Abstract
Purpose
In this review, we will discuss the state of the literature regarding Aquablation, its limitations, and opportunities for its application in the treatment of benign prostatic enlargement (BPE).
Methods
A comprehensive review of original research on Aquablation was conducted. Articles related to transurethral resection of the prostate, holmium laser enucleation of the prostate, greenlight photoselective vaporization of the prostate, and simple prostatectomy were reviewed for discussion.
Results
For small–medium prostates (30–80 mL), Aquablation’s main advantages include better ejaculatory function and similar functional outcomes compared to TURP. For large prostates (80–150 mL), Aquablation demonstrates shorter operative time and superior ejaculatory function when compared to simple prostatectomy, HoLEP, and Greenlight PVP. In addition, Aquablation displays shorter hospital stays than simple prostatectomy. The integration of software programming and semi-automatic technology increases the reproducibility of the procedure and helps standardize overall outcomes, while also accelerating the learning curve. Its ability to preserve antegrade ejaculation makes Aquablation a very compelling option for sexually active patients. However cost and postoperative bleeding risks remain a concern.
Conclusion
The current evidence suggests that Aquablation is a safe and effective alternative for BPE for small to large prostates. Further prospective clinical trials, with comparisons to other BPE modalities, and data from longer follow-up periods are still required.

Similar content being viewed by others
Data availability
All the data from our review can be found in published articles in the references.
References
Lokeshwar SD, Harper BT, Webb E et al (2019) Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl Androl Urol 8:529–539. https://doi.org/10.21037/tau.2019.10.01
Oelke M, Bachmann A, Descazeaud A et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64:118–140. https://doi.org/10.1016/j.eururo.2013.03.004
Foster HE, Dahm P, Kohler TS et al (2019) Surgical Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2019. J Urol 202:592–598. https://doi.org/10.1097/JU.0000000000000319
Rassweiler J, Teber D, Kuntz R, Hofmann R (2006) Complications of transurethral resection of the prostate (TURP)-incidence, management, and prevention. Eur Urol 50:969–979. https://doi.org/10.1016/j.eururo.2005.12.042
Pariser JJ, Packiam VT, Adamsky MA, Bales GT (2016) Trends in simple prostatectomy for benign prostatic hyperplasia. Curr Urol Rep 17:57. https://doi.org/10.1007/s11934-016-0610-6
Desai M, Bidair M, Bhojani N et al (2019) WATER II (80–150 mL) procedural outcomes. BJU Int 123:106–112. https://doi.org/10.1111/bju.14360
Faber K, De Abreu ALC, Ramos P et al (2015) Image-guided robot-assisted prostate ablation using water jet-hydrodissection: initial study of a novel technology for benign prostatic hyperplasia. J Endourol 29:63–69. https://doi.org/10.1089/end.2014.0304
Misrai V, Rijo E, Zorn KC et al (2019) Waterjet ablation therapy for treating benign prostatic obstruction in patients with small- to medium-size glands: 12-month results of the first french aquablation clinical registry. Eur Urol 76:667–675. https://doi.org/10.1016/j.eururo.2019.06.024
Desai MM, Singh A, Abhishek S et al (2018) Aquablation therapy for symptomatic benign prostatic hyperplasia: a single-centre experience in 47 patients. BJU Int 121:945–951. https://doi.org/10.1111/bju.14126
Gilling P, Reuther R, Kahokehr A, Fraundorfer M (2016) Aquablation—Image-guided robot-assisted waterjet ablation of the prostate: Initial clinical experience. BJU Int 116:923–929. https://doi.org/10.1111/bju.13358
Gilling P, Barber N, Bidair M et al (2018) WATER: A Double-blind, randomized, controlled trial of aquablation® vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol 199:1252–1261. https://doi.org/10.1016/j.juro.2017.12.065
Gravas S., Cornu J.N., Gacci M., Gratzke C., Herrmann T.R.W., Mamoulakis C., Rieken M., Speakman M.J. TKAO (2020) EAU guidelines on management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO). https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/. Accessed 25 Mar 2020
Bahls T, Fröhlich FA, Hellings A et al (2017) Extending the capability of using a waterjet in surgical interventions by the use of robotics. IEEE Trans Biomed Eng 64:284–294. https://doi.org/10.1109/TBME.2016.2553720
Bach T, Giannakis I, Bachmann A et al (2019) Aquablation of the prostate: single-center results of a non-selected, consecutive patient cohort. World J Urol 37:1369–1375. https://doi.org/10.1007/s00345-018-2509-y
