Abstract
Objectives
We aimed to assess undergraduate medical students’ knowledge, attitude, and perception regarding artificial intelligence (AI) in medicine.
Methods
A multi-national, multi-center cross-sectional study was conducted from March to April 2022, targeting undergraduate medical students in nine Arab countries. The study utilized a web-based questionnaire, with data collection carried out with the help of national leaders and local collaborators. Logistic regression analysis was performed to identify predictors of knowledge, attitude, and perception among the participants. Additionally, cluster analysis was employed to identify shared patterns within their responses.
Results
Of the 4492 students surveyed, 92.4% had not received formal AI training. Regarding AI and deep learning (DL), 87.1% exhibited a low level of knowledge. Most students (84.9%) believed AI would revolutionize medicine and radiology, with 48.9% agreeing that it could reduce the need for radiologists. Students with high/moderate AI knowledge and training had higher odds of agreeing to endorse AI replacing radiologists, reducing their numbers, and being less likely to consider radiology as a career compared to those with low knowledge/no AI training. Additionally, the majority agreed that AI would aid in the automated detection and diagnosis of pathologies.
Conclusions
Arab medical students exhibit a notable deficit in their knowledge and training pertaining to AI. Despite this, they hold a positive perception of AI implementation in medicine and radiology, demonstrating a clear understanding of its significance for the healthcare system and medical curriculum.
Clinical relevance statement
This study highlights the need for widespread education and training in artificial intelligence for Arab medical students, indicating its significance for healthcare systems and medical curricula.
Key Points
• Arab medical students demonstrate a significant knowledge and training gap when it comes to using AI in the fields of medicine and radiology.
• Arab medical students recognize the importance of integrating AI into the medical curriculum. Students with a deeper understanding of AI were more likely to agree that all medical students should receive AI education. However, those with previous AI training were less supportive of this idea.
• Students with moderate/high AI knowledge and training displayed increased odds of agreeing that AI has the potential to replace radiologists, reduce the demand for their services, and were less inclined to pursue a career in radiology, when compared to students with low knowledge/no AI training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Artificial intelligence (AI) is a field of computer science that mimics human intelligence in learning and solving problems. One subfield of AI, machine learning (ML), focuses on developing algorithms capable of improving accuracy through pattern recognition and data analysis [1,2,3]. Deep learning (DL), which falls under the umbrella of ML, has garnered significant attention in the healthcare sector. DL utilizes artificial neural networks to process and analyze large volumes of data, making it especially valuable for image processing, analysis, and even aiding in robotic surgeries [4, 5]. In the medical field, AI research encompasses a broad spectrum of applications. This includes collecting and interpreting healthcare data, imaging techniques, and extending AI’s capabilities to therapeutic and surgical approaches. Additionally, AI plays a vital role in providing timely warnings to patients and healthcare professionals when necessary [6].
The application of AI in radiology has significant implications, as FDA-approved AI-based algorithms have demonstrated remarkable accuracy in detecting specific diseases, comparable to human experts in terms of specificity and sensitivity [7]. However, the rapid technological advancements enabling the growth of AI have sparked discussions surrounding the future of diagnostic and interventional radiology, giving rise to concerns about the potential impact on the practice’s long-term viability [8]. Over the past decade, AI and ML have been the subject of intense debate within the field of radiology, as evidenced by the publication of more than 5000 articles between 2018 and 2023, according to a search conducted on PubMed as of March 25, 2023.
Consequently, these technological advancements have generated a substantial knowledge base and diverse perspectives on AI’s role in medicine. Surveys have revealed that radiologists’ attitudes towards AI range from enthusiastic acceptance to skepticism, primarily driven by fears of being displaced by technology [9, 10]. Notably, the popularity of radiology as a career choice among medical graduates in the USA has declined since the 1990s [11, 12]. Contrary to concerns about replacement, the European Society of Radiology asserts that AI will not replace radiologists but rather enhance their value and improve the field as a whole [13]. In response, radiologists must proactively learn about AI and its applications and collaborate with AI researchers to optimize patient care. Furthermore, the impact of AI extends beyond radiology and will similarly influence other healthcare professions, including pathology, cardiology, and others [13, 14].
