Abstract
Purpose
There is a lack of data-driven, risk-adjusted mortality estimates for injured children outside of high-income countries (HIC). To inform injury prevention and quality improvement efforts, an upper middle-income country (UMIC) pediatric trauma registry was compared to that of a HIC.
Methods
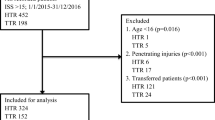
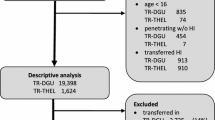
Clinical data, injury details, and mortality of injured children (< 18 years) hospitalized in two centers (USA and South African (SA)) from 2013 to 2017 were abstracted. Univariate and multivariable analyses evaluated risk of mortality and were expressed as odds ratios (OR) with 95% confidence intervals (CI).
Results
Of 2089 patients, SA patients had prolonged transfer times (21.1 vs 3.4 h) and were more likely referred (78.2% vs 53.9%; both p < 0.001). Penetrating injuries were more frequent in SA (23.2% vs 7.4%, p < 0.001); injury severity (9 vs 4) and shock index (0.90 vs 0.80) were greater (both p < 0.001). SA utilized cross-sectional imaging more frequently (66.4% vs 37.3%, p < 0.001). In-hospital mortality was similar (1.9% SA, 1.3% USA, p = 0.31). Upon multivariable analysis, ISS > 25 [210.50 (66.0-671.0)] and penetrating injury [5.5 (1.3–23.3)] were associated with mortality, while institution [1.7 (0.7–4.2)] was not.
Conclusions
Despite transfer time, the centers demonstrated comparable survival rates. Comparison of registry data can alert clinicians to problematic practice patterns, assisting initiatives to improve trauma systems.


Similar content being viewed by others
References
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32:533–536. https://doi.org/10.1007/s00268-008-9525-9
West JG, Cales RH, Gazzaniga AB (1983) Impact of regionalization. The Orange County experience. Arch Surg Chic Ill 1960 118:740–744
MacKenzie EJ, Rivara FP, Jurkovich GJ et al (2006) A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 354:366–378. https://doi.org/10.1056/NEJMsa052049
Gabbe BJ, Simpson PM, Sutherland AM et al (2012) Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg 255:1009–1015. https://doi.org/10.1097/SLA.0b013e31824c4b91
World Bank Country and Lending Groups—World Bank Data Help Desk (2019) https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed 9 Jan 2019
Meara JG, Leather AJ, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 386:569–624
Laing GL, Bruce JL, Skinner DL et al (2014) Development, implementation, and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg 38:1388–1397. https://doi.org/10.1007/s00268-013-2438-2
Laing G, Bruce J, Skinner D et al (2015) Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg 39:70–79. https://doi.org/10.1007/s00268-014-2766-x
Manchev V, Bruce J, Oosthuizen G et al (2015) The incidence, spectrum and outcome of paediatric trauma managed by the Pietermaritzburg Metropolitan Trauma Service. Ann R Coll Surg Engl 97:274–278. https://doi.org/10.1308/003588414X14055925061595
Brown JB, Gestring ML, Leeper CM et al (2017) The value of the injury severity score in pediatric trauma: time for a new definition of severe injury? J Trauma Acute Care Surg 82:995–1001. https://doi.org/10.1097/TA.0000000000001440
Bickler SW, Rode H (2002) Surgical services for children in developing countries. Bull World Health Organ 80:829–835
World Health Organization (2002) The injury chart book: a graphical overview of the global burden of injuries. World Health Organization, Geneva
Peclet MH, Newman KD, Eichelberger MR et al (1990) Patterns of injury in children. J Pediatr Surg 25:85–90 (discussion 90–91)
Bayreuther J, Wagener S, Woodford M et al (2009) Paediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Pract Ed 94:37–41. https://doi.org/10.1136/adc.2007.132787
Kristiansen T, Rehn M, Gravseth HM et al (2012) Paediatric trauma mortality in Norway: a population-based study of injury characteristics and urban-rural differences. Injury 43:1865–1872. https://doi.org/10.1016/j.injury.2011.08.011
Abantanga FA, Mock CN (1998) Childhood injuries in an urban area of Ghana A hospital-based study of 677 cases. Pediatr Surg Int 13:515–518. https://doi.org/10.1007/s003830050387
