol 46(1):77–82
Perdawid SK, Andersen OB (2011) Acceptable results of early closure of loop ileostomy to protect low rectal anastomosis. Dan Med Bull 58:A4280
Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E (2008) Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg 95:693–698
Hindenburg T, Rosenberg J (2010) Closing a temporary ileostomy within two weeks. Dan Med Bull 57:A4157
Krand O, Yalti T, Berber I, Tellioglu G (2008) Early vs. delayed closure of temporary covering ileostomy: a prospective study. Hepatogastroenterology 55:142–145
Sandra-Petrescu F, Herrle F, Hinke A, Rossion I, Suelberg H, Post S, Hofheinz RD, Kienle P (2015) CoCStom trial: study protocol for a randomised trial comparing completeness of adjuvant chemotherapy after early versus late diverting stoma closure in low anterior resection for rectal cancer. BMC Cancer 15:923
Oliphant R, Czerniewski A, Robertson I, McNulty C, Waterston A, Macdonald A (2015) The effect of adjuvant chemotherapy on stoma-related complications after surgery for colorectal cancer: a retrospective analysis. J Wound Ostomy Continence Nurs 42(5):494–498
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed Feb 2018
Higgins JP, Altman DG (eds). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S (eds). Cochrane handbook for systematic reviews of interventions. Version 5.0.1 [updated September 2008]. Available at: http://hiv.cochrane.org/sites/hiv. cochrane.org/files/uploads/Ch08_Bias.pdf. Accessed Feb 2018
Zhen L, Wang Y, Zhang Z, Wu T, Liu R, Li T, Zhao L, Deng H, Qi X, Li G (2017) Effectiveness between early and late temporary ileostomy closure in patients with rectal cancer: a prospective study. Curr Probl Cancer 41(3):231–240
Kye BH, Kim HJ, Kim JG, Cho HM (2014) Is it safe the reversal of a diverting stoma during adjuvant chemotherapy in elderly rectal cancer patients? Int J Surg 12(12):1337–1341
Tulchinsky H, Shacham-Shmueli E, Klausner JM, Inbar M, Geva R (2014) Should a loop ileostomy closure in rectal cancer patients be done during or after adjuvant chemotherapy? J Surg Oncol 109(3):266–269
Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D (2006) Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum 49:1011–1017
Petersen SH, Harling H, Kirkeby LT, Wille-Jørgensen P, Mocellin S (2012) Postoperative adjuvant chemotherapy in rectal cancer operated for cure. Cochrane Database Syst Rev 14(3):CD004078
National Comprehensive Cancer Network. Network NCC rectal cancer, NCCN guidelines 2015; Version 3
Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM (2011) Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA 305(22):2335–2342
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42(10):3171–3178
O’Leary DP, Fide CJ, Foy C, Lucarotti ME (2001) Quality of life after low anterior resection with total mesorectal excision and temporary loop ileostomy for rectal carcinoma. Br J Surg 88:1216–1220
Hajibandeh S, Hajibandeh S, Kennedy-Dalby A, Rehman S, Zadeh RA (2018) Purse-string skin closure versus linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Color Dis 33(10):1319–1332
Author information
Authors and Affiliations
Contributions
Conception and design: Shahin H, RP
Literature search and study selection: Shahin H, Shahab H, JE
Data collection: Shahin H, Shahab H
Analysis and interpretation: Shahin H, Shahab H
Writing the article: Shahin H, Shahab H
Critical revision of the article: All authors
Final approval of the article: All authors
Statistical analysis: Shahin H, Shahab H
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Sarma, D.R. et al. Meta-analysis of temporary loop ileostomy closure during or after adjuvant chemotherapy following rectal cancer resection: the dilemma remains. Int J Colorectal Dis 34, 1151–1159 (2019). https://doi.org/10.1007/s00384-019-03321-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03321-2