Abstract
Objective
To analyze factors associated with the development of early symptomatic hydrocephalus following posterior fossa tumor (PFT) surgery in children.
Methods
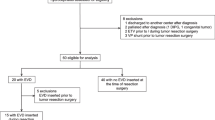
In this retrospective study, data from 148 children (age < 18 years) who underwent primary resection of their PFTs without preoperative permanent CSF diversion procedures were collected. The incidence of symptomatic hydrocephalus within 30 days of tumor resection was studied and its association with various demographic, tumor-related, and surgery-related risk factors was analyzed.
Results
At presentation, 131 (89%) of the 148 patients had symptomatic hydrocephalus. There were 99 males and 49 females (mean age 8.7 years; range 1 to 17 years). Postoperatively, 14 (9.4%) patients required shunt placement for symptomatic hydrocephalus. The indications for shunt surgery were persistent symptoms of raised intracranial pressure (n = 6, 43%), CSF leak from the wound (n = 7, 50%), and tense pseudomeningocele (n = 1, 7%). On multivariate analysis, age < 6 years (OR 5.9, 95% CI 1.6–22.6, p = 0.009) and the presence of intraventricular blood (IVB) on postoperative CT (OR 6.4, 95% CI 1.7–23.7, p = 0.006) were independent risk factors for developing symptomatic hydrocephalus.
Conclusions
The incidence of postoperative symptomatic hydrocephalus in our series (9.4%) is lower than that reported in most previous studies. Age < 6 years and the presence of postoperative IVB were independent risk factors for developing symptomatic hydrocephalus. Of these, postoperative IVB is probably the only modifiable risk factor.


Similar content being viewed by others
References
Dewan MC, Lim J, Shannon CN, Wellons JC (2017) The durability of endoscopic third ventriculostomy and ventriculoperitoneal shunts in children with hydrocephalus following posterior fossa tumor resection: a systematic review and time-to-failure analysis. J Neurosurg Pediatr 19:578–584. https://doi.org/10.3171/2017.1.PEDS16536
Riva-Cambrin J, Detsky AS, Lamberti-Pasculli M, Sargent MA, Armstrong D, Moineddin R, Cochrane DD, Drake JM (2009) Predicting postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 3:378–385. https://doi.org/10.3171/2009.1.PEDS08298
Dias MS, Albright AL (1989) Management of hydrocephalus complicating childhood posterior fossa tumors. Pediatr Neurosci 15:283–290
Kumar V, Phipps K, Harkness W, Hayward RD (1996) Ventriculo-peritoneal shunt requirement in children with posterior fossa tumours: an 11-year audit. Br J Neurosurg 10:467–470
Raimondi AJ, Tomita T (1981) Hydrocephalus and infratentorial tumors. Incidence, clinical picture, and treatment. J Neurosurg 55:174–182. https://doi.org/10.3171/jns.1981.55.2.0174
Bognár L, Borgulya G, Benke P, Madarassy G (2003) Analysis of CSF shunting procedure requirement in children with posterior fossa tumors. Childs Nerv Syst 19:332–336. https://doi.org/10.1007/s00381-003-0745-x
Due-Tønnessen BJ, Helseth E (2007) Management of hydrocephalus in children with posterior fossa tumors: role of tumor surgery. Pediatr Neurosurg 43:92–96. https://doi.org/10.1159/000098379
Gopalakrishnan CV, Dhakoji A, Menon G, Nair S (2012) Factors predicting the need for cerebrospinal fluid diversion following posterior fossa tumor surgery in children. Pediatr Neurosurg 48:93–101. https://doi.org/10.1159/000343009
Lee M, Wisoff JH, Abbott R, Freed D, Epstein FJ (1994) Management of hydrocephalus in children with medulloblastoma: prognostic factors for shunting. Pediatr Neurosurg 20:240–247. https://doi.org/10.1159/000120797
Papo I, Caruselli G, Luongo A (1982) External ventricular drainage in the management of posterior fossa tumors in children and adolescents. Neurosurgery 10:13–15
Lin C-T, Riva-Cambrin JK (2015) Management of posterior fossa tumors and hydrocephalus in children: a review. Childs Nerv Syst 31:1781–1789. https://doi.org/10.1007/s00381-015-2781-8
Evans WA Jr (1942) An encephalographic ratio for estimating ventricular enlargement and cerebral atrophy. Arch Neurol Psychiatr 47:931–937. https://doi.org/10.1001/archneurpsyc.1942.02290060069004
Moorthy RK, Sarkar H, Rajshekhar V (2013) Conservative antibiotic policy in patients undergoing non-trauma cranial surgery does not result in higher rates of postoperative meningitis: an audit of nine years of narrow-spectrum prophylaxis. Br J Neurosurg 27:497–502. https://doi.org/10.3109/02688697.2013.771138
Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34:402–408
Abraham J, Chandy J (1963) Ventriculo-atrial shunt in the management of posterior-fossa tumours: preliminary report. J Neurosurg 20:252–253. https://doi.org/10.3171/jns.1963.20.3.0252
Albright L, Reigel DH (1977) Management of hydrocephalus secondary to posterior fossa tumors. J Neurosurg 46:52–55. https://doi.org/10.3171/jns.1977.46.1.0052
Sainte-Rose C, Cinalli G, Roux FE et al (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95:791–797. https://doi.org/10.3171/jns.2001.95.5.0791
Ruggiero C, Cinalli G, Spennato P et al (2004) Endoscopic third ventriculostomy in the treatment of hydrocephalus in posterior fossa tumors in children. Childs Nerv Syst 20:828–833. https://doi.org/10.1007/s00381-004-0938-y