Simon R, Gilyoma JM, Dass RM et al (2013) Paediatric injuries at Bugando Medical Centre in Northwestern Tanzania: a prospective review of 150 cases. J Trauma Manag Outcomes 7:10. https://doi.org/10.1186/1752-2897-7-10
Eighemhenrio A, Campbell F, Fred FE et al (2015) Paediatric trauma at a tertiary hospital in Niger-Delta, Nigeria: a 5-year review. East Cent Afr J Surg 20:66–72
Spence RT, Scott JW, Haider A et al (2017) Comparative assessment of in-hospital trauma mortality at a South African trauma center and matched patients treated in the United States. Surgery 162:620–627. https://doi.org/10.1016/j.surg.2017.04.024
Lasecki CH, Mujica FC, Stutsman S et al (2018) Geospatial mapping can be used to identify geographic areas and social factors associated with intentional injury as targets for prevention efforts distinct to a given community. J Trauma Acute Care Surg 84:70–74. https://doi.org/10.1097/TA.0000000000001720
Haider AH, Hashmi ZG, Gupta S et al (2014) Benchmarking of trauma care worldwide: the potential value of an international trauma data bank (ITDB). World J Surg 38:1882–1891. https://doi.org/10.1007/s00268-014-2629-5
Breen J (2004) Road safety advocacy. The BMJ 328:888–890
Herbert HK, van As AB, Bachani AM et al (2012) Patterns of pediatric injury in South Africa: an analysis of hospital data between 1997 and 2006. J Trauma Acute Care Surg 73:168–174. https://doi.org/10.1097/TA.0b013e31824d67c3
Ochola FO, Okumu MO, Mwangi GM et al (2018) Epidemiology of snake bites in selected areas of Kenya. Pan Afr Med J. https://doi.org/10.11604/pamj.2018.29.217.15366
Roudsari BS, Psoter KJ, Vavilala MS et al (2013) CT use in hospitalized pediatric trauma patients: 15-year trends in a level I pediatric and adult trauma center. Radiology 267:479–486. https://doi.org/10.1148/radiol.13120865
Dicker RA, Sartorelli KH, McBrids WJ, Vane DW (1996) Penetrating hepatic trauma in children: operating room or not? J Pediatr Surg 31:1189–1191 (discussion 1191–1193)
Seidenberg P, Cerwensky K, Brown RO et al (2014) Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med 4:115–122. https://doi.org/10.1016/j.afjem.2014.01.006
Gabbe BJ, Biostat GD, Lecky FE et al (2011) The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United kingdom and victoria, australia. Ann Surg 253:138–143. https://doi.org/10.1097/SLA.0b013e3181f6685b
Meel BL (2003) Mortality of children in the Transkei region of South Africa. Am J Forensic Med Pathol 24:141–147. https://doi.org/10.1097/01.PAF.0128052262.54227.DD
Funding
The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Informed consent
This research was reviewed by both the Mayo Clinic and the Biomedical Research Committee (BREC) of the University of KwaZulu-Natal and determined to be exempt from the requirement for IRB approval and informed consent (45 CFR 46.101, item 4).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
The definitions of low-, middle-, lower middle-, upper middle-, and high-income countries are included below. These definitions are based upon Gross National Income (GNI) per capita using the World Bank Atlas method for the 2019 fiscal year. They can be found at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
Classification | World Bank definition |
|---|---|
Low income | Low-income economies are those with GNI per capita of $995 or less in 2017 |
Lower middle income | Lower middle-income economies are those with a GNI per capita of more than $995 but less than $3896 |
Middle income | Middle-income economies are those with a GNI per capita between $996 and $12,055 |
Upper middle income | Upper middle-income economies those with a GNI per capita of more than $3895 but less than $12,056 |
High income | High-income economies are those with a GNI per capita of $12,056 or more |
Rights and permissions
About this article
Cite this article
Traynor, M.D., Hernandez, M.C., Shariq, O. et al. Trauma registry data as a tool for comparison of practice patterns and outcomes between low- and middle-income and high-income healthcare settings. Pediatr Surg Int 35, 699–708 (2019). https://doi.org/10.1007/s00383-019-04453-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04453-w