Abstract
Objectives
Craniopharyngioma during childhood poses difficulty in management because of the high incidence of surgical complications and treatment failure. In order to identify less detrimental and more effective treatment, a personal series of craniopharyngioma was reviewed in regard to various clinical factors, patient factors (age and sex), tumor factors (location and extension, relationship with chiasm, and hydrocephalus), and therapeutic modes [extent of resection and radiation therapy (RT)].
Materials and methods
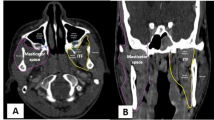
Fifty-four childhood craniopharyngiomas treated from 1984 to 2003 were reviewed. Preoperative neuroimaging studies were classified depending upon tumor location and extension. In this series of 54 patients, 43 had total tumor resection and 11 had subtotal resection. Of the total resection group, ten showed evidence of residual tumor on postoperative neuroimaging studies. Following the initial resection, 46 did not have RT whereas 8 with subtotal resection received RT.
Results
There were no surgical deaths. Postoperative complications included pseudoaneurysm in 1, hemiparesis in 3, severe obesity in 5, panhypopituitarism in 50, and worsening of visual function in 7. During follow-up ranging from 12 months to 21 years, 24 patients had recurrence. Of the 33 patients with radiographic total resection, 9 (27.3%) had recurrence. Among the patients with total resection but radiographic residual and those with subtotal resection, the craniopharyngioma recurred in 90% and 100%, respectively. Three (37.5%) of eight patients with subtotal resection with RT had recurrence. Overall recurrence-free survival was 62% at 5 years and 49% at 10 years. The sex and age, location and extension of the tumor, nature of the optic chiasm, and hydrocephalus did not influence survival with statistical significance. However, the extent of surgical resection and use of RT showed significant differences for survival. Patients with total resection had a recurrence-free survival rate of 83% and 70% at 5 and 10 years, respectively. Patients with subtotal resection with RT had 71% at 5 years and 36% at 10 years. Patients who had subtotal resection or radiographically residual tumor without RT had a recurrence-free survival rate of only 9%. Among 22 patients whose recurrent tumor was treated with RT, a second recurrence-free survival rate was 90% at 5 years.
Conclusion
Total resection provided the best outcome. However, recurrence rates and surgical complications remained high following radical tumor resection. RT was effective for recurrent tumors and should be considered being the primary treatment for recurrences or difficult tumors, which are not amenable to total resections.























Similar content being viewed by others
References
Abe T, Ludecke DK (1999) Transnasal surgery for infradiaphragmatic craniopharyngiomas in pediatric patients. Neurosurgery 44:957–966
CBTRUS (2004) Statistical report: primary brain tumors in the United States, 1997–2001. Central Brain Tumor Registry of the United States, Chicago, IL
Carpentieri SC, Waber DP, Scott RM, Goumnerova LC, Kieran MW, Cohen LE, Kim F (2001) Memory deficits among children with craniopharyngiomas. Neurosurgery 49:1053–1057
De Vile CJ, Grant DB, Kendal BE, Neville BGR, Stanhope R, Watkins KE, Hayward RD (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81
Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46:220–229
Flickinger JC, Lunsford LD, Singer J, Cano ER, Deutsch M (1990) Megavoltage external beam irradiation of craniopharyngiomas: analysis of tumor control and morbidity. Int J Radiat Oncol Biol Phys 19:117–122
Gonc EN, Yordam N, Ozon A, Alikasifoglu A, Kandemir N (2004) Endocrinological options in children with craniopharyngioma: a retrospective analysis of 66 cases. Pediatr Neurosurg 40:112–119
Habrand JL, Gantry O, Couanet D, Rouxel V, Levy-Piedbois C, Pierre-Kahn A, Kalifa C (1999) The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys 44:255–263
Hamamoto Y, Niino K, Adachi M, Hosoya T (2002) MR and CT findings of craniopharyngioma during and after radiation therapy. Neuroradiology 44:118–122
Hetelekidis S, Barnes PD, Tao ML, Fischer EG, Schneider L, Scott RM, Tarbell NJ (1993) 20-year experience in childhood craniopharyngioma. Int J Radiat Oncol Biol Phys 27:471–475
Hoffman HJ (1994) Surgical management of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):44–49
Hoffman HJ, De Silva M, Humphreys RP, Drake JM, Smith ML, Blaser SI (1992) Aggressive surgical management of craniopharyngiomas in children. J Neurosurg 76:47–52
Im SH, Wang KC, Kim SK, Chung YN, Kim HS, Lee CH, Cho BK (2003) Transsphenoidal microsurgery for pediatric craniopharyngioma: special considerations regarding indications and method. Pediatr Neurosurg 39:97–103