Given the recent advancements in AI within the healthcare system, it is increasingly evident that doctors and medical students require comprehensive education in AI. Consequently, raising awareness of AI among future healthcare professionals is crucial to guide their career choices. This topic has received significant attention in Europe, Canada, and the USA; however, it remains relatively understudied in the Middle East and Arab countries. Limited information is available regarding Arab medical students’ awareness and perspectives towards AI and DL in medicine and radiology, as well as the factors influencing their knowledge and attitudes, such as demographics, academic performance, technological proficiency, and previous AI training. Furthermore, it is crucial to investigate their opinions regarding integrating AI into medical school curricula and explore potential differences between Arab and foreign medical students’ attitudes and perceptions.
We aimed to evaluate students’ knowledge, attitude, and perception concerning the utilization of AI in medicine, with a specific focus on its application in radiology. Furthermore, we sought to identify variations in perceptions and attitudes among different student groups. Through this investigation, we aimed to gain insights into the thoughts and sentiments of these students regarding AI in medicine, as well as to determine the potential utility of incorporating the study of AI applications as a compulsory component within their educational curriculum.
Methods
Design
We conducted a multi-national, multi-center cross-sectional study among undergraduate medical students in nine countries in the Middle East and North Africa (MENA) region (Libya, Egypt, Iraq, Jordan, Syria, Sudan, Algeria, Palestine, and Yemen) between March 1, 2022, and April 13, 2022, using an online self-administered questionnaire. All undergraduate students were included. There were no exclusion criteria regarding age or gender. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Checklist was followed in the conduct and reporting of the current article.
Sampling
We adopted the convenience sampling method in our study. The Raosoft sample size calculator was used to estimate the sample size [15]. With a 5% margin of error, a 95% confidence level, and a 50% response distribution (according to a study in Saudi Arabia which found that approximately 50% of the students believed they had a good understanding of AI; however, when knowledge of AI was tested, only 22% of the questions were answered correctly [16]), the sample size was calculated to be at least 382 students per country.
Questionnaire development and validation
The questionnaire was developed using frequently asked questions from previously published national surveys in Canada, the UK, Croatia, the USA, and Germany [17,18,19,20,21]. Experts in the fields of AI and radiology revised each question in terms of relevance, comprehensiveness, and clarity, and some details were improved according to their comments. The questionnaire was translated into Arabic by two bilingual translators, and then the Arabic version was translated back into English by two different translators. The new English version was compared to the original one until a final version was agreed upon. The questionnaire was distributed in both languages; each participant could select his/her preferred language. We also conducted a pilot sampling for both Arabic and English versions with a total of 265 responses that were not included in the analysis to assess Cronbach’s alpha for each domain of the questionnaire.
The questionnaire included four sections:
-
1.
Socio-demographic data: including gender, country, residence (urban/rural), university, grade, and if they are proficient in using modern technology.
-
2.
Knowledge about AI and DL: consisted of 10 questions about the basic principles of AI, its limitations, and whether they are familiar with the terminology related to AI. Cronbach’s alpha for this section was 0.75.
-
3.
Attitudes towards AI and DL: consisted of 18 questions assessing their feelings and perspectives towards AI and DL in medicine and radiology. Cronbach’s alpha for this section was 0.81.
-
4.
Perception regarding AI: consisted of four questions: one assessing whether they accept working alongside AI in a certain clinical workflow, and three asking about AI’s potential applications in radiology practice. Cronbach’s alpha for this section was 0.66.
Finally, four more questions were added. One about which specialties students think would be impacted the earliest and the most by AI, and another three questions about whether they had AI training.
The confirmatory factor analysis model demonstrated an acceptable fit for the data. The model was tested against a baseline model, which revealed a statistically significant difference between the two models. The comparative fit index (CFI) and Tucker-Lewis index (TLI) values were 0.460 and 0.417, respectively, suggesting adequate model fit. The root mean square error of approximation (RMSEA) was 0.123, with a 90% confidence interval between 0.118 and 0.129, indicating a reasonable fit. The loading factors for all three sections of the questionnaire are demonstrated in Table S1 (Supplementary material).
The Arabic and English versions of the questionnaire are illustrated in the Supplementary material.
Data collection
To ensure the quality of the data collection process, we designated a national leader responsible for their country’s data collection process and obtaining ethical approval. We taught them about the nature of the study and the data collection strategy. Each national leader recruited two to five collaborators between January 1, 2022, and February 10, 2022, to help collect the required sample.
