Abstract
Purpose
Postoperative analgesia after corrective surgery of pediatric craniosynostosis is crucial in terms of short- and long-term outcomes. The objective of this observational study was to evaluate the effectiveness of an analgesic technique based on the scalp block versus traditional pharmacological approach.
Methods
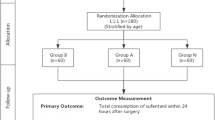
Thirteen patients, aged between 3 months and 2 years, undergoing surgical correction of craniosynostosis, received scalp nerve block before awakening (scalp block group). This group of patients was compared to a second group of 13 patients, retrieved from our database, treated with the traditional pharmacological approach (control group). Pain scores, need of rescue therapy, resumption of oral nutrition, degree of parent satisfaction at discharge, and length of stay in the Pediatric Intensive Care Unit (PICU) and in the hospital were compared between the two groups.
Results
Objective Pain Score values were significantly lower in patients treated with scalp block at 30 min and at 8 h after extubation. The number of pharmacological interventions for the treatment of pain in PICU was significantly higher in Control group. Children in Scalp block group started earlier oral feeding than in Control group, both for clear fluids and milk. Length of stay in PICU was longer in Scalp block group than in Control group, though the difference between the mean data in the two groups is about 3 . This difference does not seem significant from a clinical standpoint, since it seems more related to logistic issues (e.g., availability of bed in the Pediatric Neurosurgery Unit, presence of a parent), rather than clinical problems contraindicating the discharge from PICU. Indeed, the overall hospital length of stay was similar between the two groups.
Conclusion
Scalp nerve block was effective for immediate postoperative pain control in patients younger than 2 years who underwent cranioplasty for craniosynostosis. The best pain control compared to conventional therapy allowed to limit the need for rescue analgesics in PICU and an earlier recovery time.
ClinicalTrials.gov Identification: NCT04133467


Similar content being viewed by others
References
Adetayo OA, Poggi J (2015) Evaluating the efficacy and safety of scalp blocks in nonsyndromic craniosynostosis surgery. Paediatr Anaesth 25(11):1174–1175. https://doi.org/10.1111/pan.12716
Andersen RD, Langius-Eklöf A, Nakstad B, Bernklev T, Jylli L (2017) The measurement properties of pediatric observational pain scales: a systematic review of reviews. Int J Nurs Stud 73:93–101
Arnetz JE, Arnetz BB (1996) The development and application of a patient satisfaction measurement system for hospital-wide quality improvement. Int J Qual Health Care 6:555–566
Bebawy JF, Bilotta F, Koht A (2014) A modified technique for auriculotemporal nerve blockade when performing selective scalp nerve block for craniotomy. J Neurosurgical Anesthesiol 26:271–272
Beverly A, Kaye AD, Ljungqvist O, Urman RD (2017) Essential elements of multimodal analgesia in Enhanced Recovery After Surgery (ERAS) guidelines. Anesthesiol Clin 35(2):e115–e143
Bronco A, Pietrini D, Lamperti M, Somaini M, Tosi F, Minguell del Lungo L, Zeimantz E, Tumolo M, Lampugnani E, Astuto M, Perna F, Zadra N, Meneghini L, Benucci V, Bussolin L, Scolari A, Savioli A, Locatelli BG, Prussiani V, Cazzaniga M, Mazzoleni F, Giussani C, Rota M, Ferland CE, Ingelmo PM (2014) Incidence of pain after craniotomy in children. Pediatr Anesth 24:781–787
Cercueil E, Migeon A, Desgranges FP, Chassard D, Bouvet L (2018) Postoperative analgesia for craniosynostosis reconstruction: scalp nerve block or local anesthetic infiltration? Paediatr Anaesth 28(5):474–475. https://doi.org/10.1111/pan.13356
Di Rocco C, Frassanito P, Tamburrini G (2013) The shell technique: bilateral fronto-orbital reshaping in trigonocephaly. Childs Nerv Syst 29(12):2189–2194. https://doi.org/10.1007/s00381-012-1766-0
Di Rocco C, Frassanito P, Pelo S, Tamburrini G (2016) In: Cohen AR (ed) Syndromic craniosynostosis, in pediatric neurosurgery: tricks of the trade. Thieme Medical Publishers
Guilfoyle MR, Helmy A, Duane D, Hutchinson PJA (2013) Regional scalp block for postcraniotomy analgesia: a systematic review and meta-analysis. Anesth Analg 116(5):1093–1102
Hughes C, Thomas K, Johnson D, Das S (2013) Anesthesia for surgery related to craniosynostosis: a review. Part 2. Paediatr Anaesth 23(1):22–27
Kemp WJ 3rd, Tubbs RS, Cohen-Gadol AA (2011) The innervation of the scalp: a comprehensive review including anatomy, pathology, and neurosurgical correlates. Surg Neurol Int 2:178
Lundeberg S, Lönnqvist PA (2004) Update on systemic postoperative analgesia in children. Paediatr Anaesth 14(5):394–397
