Abstract
Purpose
To determine whether intraoperative adjunctive EVD placement in patients with a posterior fossa tumor (PFT) led to improved surgical, radiographic, and clinical outcomes compared to those who did not receive an EVD.
Methods
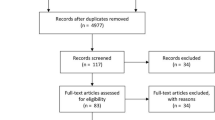
Patients were grouped as those who underwent routine intraoperative adjunctive EVD insertion and those who did not at time of PFT resection. Patients who pre-operatively required a clinically indicated EVD insertion were excluded. Comparative analyses between both groups were conducted to evaluate clinical, radiological, and pathological outcomes. Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were computed for post-operative outcomes.
Results
Fifty-five selected patients were included, 15 who had an EVD placed at the time of PFT resection surgery, and 40 who did not. Children without an EVD did not experience a higher rate of complications or poorer post-operative outcomes compared to those with an EVD placed during resection surgery. There was no significant difference in the degree of gross total resection (p = 0.129), post-operative CSF leak (p = 1.000), and post-operative hemorrhage (p = 0.554) between those with an EVD and those without. The frequency of new cranial nerve deficits post-operatively was higher in those with an EVD (40%) compared to those without (3%, p = 0.001). There was a trend towards more frequently observed post-operative hydrocephalus in the EVD group (p = 0.057).
Conclusion
The routine use of EVD as an intraoperative adjunct in clinically stable pediatric patients with posterior fossa tumors and hydrocephalus may not be associated with improved radiological or clinical outcomes.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- ETV:
-
Endoscopic third ventriculostomy
- EVD:
-
External ventricular drain
- ICP:
-
Intracranial pressure
- MRI:
-
Magnetic resonance imaging
- PFT:
-
Posterior fossa tumor
- VP:
-
Ventriculoperitoneal
References
Albright L, Reigel DH (1977) Management of hydrocephalus secondary to posterior fossa tumors. J Neurosurg 46:52–55
Papo I, Caruselli G, Luongo A (1982) External ventricular drainage in the management of posterior fossa tumors in children and adolescents. Neurosurgery 10:13–15
Bateman GA, Fiorentino M (2016) Childhood hydrocephalus secondary to posterior fossa tumor is both an intra- and extraaxial process. J Neurosurg Pediatr 18:21–28
Tamburrini G, Frassanito P, Bianchi F, Massimi L, Di Rocco C, Caldarelli M (2015) Closure of endoscopic third ventriculostomy after surgery for posterior cranial fossa tumor: the “snow globe effect.” Br J Neurosurg 29:386–389
Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34:402–408
Due-Tønnessen BJ, Helseth E (2007) Management of hydrocephalus in children with posterior fossa tumors: role of tumor surgery. Pediatr Neurosurg 43:92–96
Srinivasan HL, Foster MT, Van Baarsen K, Hennigan D, Pettorini B, Mallucci C (2020) Does pre-resection endoscopic third ventriculostomy prevent the need for post-resection CSF diversion after pediatric posterior fossa tumor excision? A historical cohort study and review of the literature. J Neurosurg Pediatr 25:615–624
Gopalakrishnan CV, Dhakoji A, Menon G, Nair S (2012) Factors predicting the need for cerebrospinal fluid diversion following posterior fossa tumor surgery in children. Pediatr Neurosurg 48:93–101
Azab W, Al-Sheikh T, Yahia A (2013) Preoperative endoscopic third ventriculostomy in children with posterior fossa tumors: an institution experience. Turk Neurosurg 23:359–365
Epstein F, Murali R (1978) Pediatric posterior fossa tumors: hazards of the “preoperative” shunt. Neurosurgery 3:348–350
McLaurin RL (1983) Disadvantages of the preoperative shunt in posterior fossa tumors. Clin Neurosurg 30:286–292
Bhatia R, Tahir M, Chandler CL (2009) The management of hydrocephalus in children with posterior fossa tumours: the role of pre-resectional endoscopic third ventriculostomy. Pediatr Neurosurg 45:186–191
Di Rocco F, Jucá CE, Zerah M, Sainte-Rose C (2013) Endoscopic third ventriculostomy and posterior fossa tumors. World Neurosurg 79:18.e15-19
Lam S, Reddy G, Lin Y, Jea A (2015) Management of hydrocephalus in children with posterior fossa tumors. Surg Neurol Int 6:S346-348