Online Google Forms were used for data collection. There were no duplicates since each respondent was only permitted to fill out the questionnaire once via activating the limit to one response option in the settings list, where you can only answer the survey through your email once. Data from the online questionnaires were automatically collected and kept in an Excel spreadsheet. Each collaborator could only access their replies; however, the central investigator could access all responses throughout the country. Arabic answers were translated into English and merged with the English responses in a single Excel spreadsheet for analysis.
Ethical considerations
We obtained ethical approval from the Ethics Committee in six countries before starting the data collection process. In addition, written consent was obtained from the participants after a detailed explanation of the study before filling out the questionnaire, emphasizing their confidentiality and the complete preservation of their data.
Data analysis
Descriptive statistics and regression analyses were performed using R Statistical Software (v4.1.3; R Core Team 2022). Simple descriptive statistics were used to represent the attitude and perceptions of the students using frequencies with percentages. The knowledge section was rated as high (>80% correct answers), moderate (60 to 80% correct answers), and low knowledge level (<60% correct answers). Univariate and multivariate logistic regression analyses were used to assess students’ knowledge, attitude, and perception predictors (demographics including gender, grade, university, place of living, technology experience, and previous AI training). We also used the Hosmer–Lemeshow test to assess the goodness of fit for the regression models.
K-means cluster analyses were performed using Python 3.10.6 to find the patterns of students’ attitudes and perceptions and to see which participants have which kind of perspectives. We standardized the variables using the StandardScaler function, which modifies the data distribution to have a mean of 0 and a standard deviation of 1. This step ensured that each variable had equal weight in the clustering process. The optimal number of clusters was determined using the silhouette score method, which evaluates the clustering quality based on the similarity of objects within a cluster and the dissimilarity between clusters. The higher the score, the better fit the cluster analysis. A chi-square p value was used to assess the statistical significance of the variables in the clusters.
Results
Demographic data
The study sample comprised 4492 medical students from nine countries. In all countries except Yemen, females outnumbered males, with 2768 (61.6%) female participants. Most participants studied in public universities (n = 3877, 86.3%) and lived in urban zones (n = 3486, 77.6%). About 19.2% of the participants (n = 864) were in their third year at medical school. Furthermore, 1784 participants (39.7%) consider themselves neutral regarding tech-savviness. The demographics of the included participants are shown in Table 1.
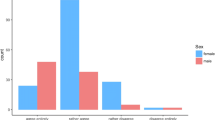
Knowledge
Most students (n = 3914, 87.1%) had a low level of knowledge regarding AI. Moreover, 479 students (10.6%) and 99 students (2.2%) had moderate and high levels of knowledge, respectively. 83.7% of the students (n = 3762) had a low level of knowledge regarding DL. Sudan had the highest percentage of students (n = 440, 92.8%) with a low knowledge of basic AI computational principles, terminology, limitations, and DL. In contrast, the highest number of students with a high level of knowledge was reported among Syrians (n = 23, 4.8%), as shown in Fig. 1.
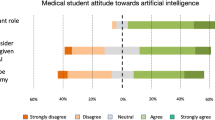
Attitude
Artificial intelligence and deep learning
Concerning the feelings and attitudes towards AI and DL in medicine and radiology, 1958 participants strongly agree that AI will revolutionize radiology (43.6%). Moreover, 1593 responses were neutral concerning human radiologist replacement in the future (35.5%); meanwhile, 1620 students (36.1%) agreed that it would reduce the number of needed radiologists. 38.7% of the responses (n = 1738) were neutral regarding students’ likelihood of considering a career in radiology given the advancement of AI (Table S2, Supplementary material).
Artificial intelligence and medical curriculum
The majority of participants strongly agreed that all medical students should receive teaching in AI (n = 1950, 43.4%) and that it will be beneficial for their career (n = 1850, 41.2%), as shown in Table S3 (Supplementary material).
Artificial intelligence training
92.4% of participants (n = 4152) received no teaching or training in AI. Only 142 students (41.8%) of those who received the training received it as part of their curriculum, and 111 (32.6%) of those who received the training rated their satisfaction to be 3 out of 5 (neutral).
Specialties affected by artificial intelligence
Diagnostic radiology was reported to be the most affected specialty at the early stages of developing AI applications (n = 2214, 49.3%), followed by surgery and oncology, as shown in Fig. 2.