Bhatia R, Tahir M, Chandler CL (2009) The management of hydrocephalus in children with posterior fossa tumours: the role of pre-resectional endoscopic third ventriculostomy. Pediatr Neurosurg 45:186–191. https://doi.org/10.1159/000222668
El Beltagy MA, Kamal HM, Taha H, Awad M, El Khateeb N (2010) Endoscopic third ventriculostomy before tumor surgery in children with posterior fossa tumors, CCHE experience. Childs Nerv Syst 26:1699–1704. https://doi.org/10.1007/s00381-010-1180-4
Epstein F, Murali R (1978) Pediatric posterior fossa tumors: hazards of the “preoperative” shunt. Neurosurgery 3:348–350
El-Gaidi MA, El-Nasr AHA, Eissa EM (2015) Infratentorial complications following preresection CSF diversion in children with posterior fossa tumors. J Neurosurg Pediatr 15:4–11. https://doi.org/10.3171/2014.8.PEDS14146
Santhanam R, Balasubramaniam A, Chandramouli BA (2009) Fatalintratumoral hemorrhage in posterior fossa tumors following ventriculoperitoneal shunt. J Clin Neurosci 16:135–137. https://doi.org/10.1016/j.jocn.2008.02.016
Goel A (1993) Whither preoperative shunts for posterior fossa tumours? Br J Neurosurg 7:395–399
Rappaport ZH, Shalit MN (1989) Perioperative external ventricular drainage in obstructive hydrocephalus secondary to infratentorial brain tumours. Acta Neurochir 96:118–121
Gnanalingham KK, Lafuente J, Thompson D, Harkness W, Hayward R (2003) The natural history of ventriculomegaly and tonsillar herniation in children with posterior fossa tumours – an MRI study. Pediatr Neurosurg 39:246–253. https://doi.org/10.1159/000072869
Santos de Oliveira R, Barros Jucá CE, Valera ET, Machado HR (2008) Hydrocephalus in posterior fossa tumors in children. Are there factors that determine a need for permanent cerebrospinal fluid diversion? Childs Nerv Syst 24:1397–1403. https://doi.org/10.1007/s00381-008-0649-x
Tamburrini G, Pettorini BL, Massimi L, Caldarelli M, Di Rocco C (2008) Endoscopic third ventriculostomy: the best option in the treatment of persistent hydrocephalus after posterior cranial fossa tumour removal? Childs Nerv Syst 24:1405–1412. https://doi.org/10.1007/s00381-008-0699-0
Foreman P, McClugage S, Naftel R, Griessenauer CJ, Ditty BJ, Agee BS, Riva-Cambrin J, Wellons J (2013) Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12:220–226. https://doi.org/10.3171/2013.5.PEDS1371
Schneider C, Ramaswamy V, Kulkarni AV et al (2015) Clinical implications of medulloblastoma subgroups: incidence of CSF diversion surgery. J Neurosurg Pediatr 15:236–242. https://doi.org/10.3171/2014.9.PEDS14280
Stein BM, Tenner MS, Fraser RA (1972) Hydrocephalus following removal of cerebellar astrocytomas in children. J Neurosurg 36:763–768. https://doi.org/10.3171/jns.1972.36.6.0763
Dubey AK, Rao KL (1997) Pathology of post meningitic hydrocephalus. Indian J Pediatr 64:30–33
Schmid UD, Seiler RW (1986) Management of obstructive hydrocephalus secondary to posterior fossa tumors by steroids and subcutaneous ventricular catheter reservoir. J Neurosurg 65:649–653. https://doi.org/10.3171/jns.1986.65.5.0649
Morelli D, Pirotte B, Lubansu A, Detemmerman D, Aeby A, Fricx C, Berré J, David P, Brotchi J (2005) Persistent hydrocephalus after early surgical management of posterior fossa tumors in children: is routine preoperative endoscopic third ventriculostomy justified? J Neurosurg 103:247–252. https://doi.org/10.3171/ped.2005.103.3.0247
Bu Y, Chen M, Gao T, Wang X, Li X, Gao F (2016) Mechanisms of hydrocephalus after intraventricular haemorrhage in adults. Stroke Vasc Neurol 1:23–27. https://doi.org/10.1136/svn-2015-000003
Strahle J, Garton HJL, Maher CO, Muraszko KM, Keep RF, Xi G (2012) Mechanisms of hydrocephalus after neonatal and adult intraventricular hemorrhage. Transl Stroke Res 3:25–38. https://doi.org/10.1007/s12975-012-0182-9
Kaestner S, Dimitriou I (2013) TGF beta1 and TGF beta2 and their role in posthemorrhagic hydrocephalus following SAH and IVH. J Neurol Surg A Cent Eur Neurosurg 74:279–284. https://doi.org/10.1055/s-0033-1342929
Gao C, Du H, Hua Y, Keep RF, Strahle J, Xi G (2014) Role of red blood cell lysis and iron in hydrocephalus after intraventricular hemorrhage. J Cereb Blood Flow Metab 34:1070–1075. https://doi.org/10.1038/jcbfm.2014.56
Gao F, Liu F, Chen Z, Hua Y, Keep RF, Xi G (2014) Hydrocephalus after intraventricular hemorrhage: the role of thrombin. J Cereb Blood Flow Metab 34:489–494. https://doi.org/10.1038/jcbfm.2013.225
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest. The datasets generated for the study are available from the corresponding author on reasonable request.
Additional information
A portion of this study was presented as a podium presentation at the 29th Annual Conference of the Indian Society for Pediatric Neurosurgery in February, 2018.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abraham, A.P., Moorthy, R.K., Jeyaseelan, L. et al. Postoperative intraventricular blood: a new modifiable risk factor for early postoperative symptomatic hydrocephalus in children with posterior fossa tumors. Childs Nerv Syst 35, 1137–1146 (2019). https://doi.org/10.1007/s00381-019-04195-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04195-z