Morelli D, Pirotte B, Lubansu A et al (2005) Persistent hydrocephalus after early surgical management of posterior fossa tumors in children: is routine preoperative endoscopic third ventriculostomy justified? J Neurosurg 103:247–252
Merchant TE, Lee H, Zhu J et al (2004) The effects of hydrocephalus on intelligence quotient in children with localized infratentorial ependymoma before and after focal radiation therapy. J Neurosurg 101:159–168
Sainte-Rose C, Cinalli G, Roux FE et al (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95:791–797
Santos de Oliveira R, Barros Jucá CE, Terci Valera E et al (2008) Hydrocephalus in posterior fossa tumors in children. Are there factors that determine a need for permanent cerebrospinal fluid diversion? Childs Nerv Syst 24:1397–1403
Lee M, Wisoff JH, Abbott R et al (1994) Management of hydrocephalus in children with medulloblastoma: prognostic factors for shunting. Pediatr Neurosurg 20:240–247
Lin C, Riva-Cambrin JK (2015) Management of posterior fossa tumors and hydrocephalus in children: a review. Childs Nerv Syst 31:1781–1789
Bognár L, Borgulya G, Benke P et al (2003) Analysis of CSF shunting procedure requirement in children with posterior fossa tumors. Childs Nerv Syst 19:332–336
Tamburrini G, Pettorini BL, Massimi L (2008) Endoscopic third ventriculostomy: the best option in the treatment of persistent hydrocephalus after posterior cranial fossa tumour removal? Childs Nerv Syst 24:1405–1412
Rappaport ZH, Shalit MN (1989) Perioperative external ventricular drainage in obstructive hydrocephalus secondary to infratentorial brain tumours. Acta Neurochir 96:118–121
Won S-Y, Dubinski D, Behmanesh B et al (2020) Management of hydrocephalus after resection of posterior fossa lesions in pediatric and adult patients – predictors for development of hydrocephalus. Neurosurg Rev 43:1143–1150
Riva-Cambrin J, Detsky AS, Lamberti-Pasculli M et al (2009) Predicting postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 3:378–385
Foreman P, McClugage S, Naftel R et al (2013) Validation and modification of a predictive model for postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12:220–226
Won S-Y, Gessler F, Dubinski D et al (2019) A novel grading system for the prediction of the need for cerebrospinal fluid drainage following posterior fossa tumor surgery. J Neurosurg 132:296–305
Author information
Authors and Affiliations
Consortia
Contributions
LHV: conception, data analysis and interpretation, drafting and revising manuscript, final manuscript approval, and ensuring accuracy and integrity of the work; AM: data acquisition and analysis, drafting and revising manuscript, and final manuscript approval; NP: data acquisition and analysis, and final manuscript approval; BM: drafting and revising manuscript, and final manuscript approval; OA: conception, revising manuscript, and final manuscript approval; AF: conception, revising manuscript, final manuscript approval, and ensuring accuracy and integrity of the work; FF: data interpretation, revising manuscript, and final manuscript approval; SKS: conception, data interpretation, revising manuscript, final manuscript approval, and ensuring accuracy and integrity of the work; BY: conception, data interpretation, revising manuscript, final manuscript approval, and ensuring accuracy and integrity of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the ethical standards of McMaster University, and with the principles of the 1964 Declaration of Helsinki and its later amendments. Given the retrospective nature of this study, the Research Ethics Boards waived the need for consent to participate.
Consent for publication
Not applicable.
Conflict of interest
The authors have no financial or proprietary interests in any of the material discussed in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verhey, L.H., Maharaj, A., Patel, N. et al. External ventricular drainage in the management of pediatric patients with posterior fossa tumors and hydrocephalus: a retrospective cohort study. Childs Nerv Syst 39, 887–894 (2023). https://doi.org/10.1007/s00381-022-05818-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05818-8