Regression analysis
Knowledge levels (high/moderate vs. low)
The multivariate logistic regression analysis showed that students studying in a private university (adjusted odds ratio (AOR): 1.55; 95%CI: 1.18–2.03; p = 0.001), being neutral (AOR: 3.45; 95%CI: 1.87–7.11; p < 0.001), “agreed” (AOR: 10.14; 95%CI: 5.53–20.89; p < 0.001) or “strongly agreed” (AOR: 25.17; 95%CI: 13.52–52.35; p < 0.001) that they were tech-savvy, and having AI training (AOR: 7.63; 95%CI: 5.86–9.94; p < 0.001) were found to be independently associated with increased odds of getting a high/moderate level of knowledge (Table 2). The test statistic of the Hosmer–Lemeshow test was − 30,930 with 8 degrees of freedom, and the p value was greater than 0.5, indicating a good fit for the model.
Attitude and perception
We observed that students with high/moderate AI knowledge and training were associated with increased odds of strongly agreeing/agreeing that AI will replace radiologists (AOR = 1.69; 95%CI: 1.35–2.12; p < 0.001, AOR = 2.81; 95%CI: 2.12–3.76; p < 0.001, respectively) and reduce the number of needed radiologists (AOR = 1.35; 95%CI: 1.05–1.75; p = 0.023, AOR = 1.36; 95%CI: 0.97–1.94; p = 0.076, respectively) compared to students having low knowledge and no AI training. Similarly, having high/moderate AI knowledge and training were found to be associated with higher odds of agreeing (strongly agree or agree) that students were less likely to consider pursuing a career in radiology (AOR = 1.77; 95%CI: 1.33–2.36; p < 0.001, AOR = 1.52; 95%CI: 1.21–1.90; p < 0.001, respectively).
Furthermore, our study revealed that clinical year medical students (4th, 5th, 6th year, and interns) were independently associated with lower odds of agreeing (strongly agree or agree) that AI will replace radiologists in the future (AOR = 0.83; 95%CI: 0.72–0.97; p = 0.021) compared to academic years students (from 1st to 3rd grade).
On the other hand, our study found that having high/moderate AI knowledge was independently associated with higher odds of strongly agreeing or agreeing that all medical students should receive AI training or teaching (AOR = 2.09; 1.46–3.08; p < 0.001). However, students who obtained previous AI training were associated with lower odds of agreeing (strongly agree or agree) with that suggestion (AOR = 0.44; 95%CI: 0.31–0.63, p < 0.001) compared to untrained subjects.
The p value for the Hosmer–Lemeshow tests for all these regression models was greater than 0.5, indicating a good fit for the model.
Cluster analysis
Through confirmatory factor analysis and Cronbach alpha’s results, our questionnaire was structured into three distinct sections: knowledge (9 variables), attitude (18 variables), and perception (4 variables). A detailed breakdown of these sections can be found in Table S1 of the Supplementary material. Furthermore, the attitude section was further divided into two subsections: AI and DL attitude (13 variables) and AI and medical curriculum attitude (5 variables). We performed three rounds of K-means cluster analysis on all these sections except the knowledge section to assess the patterns of students’ attitudes and perceptions regarding AI. In our cluster analyses, we used silhouette scores as a guide to determine the optimal number of clusters for each analysis. It happened that the silhouette score indicated two clusters as the optimal choice in all three of our cluster analyses. We did not force two clusters; rather, we selected this number based on the highest silhouette score, which indicates a better fit for the analysis.
Artificial intelligence and deep learning attitude
Cluster analysis using the K-means method was conducted on the section pertaining to attitudes towards AI and DL, encompassing 13 variables. The analysis resulted in the identification of two distinct clusters, as presented in Table 3, with a silhouette score of 0.325. The selection of these variables was based on their demonstrated relevance in capturing participants’ sentiments and attitudes towards the integration of AI and DL in medicine and radiology, as previously determined through factor analysis. Through an examination of these variables, our aim was to delve into the participants’ attitudes and emotional responses towards AI and gain a comprehensive understanding of the diverse perspectives within the studied population.
Cluster 1 comprised 3818 students, the majority of whom expressed agreement with the transformative potential of AI in medicine and radiology, finding these advancements to be exciting. However, they also acknowledged apprehension towards AI progress and its potential impact on the need for radiologists, expressing concerns about a decrease in demand. Additionally, cluster 1 participants disagreed with the notion of entirely replacing physicians and radiologists and, instead, showed a greater inclination towards considering a career in radiology.