Zorn KC, Larry Goldenberg S, Paterson R et al (2019) Aquablation among novice users in Canada: a WATER II subpopulation analysis. Can Urol Assoc J 13:E113–E118. https://doi.org/10.5489/cuaj.5501
Brunckhorst O, Ahmed K, Nehikhare O et al (2015) Evaluation of the learning curve for holmium laser enucleation of the prostate using multiple outcome measures. Urology 86:824–829. https://doi.org/10.1016/j.urology.2015.07.021
Kampantais S, Dimopoulos P, Tasleem A et al (2018) Assessing the learning curve of holmium laser enucleation of prostate (HoLEP). Syst Rev Urol 120:9–22. https://doi.org/10.1016/j.urology.2018.06.012
Bastard C, Zorn K, Peyronnet B, Hueber PA, Pradère B, Rouprêt M, M V. (2019) Assessment of learning curves for 180-W GreenLight XPS photoselective vaporisation of the prostate: a multicentre study. Eur Urol Focus 5:266–272. https://doi.org/10.1016/j.euf.2017.09.011
Furuya S, Furuya R, Ogura H et al (2006) A study of 4,031 patients of transurethral resection of the prostate performed by one surgeon: learning curve, surgical results and postoperative complications. Acta Urol Jpn 52:609–614
Nguyen DD, Bhojani N, Zorn KC (2019) Furthering the external validity of Aquablation and implications for real-world patients. World J Urol 37:1983–1984. https://doi.org/10.1007/s00345-018-2610-2
Kasivisvanathan V, Hussain M (2018) Aquablation versus transurethral resection of the prostate: 1 year United States—cohort outcomes. Can J Urol 25:9317–9322
Bach T, Gilling P, El Hajj A et al (2020) First multi-center all-comers study for the Aquablation procedure. J Clin Med 9:603. https://doi.org/10.3390/jcm9020603
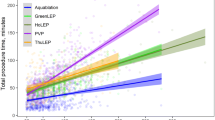
Nguyen D-D, Misraï V, Bach T et al (2020) Operative time comparison of Aquablation, greenlight PVP, ThuLEP, GreenLEP, and HoLEP. World J Urol. https://doi.org/10.1007/s00345-020-03137-8
Bhojani N, Nguyen D-D, Kaufman RPJ et al (2019) Comparison of < 100 cc prostates and > 100 cc prostates undergoing Aquablation for benign prostatic hyperplasia. World J Urol 37:1361–1368. https://doi.org/10.1007/s00345-018-2535-9
Uchida T, Ohori M, Soh S et al (1999) Factors influencing morbidity in patients undergoing transurethral resection of the prostate. Urology 53:98–105. https://doi.org/10.1016/S0090-4295(98)00524-X
Nguyen DD, Barber N, Bidair M et al (2020) Waterjet ablation therapy for endoscopic resection of prostate tissue trial (WATER) vs WATER II: comparing Aquablation therapy for benign prostatic hyperplasia in 30–80 and 80–150 mL prostates. BJU Int 125:112–122. https://doi.org/10.1111/bju.14917
Gilling P, Barber N, Bidair M et al (2020) Three-year outcomes after Aquablation therapy compared to TURP: results from a blinded randomized trial. Can J Urol 27:10072–10079
Yalçın S, Yılmaz S, Gazel E et al (2020) Holmium laser enucleation of the prostate for the treatment of size-independent BPH: a single-center experience of 600 cases. Turkish J Urol 46:219–225. https://doi.org/10.5152/tud.2020.19235
Valdivieso R, Hueber PA, Meskawi M et al (2018) Multicentre international experience of 532-nm laser photoselective vaporization with GreenLight XPS in men with very large prostates. BJU Int 122:873–878. https://doi.org/10.1111/bju.14208
Gilling P, Barber N, Bidair M et al (2019) Two-year outcomes after Aquablation compared to TURP: efficacy and ejaculatory improvements sustained. Adv Ther 36:1326–1336. https://doi.org/10.1007/s12325-019-00952-3
Gilling P, Anderson P, Tan A (2017) Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1-year results. J Urol 197:1565–1572. https://doi.org/10.1016/j.juro.2017.01.056
Desai M, Bidair M, Bhojani N et al (2020) Aquablation for benign prostatic hyperplasia in large prostates (80–150 cc): 2-year results. Can J Urol 27:10147–10153
Bhojani N, Bidair M, Zorn KC et al (2019) Aquablation for benign prostatic hyperplasia in large prostates (80–150 cc): 1-Year Results. Urology 129:1–7. https://doi.org/10.1016/j.urology.2019.04.029
Krambeck AE, Handa SE, Lingeman JE (2010) Experience with more than 1000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol 198:663–670. https://doi.org/10.1016/j.juro.2009.11.034
Rosen RC (2006) Assessment of sexual dysfunction in patients with benign prostatic hyperplasia. BJU Int 97:29–33. https://doi.org/10.1111/j.1464-410X.2006.06103.x
Reale G, Cimino S, Bruno G et al (2019) “Aquabeam® system” for benign prostatic hyperplasia and LUTS: birth of a new era. A systematic review of functional and sexual outcome and adverse events of the technique. Int J Impot Res 31:392–399. https://doi.org/10.1038/s41443-019-0158-3
Suarez-Ibarrola R, Bach T, Hein S et al (2019) Efficacy and safety of Aquablation of the prostate for patients with symptomatic benign prostatic enlargement: a systematic review. World J Urol 38:1147–1163. https://doi.org/10.1007/s00345-019-02959-5