Macmillan A, Kattail D, Faateh M, Pedreira R, Musavi L, Cho R, Lopez J, Dorafshar AH (2017) Craniosynostosis surgery: a painless procedure? A single institution’s experience in postoperative pain management. Plast Reconstr Surg Glob Open 5(2 Suppl):6
Massimi L, Di Rocco C (2012) Mini-invasive surgical technique for sagittal craniosynostosis. Childs Nerv Syst 28(9):1341–1345. https://doi.org/10.1007/s00381-012-1799-4
McGrath PJ, Johnston G, Goodman JT (1985) CHEOPS: a behavioral scale for rating postoperative pain in children. Adv Pain Res Ther 9:395–402
Merkel SI, Voepel-Lewis T (1997) The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs 23:293–297
Norden J, Hannallah R, Geston P et al (1991) Reliability of an objective pain scale in children. J Pain Symptom Manag 6:196
Pardey Bracho GF, Grousson S, de Souza EP et al (2008) Levobupivacaine scalp nerve block in children. Pediatr Anesth 18:271–272
Pardey Bracho GF, Pereira de Souza Neto E, Grousson S et al (2014) Opioid consumption after levobupivacaine scalp nerve block for craniosynostosis surgery. Acta Anaesthesiol Taiwanica 52(2):64–69
Phillips S, Gift M, Gelot S, Duong M, Tapp H (2013) Assessing the relationship between the level of pain control and patient satisfaction. J Pain Res 6:683–689
Pinosky ML, Fishman RL, Reeves ST, Harvey SC, Patel S, Palesch Y, Dorman BH (1996) The effect of bupivacaine skull block on the hemodynamic response to craniotomy. Anesth Analg 83:1256–1261
Rothera E, Chumas P, Liddington M, Russell J, Guruswamy V (2014) Scalp blocks in nonsyndromic craniosynostosis surgery - a retrospective case series review. Paediatr Anaesth 24(8):894–895. https://doi.org/10.1111/pan.12465
Schnabel A, Schnabel A, Reichl SU, Meyer-Frießem C et al (2015) Tramadol for postoperative pain treatment in children. Cochrane Database Syst Rev 18(3):CD009574
Stricker PA, Goobie SM, Cladis FP, Haberkern CM, Meier PM, Reddy SK, Nguyen TT, Cai L, Polansky M, Szmuk P, Fiadjoe J, Soneru C, Falcon R, Petersen T, Kowalczyk-Derderian C, Dalesio N, Budac S, Groenewald N, Rubens D, Thompson D, Watts R, Gentry K, Ivanova I, Hetmaniuk M, Hsieh V, Collins M, Wong K, Binstock W, Reid R, Poteet-Schwartz K, Gries H, Hall R, Koh J, Bannister C, Sung W, Jain R, Fernandez A, Tuite GF, Ruas E, Drozhinin O, Tetreault L, Muldowney B, Ricketts K, Fernandez P, Sohn L, Hajduk J, Taicher B, Burkhart J, Wright A, Kugler J, Barajas-DeLoa L, Gangadharan M, Busso V, Stallworth K, Staudt S, Labovsky KL, Glover CD, Huang H, Karlberg-Hippard H, Capehart S, Streckfus C, Nguyen KPT, Manyang P, Martinez JL, Hansen JK, Levy HM, Brzenski A, Chiao F, Ingelmo P, Mujallid R, Olutoye OA, Syed T, Benzon H, Bosenberg A (2017) Perioperative outcomes and management in pediatric complex cranial vault reconstruction: a multicenter study from the Pediatric Craniofacial Collaborative Group. Anesthesiology 126(2):276–287
Tamburrini G, Caldarelli M, Massimi L, Gasparini G, Pelo S, Di Rocco C (2012) Complex craniosynostoses: a review of the prominent clinical features and the related management strategies. Childs Nerv Syst 28(9):1511–1523. https://doi.org/10.1007/s00381-012-1819-4
Tawfic Q, Kumar K, Pirani Z, Armstrong K (2017) Prevention of chronic post-surgical pain: the importance of early identification of risk factors. J Anesth 31(3):424–431
Teo JH, Palmer GM, Davidson AJ (2011) Post-craniotomy pain in a pediatric population. Anaesth Intensive Care 39(1):89–94
Thomas K, Hughes C, Johnson D, Das S (2012) Anesthesia for surgery related to craniosynostosis: a review. Part 1. Paediatr Anaesth 22(11):1033–1041
Warren DT, Bowen-Robert T, Ou C et al (2010) Safety and efficacy of continuous morphine infusions following pediatric cranial surgery in a surgical ward setting. Childs Nerv Syst 26(11):1535–1541
Xing F, An LX, Xue FS, Zhao CM, Bai YF (2019) Postoperative analgesia for pediatric craniotomy patients: a randomized controlled trial. BMC Anesthesiol 19:53
Ygge BM, Arnetz JE (2001) Quality of pediatric care: application and validation of an instrument for measuring parent satisfaction with hospital care. Int J Qual Health Care 13:33–43
Funding
The authors received no funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interests.
Ethics approval
The study protocol was approved by the institutional Ethics Committee: Prot. 14,138/18 (3258/19), ID: 2024.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Festa, R., Tosi, F., Pusateri, A. et al. The scalp block for postoperative pain control in craniosynostosis surgery: a case control study. Childs Nerv Syst 36, 3063–3070 (2020). https://doi.org/10.1007/s00381-020-04661-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04661-z