In contrast, cluster 2 consisted of 674 participants, who similarly acknowledged the potential revolution that AI could bring to medicine and radiology. However, their perspectives were more neutral when it came to the replacement of radiologists and physicians by AI, their personal fears surrounding AI, their interest in pursuing a career in radiology, and the potential decrease in the number of radiologists due to AI.
Notably, cluster 1 displayed a higher level of technological proficiency, possessing more comprehensive knowledge and training in AI compared to cluster 2. No significant variations were observed between the two clusters in terms of gender, university affiliation, academic grade, or residential location.
Artificial intelligence and medical curriculum attitude
For the analysis of the AI and medical curriculum attitude section, five relevant variables were employed in the K-means cluster analysis. This analysis generated two distinct clusters, as displayed in Table 4, with a silhouette score of 0.42. The selection of these variables was guided by their demonstrated relevance in evaluating students’ attitudes and perceptions regarding the incorporation of AI into the medical curriculum, as determined through previous factor analysis. By exploring these variables, our objective was to gain valuable insights into the students’ viewpoints concerning the integration of AI within the medical curriculum and their preparedness to engage with AI technologies.
Cluster 1 comprised 3084 participants, who demonstrated a higher level of AI knowledge, technological proficiency (tech-savviness), and experience compared to cluster 2 (n = 1408). Both clusters exhibited agreement regarding the importance of incorporating AI education into the medical curriculum, recognizing its potential benefits for their future careers. However, cluster 1 students predominantly expressed confidence, understanding, and knowledge pertaining to the utilization of fundamental AI tools and methods in healthcare, while cluster 2 students maintained a neutral stance on these aspects.
Notably, no significant variations were observed between the two clusters in terms of gender distribution, university affiliation, academic grade, residential location, or AI training.
Perception
To investigate the perception of medical students towards the integration of AI in radiology, a K-means cluster analysis was conducted on the perception section, utilizing four pertinent variables. The analysis yielded two distinct clusters, as depicted in Table 5, with a silhouette score of 0.5. These variables were selected based on their demonstrated relevance in capturing the perceptions of medical students regarding the integration of AI in radiology, as determined by prior factor analysis. By examining these variables, our aim was to explore the students’ perspectives on the potential applications and benefits of AI in radiology, as well as their willingness to embrace AI technologies.
Cluster 1 encompassed 3536 students, the majority of whom expressed agreement with the notion of working collaboratively with AI in a specific workflow, involving a review of both medical images and AI-generated findings subsequent to the initial AI analysis. They also acknowledged the potential applications of AI in detecting and diagnosing pathologies, as well as appropriate indications for imaging examinations. In contrast, cluster 2 (n = 956) exhibited predominantly neutral responses to these questions.
Cluster 1 comprised a larger proportion of students with advanced AI knowledge, training, and technological experience (tech-savviness) compared to cluster 2. No significant differences were observed between the two clusters in terms of gender distribution, university affiliation, academic grade, or residential location.
Discussion
Our findings revealed a concerning lack of knowledge regarding AI and DL among the majority of students. This inadequacy is notably higher compared to findings from previous studies. For instance, a study conducted by Santos et al in Germany reported that 52% of students were aware of the ongoing discussion surrounding the utilization of AI in radiology, with 68% indicating their lack of awareness regarding the underlying technologies [18]. Similarly, a study conducted in Saudi Arabia found that approximately 50% of students believed they possessed a good understanding of AI, but when tested on their knowledge, only 22% answered the questions correctly [16]. Furthermore, a study conducted in Brazil demonstrated that 64.3% of students claimed to lack sufficient knowledge regarding the new advancements in AI technologies [22].
The transformative potential of AI in various medical disciplines, including radiology, is already widely recognized. Consistent with this recognition, the majority of students in our cohort expressed agreement with the notion that AI will exert a substantial impact on healthcare. Correspondingly, a study conducted in the UK reported that 88% of students shared the belief that AI would play a crucial role in the realm of healthcare [19]. Moreover, findings from another study indicated that radiologists themselves anticipate significant changes within the radiology field due to AI within a decade, envisioning its potential roles as a secondary reader and workflow optimizer [23].