Kim SK, Wang KC, Shin SH, Choe G, Chi JG, Cho BK (2001) Radical resection of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Childs Nerv Syst 17:531–536
Kristopaitis T, Thomas C, Petruzzelli GJ, Lee JM (2000) Malignant craniopharyngioma. Arch Pathol Lab Med 124:1356–1360
Laws ER (1994) Transsphenoidal removal of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):57–63
Maira G, Anile C, Colosimo C, Cabezas D (2000) Craniopharyngioma of the third ventricle: trans-lamina terminalis approach. Neurosurgery 47:857–865
Maira G, Anile C, Albanese A, Cabezas D, Pardi F, Vignati A (2004) The role of transsphenoidal surgery in the treatment of craniopharyngiomas. J Neurosurg 100:445–451
Merchant TE, Kiehna EN, Sanford RA, Mulhern RK, Thompson SJ, Wilson MW, Lustig RH, Kun LE (2002) Craniopharyngioma: St. Jude children’s research hospital experience 1984–2001. Int J Radiat Oncol Biol Phys 53:533–542
Miller DC (1994) Pathology of craniopharyngiomas: clinical import of pathological findings. Pediatr Neurosurg 21(Suppl 1):11–17
Muller HL, Bueb K, Bartels U, Roth C, Harz K, Graf N, Korinthenberg R, Bettendorf M, Kuhl J, Gutjahr P, Sorensen N, Calaminus G (2001) Obesity after childhood craniopharyngioma—German multicenter study on pre-operative risk factors and quality of life. Klin Padiatr 213:244–249
Pascual JM, Gonzalez-Llanos F, Roda JM (2004) Intraventricular craniopharyngiomas: topographic classification and surgical approach selection based on an extensive overview. Acta Neurochir (Wien) 146:785–802
Patterson RH Jr, Danylevich A (1980) Surgical removal of craniopharyngiomas by a transsphenoidal approach through the lamina terminalis and sphenoid sinus. Neurosurgery 7:111–117
Pierre-Kahn A, Sainte-Rose C, Renier D (1994) Surgical approach to children with craniopharyngiomas and severely impaired vision: special considerations. Pediatr Neurosurg 21(Suppl 1):50–56
Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46:220–229
Price DA, Wilton P, Jonsson P, Albertsson-Wikland K, Chatelain P, Cutfield W, Ranke MB (1998) Efficacy and safety of growth hormone treatment in children with prior craniopharyngioma: an analysis of the Pharmacia and Upjohn International Growth Database (KIGS) from 1988 to 1996. Horm Res 49:91–97
Rajan B, Ashley S, Gorman C, Jose CC, Horwich A, Bloom HJ, Marsh H, Brada M (1993) Craniopharyngioma—a long-term results following limited surgery and radiotherapy. Radiother Oncol 26:1–10
Rajan B, Ashley S, Thomas DG, Marsh H, Britton J, Brada M (1997) Craniopharyngioma: improving outcome by early recognition and treatment of acute complications. Int J Radiat Oncol Biol Phys 37:517–521
Shibuya M, Takayasu M, Suzuki Y, Saito K, Sugita K (1996) Bifrontal basal interhemispheric approach to craniopharyngioma resection with or without division of the anterior communicating artery. J Neurosurg 84:951–956
Srinivasa J, Dailey AT, Berger MS (1999) The bifrontal olfactory nerve-sparing approach to lesions of the suprasellar region in children. Pediatr Neurosurg 30:245–252
Steno J, Malacek M, Bizik I (2004) Tumor-third ventricular relationships in supradiaphragmatic craniopharyngiomas: correlation of morphological, magnetic resonance imaging, and operative findings. Neurosurgery 54:1051–1060
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW, Moshang T, Rorke LB, Phillips PC, Sutton LN, Shu HK (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58:714–720
Sutton LN (1994) Vascular complications of surgery for craniopharyngioma and hypothalamic glioma. Pediatr Neurosurg 21(Suppl 1):124–128
Tomita T, McLone DG (1993) Radical resections of childhood craniopharyngiomas. Pediatr Neurosurg 19:6–14
Van Effenterre R, Boch A-L (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Van Effenterre R, Boch AL (1993) Radionecrosis of the optic chiasm. A clinical and radiological study of 3 cases. Neurochirurgie 39:75–84
Villani RM, Tomei G, Bello L, Sganzerla E, Ambrosi B, Re T, Giovanelli Barilari M (1997) Long-term results of treatment for craniopharyngioma in children. Childs Nerv Syst 13:397–405
Wang KC, Kim SK, Choe G, Chi JG, Cho BK (2002) Growth patterns of craniopharyngioma in children: role of the diaphragma sellae and its surgical implication. Surg Neurol 57:25–33
Yasargi MG, Curcic M, Kis S, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Zuccaro G, Jaimovich R, Mantese B et al (1996) Complications in paediatric craniopharyngioma treatment. Childs Nerv Syst 12:385–391
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tomita, T., Bowman, R.M. Craniopharyngiomas in children: surgical experience at Children’s Memorial Hospital. Childs Nerv Syst 21, 729–746 (2005). https://doi.org/10.1007/s00381-005-1202-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-1202-9