Rosen RC, Riley A, Wagner G et al (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830. https://doi.org/10.1016/S0090-4295(97)00238-0
Rosen RC, Catania J, Pollack L et al (2004) Male sexual health questionnaire (MSHQ): scale development and psychometric validation. Urology 64:777–782. https://doi.org/10.1016/j.urology.2004.04.056
Sturch P, Woo HH, McNicholas T, Muir G (2015) Ejaculatory dysfunction after treatment for lower urinary tract symptoms: retrograde ejaculation or retrograde thinking? BJU Int 115:186–187. https://doi.org/10.1111/bju.12868
Bachmann A, Tubaro A, Barber N et al (2014) 180-W XPS greenlight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European multicentre randomised trial - The GOLIATH study. Eur Urol 65:931–942. https://doi.org/10.1016/j.eururo.2013.10.040
Marra G, Sturch P, Oderda M et al (2016) Systematic review of lower urinary tract symptoms/benign prostatic hyperplasia surgical treatments on men’s ejaculatory function: time for a bespoke approach? Int J Urol 23:22–35. https://doi.org/10.1111/iju.12866
Elterman D, Bach T, Rijo E et al (2020) Transfusion rates after 800 Aquablation procedures using various haemostasis methods. BJU Int 125:568–572. https://doi.org/10.1111/bju.14990
Pariser JJ, Pearce SM, Patel SG, Bales GT (2015) National trends of simple prostatectomy for benign prostatic hyperplasia with an analysis of risk factors for adverse perioperative outcomes. Urology 86:721–725. https://doi.org/10.1016/j.urology.2015.06.048
Gratzke C, Schlenker B, Seitz M et al (2007) Complications and early postoperative outcome after open prostatectomy in patients with benign prostatic enlargement: results of a prospective multicenter study. J Urol 177:1419–1422. https://doi.org/10.1016/j.juro.2006.11.062
Zheng X, Peng L, Cao D et al (2019) Holmium laser enucleation of the prostate in benign prostate hyperplasia patients with or without oral antithrombotic drugs: a meta-analysis. Int Urol Nephrol 51:2127–2136. https://doi.org/10.1007/s11255-019-02278-z
Misraï V, Pasquie M, Bordier B et al (2018) Comparison between open simple prostatectomy and green laser enucleation of the prostate for treating large benign prostatic hyperplasia: a single-centre experience. World J Urol 36:793–799. https://doi.org/10.1007/s00345-018-2192-z
Mebust WK, Holtgrewe HL, Cockett ATK et al (2002) Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol 167:5–9. https://doi.org/10.1016/S0022-5347(05)65370-0
Lerner LB, Tyson MD, Mendoza PJ (2010) Stress incontinence during the learning curve of holmium laser enucleation of the prostate. J Endourol 24:1655–1658. https://doi.org/10.1089/end.2010.0021
Tubaro A, Carter S, Hind A et al (2001) A prospective study of the safety and efficacy of suprapubic transvesical prostatectomy in patients with benign prostatic hyperplasia. J Urol 166:172–176. https://doi.org/10.1016/S0022-5347(05)66102-2
Serretta V, Morgia G, Fondacaro L et al (1990s) Open prostatectomy for benign prostatic enlargement in southern Europe in the late 1990s: a contemporary series of 1800 interventions. Urology 60:623–627. https://doi.org/10.1016/S0090-4295(02)01860-5
Vavassori I, Valenti S, Naspro R et al (2008) Three-year outcome following holmium laser enucleation of the prostate combined with mechanical morcellation in 330 consecutive patients. Eur Urol 53:599–604. https://doi.org/10.1016/j.eururo.2007.10.059
Elmansy HM, Kotb A, Elhilali MM (2011) Is there a way to predict stress urinary incontinence after holmium laser enucleation of the prostate? J Urol 186:1977–1981. https://doi.org/10.1016/j.juro.2011.06.063
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The literature search, data analysis, and draft were done by IS. All the authors were involved in the revision/critical appraisal of the paper.
Corresponding author
Ethics declarations
Conflict of interest
Kevin C. Zorn: Consultant, Investigator (Procept BioRobotics). Dean Elterman: Consultant, Investigator (Procept BioRobotics). Enrique Rijo: Consultant, Investigator (Procept BioRobotics). Thorsten Bach: Consultant, Investigator (Procept BioRobotics). Kevin C. Zorn, Dean Elterman, Enrique Rijo, and Thorsten Bach are consultants and investigators for Procept BioRobotics. Iman Sadri, Adel Arezki, Félix Couture, Ahmed S. Zakaria, David-Dan Nguyen have nothing to disclose.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sadri, I., Arezki, A., Couture, F. et al. Reasons to overthrow TURP: bring on Aquablation. World J Urol 39, 2291–2299 (2021). https://doi.org/10.1007/s00345-020-03390-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03390-x