However, despite the existence of compelling arguments to the contrary, radiologists continue to harbor significant concerns regarding potential career displacement resulting from further AI integration in the medical field [24]. Our study aimed to investigate the attitudes of Arab students towards AI in medicine and radiology, leading to the identification of two distinct clusters. The larger and more knowledgeable cluster expressed apprehension towards AI advancements and held the belief that AI would lead to a decrease in the demand for radiologists. However, they were predominantly opposed to the complete replacement of radiologists by AI and expressed a continued interest in pursuing a career in radiology. In a study conducted in Saudi Arabia by Bin Dahmash et al [16] among participants who ranked radiology as their first, second, or third career choice, 52% disagreed with the notion of radiologists being replaced during their lifetime, while 44.8% agreed that AI would reduce the number of radiologists needed in the future. Gong et al [17] reported that 67.7% of students believed that AI would diminish the demand for radiologists in the future, yet 58.6% disputed the notion of AI replacing radiologists entirely. Furthermore, research conducted on German medical students by Santos et al [18] revealed that 82.9% of participants did not foresee AI eventually replacing radiologists. Additionally, a study investigating the perception, knowledge, and attitude of radiologists and radiology residents towards AI found that 48% displayed an open and proactive attitude towards AI, while 38% expressed fear regarding potential replacement by AI [25].
Our findings indicate that the influence of AI advancements is perceived more negatively by Arab medical students considering a career in radiology compared to their counterparts in the UK [19], Canada [17], and Germany [18]. Furthermore, our regression analysis revealed a noteworthy association between Arab students possessing moderate/high levels of AI knowledge and training and their increased likelihood of agreeing that AI will replace radiologists, reduce the number of required radiologists, and diminish their interest in pursuing a career in radiology when compared to students with low knowledge and no AI training. This observation suggests a potential misunderstanding among these students, highlighting the need for clarification.
Several studies [24, 26, 27] have addressed this concern, demonstrating that AI does not aim to replace radiologists but rather facilitates their work, emphasizing the importance of adhering to established rules and principles to ensure optimal patient outcomes. It is crucial to acknowledge that the role of radiologists extends beyond image interpretation, encompassing collaboration with other physicians in diagnosis and treatment, management of illnesses, performance of image-guided medical interventions (interventional radiology), and various other tasks [25]. Furthermore, it is plausible to attribute this misunderstanding among Arab students to the phenomenon known as the initial overconfidence effect. This effect occurs when individuals possess limited knowledge in a new domain, leading them to develop an unwarranted sense of confidence in their understanding [28]. In our study, the majority of participants had a relatively low level of AI knowledge. However, even those with a somewhat higher level of knowledge may still have encountered limitations due to the aforementioned overconfidence effect. Consequently, this may explain why these students continue to express concerns and fear regarding AI advancements in the field of radiology.
Most participants in our research expressed agreement regarding the necessity of providing comprehensive education in AI to all medical students. Through our analysis, we identified two distinct clusters of responses pertaining to AI and its integration into the medical curriculum. Both clusters shared the viewpoint that AI education is essential and holds significant benefits for the future careers of medical students. However, the larger and more knowledgeable cluster demonstrated a stronger consensus regarding their confidence, understanding, and knowledge surrounding the use of fundamental AI tools in healthcare. These findings are in line with previous studies conducted in the UK, where 89% of medical students believed that incorporating AI education into their curriculum would be advantageous to their careers, with 78% supporting the inclusion of AI training as part of their medical degree [19]. Similarly, a study conducted in Croatia revealed that 89.6% of radiologists and radiology residents supported the integration of AI into medical education and curricula, underscoring the perceived importance of AI adoption within the medical field [21]. Additional research focusing on radiologists and radiology residents demonstrated a strong consensus among them, indicating that AI should be incorporated into residency programs and radiology curricula [23]. However, our research revealed that students who had received prior AI training were less inclined to agree with the suggestion of integrating AI education for all medical students, in contrast to their untrained counterparts. This observation suggests that these trained students, who were exposed to AI tools, may have gained a deeper appreciation for the complexity and challenges associated with these intelligent systems. Consequently, they expressed reservations about widespread AI education, recognizing the intricacies involved despite acknowledging the utility and potential of these technologies.
Our study revealed a predominantly positive perception of AI applications in radiology among Arab students. Specifically, cluster 1, which consisted of a larger group of knowledgeable and trained students in AI, exhibited a stronger agreement towards working alongside AI and recognized the potential benefits of AI in detecting and diagnosing pathologies and appropriate indications in imaging exams. These findings align with a study conducted by Santos et al [18], in which 30 to 43.4% of German students “rather agreed” with the same concept.
More than 92% of the participants reported no prior training in AI, and over 80% had low knowledge in this area. As a result, the validity of their perspectives and attitudes regarding the impact of AI on various healthcare issues may be limited. This underscores a critical point in our data, potentially affecting their representativeness. It is plausible that the opinions of these students regarding AI are shaped by their limited knowledge and understanding.
Furthermore, our regression analysis demonstrated that students studying in private universities, those who exhibited greater proficiency in using modern technology, and those who had received prior AI training were more likely to possess a high/moderate level of AI and DL knowledge. This observation highlights the importance of incorporating AI into medical curricula, particularly in public universities where students often exhibit lower levels of knowledge. By introducing AI into their education, students will have increased exposure to computers and AI tools, enhancing their proficiency in using modern technology and fostering AI literacy among them.
Strengths and limitations
To our knowledge, this study represents the first comprehensive multi-national investigation of medical students’ knowledge, attitude, and perception regarding AI within the MENA region. Including data from nine Arab countries has allowed for a more extensive assessment of the current landscape. Nevertheless, we acknowledge some limitations to our study, including the use of convenience sampling, which may introduce selection bias and hinder the establishment of causal relationships between the examined independent and dependent variables inherent to the cross-sectional design. Therefore, we encourage future investigations to adopt a longitudinal study design to better elucidate these relationships.
Conclusion
Arab medical students have considerably poor knowledge and training regarding the use of AI in medicine and radiology. However, they acknowledge AI’s importance for the healthcare system and medical curriculum and have a positive perception towards AI. These findings raise a significant concern that must be addressed immediately to ensure the up-to-date use and practice of modern technology in the medical field.
Abbreviations
- AI:
-
Artificial intelligence
- AOR:
-
Adjusted odds ratio
- DL:
-
Deep learning
- FDA:
-
Food and Drug Administration
- MENA:
-
Middle East and North Africa
- ML:
-
Machine learning
- OR:
-
Odds ratio
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- UK:
-
United Kingdom
References
Martín Noguerol T, Paulano-Godino F, Martín-Valdivia MT et al (2019) Strengths, weaknesses, opportunities, and threats analysis of artificial intelligence and machine learning applications in radiology. J Am Coll Radiol 16:1239–1247. https://doi.org/10.1016/J.JACR.2019.05.047
Nichols JA, Herbert Chan HW, Baker MAB (2019) Machine learning: applications of artificial intelligence to imaging and diagnosis. Biophys Rev 11:111–118. https://doi.org/10.1007/s12551-018-0449-9
Janiesch C, Zschech P, Heinrich K (2021) Machine learning and deep learning. Electron Mark 31:685–695. https://doi.org/10.1007/s12525-021-00475-2
Lee JG, Jun S, Cho YW et al (2017) Deep learning in medical imaging: general overview. Korean J Radiol 18:570–584. https://doi.org/10.3348/KJR.2017.18.4.570
Egger J, Gsaxner C, Pepe A et al (2022) Medical deep learning-a systematic meta-review. Comput Methods Programs Biomed 221:106874. https://doi.org/10.1016/j.cmpb.2022.106874
Wartman SA, Combs CD (2019) Reimagining medical education in the age of AI. AMA J ethics 21:E146-152. https://doi.org/10.1001/amajethics.2019.146
Topol EJ (2019) High-performance medicine: the convergence of human and artificial intelligence. Nat Med 25:44–56. https://doi.org/10.1038/s41591-018-0300-7
Auloge P, Garnon J, Robinson JM et al (2020) Interventional radiology and artificial intelligence in radiology: is it time to enhance the vision of our medical students? Insights Imaging 11:127. https://doi.org/10.1186/s13244-020-00942-y
European Society of Radiology (ESR) (2019) Impact of artificial intelligence on radiology: a EuroAIM survey among members of the European Society of Radiology. Insights Imaging 10:105. https://doi.org/10.1186/s13244-019-0798-3
Pakdemirli E (2019) Perception of artificial intelligence (AI) among radiologists. Acta Radiol Open 8:205846011987866. https://doi.org/10.1177/2058460119878662
Chockley K, Emanuel E (2016) The end of radiology? Three threats to the future practice of radiology. J Am Coll Radiol 13:1415–1420. https://doi.org/10.1016/J.JACR.2016.07.010
Chen JY, Heller MT (2014) How competitive is the match for radiology residency? Present view and historical perspective. J Am Coll Radiol 11:501–506. https://doi.org/10.1016/J.JACR.2013.11.011
Neri E, de Souza N, Brady A et al (2019) What the radiologist should know about artificial intelligence – an ESR white paper. Insights Imaging 10. https://doi.org/10.1186/S13244-019-0738-2
Hricak H (2018) 2016 New Horizons Lecture: beyond imaging—radiology of tomorrow. Radiology 286:764–775. https://doi.org/10.1148/radiol.2017171503
Raosoft.com (2016) Sample size calculator by Raosoft , Inc . In: Online. http://www.raosoft.com/samplesize.html. Accessed 5 Feb 2020
Bin Dahmash A, Alabdulkareem M, Alfutais A et al (2020) Artificial intelligence in radiology: does it impact medical students preference for radiology as their future career? BJR|Open 2:20200037. https://doi.org/10.1259/bjro.20200037
Gong B, Nugent JP, Guest W et al (2019) Influence of artificial intelligence on Canadian medical students’ preference for radiology specialty: a national survey study. Acad Radiol 26:566–577. https://doi.org/10.1016/J.ACRA.2018.10.007
Pinto Dos Santos D, Giese D, Brodehl S et al (2019) Medical students’ attitude towards artificial intelligence: a multicentre survey. Eur Radiol 29:1640–1646. https://doi.org/10.1007/s00330-018-5601-1
Sit C, Srinivasan R, Amlani A et al (2020) Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging 11:14. https://doi.org/10.1186/s13244-019-0830-7
Park CJ, Yi PH, Siegel EL (2021) Medical student perspectives on the impact of artificial intelligence on the practice of medicine. Curr Probl Diagn Radiol 50:614–619. https://doi.org/10.1067/j.cpradiol.2020.06.011
Dumić-Čule I, Orešković T, Brkljačić B et al (2020) The importance of introducing artificial intelligence to the medical curriculum - assessing practitioners’ perspectives. Croat Med J 61:457–464. https://doi.org/10.3325/cmj.2020.61.457
Brandes GIG, D’Ippolito G, Azzolini AG, Meirelles G (2020) Impact of artificial intelligence on the choice of radiology as a specialty by medical students from the city of São Paulo. Radiol Bras 53:167–170. https://doi.org/10.1590/0100-3984.2019.0101
Huisman M, Ranschaert E, Parker W et al (2021) An international survey on AI in radiology in 1041 radiologists and radiology residents. Part 2: Expectations, hurdles to implementation, and education. Eur Radiol 31:8797–8806. https://doi.org/10.1007/s00330-021-07782-4
European Society of Radiology (ESR) (2019) What the radiologist should know about artificial intelligence - an ESR white paper. Insights Imaging 10:44. https://doi.org/10.1186/s13244-019-0738-2
Huisman M, Ranschaert E, Parker W et al (2021) An international survey on AI in radiology in 1,041 radiologists and radiology residents. Part 1: Fear of replacement, knowledge, and attitude. Eur Radiol 31:7058–7066. https://doi.org/10.1007/s00330-021-07781-5
Pesapane F, Codari M, Sardanelli F (2018) Artificial intelligence in medical imaging: threat or opportunity? Radiologists again at the forefront of innovation in medicine. Eur Radiol Exp 2:35. https://doi.org/10.1186/s41747-018-0061-6
Kohli M, Geis R (2018) Ethics, artificial intelligence, and radiology. J Am Coll Radiol 15:1317–1319. https://doi.org/10.1016/j.jacr.2018.05.020
Dunning D, Griffin DW, Milojkovic JD, Ross L (1990) The overconfidence effect in social prediction. J Pers Soc Psychol 58:568–581. https://doi.org/10.1037//0022-3514.58.4.568
Acknowledgements
For the EARG Group (Eltewacy Arab Research Group):
Hajar Alkokhiya Aldare1, Mohammed Amir Rais2, Moath Salem3, Jaafar D. Al-Dabagh4, Monzer Abdulatif Alhassan5, Marah M Hanjul6, Tayba Abdulrahman Mugibel7, Sara Hamada Motawea8, Mirna Hussein9, Omar Saeed Anas10, Nacer Mohamed Amine11, Moath Ahmed Almekhlafi12, Muna Ali Mugibel7, Eman Salem Barhoom7, Haroun Neiroukh6, Raghad Shweiki13, Mohammad Khalaf Balaw14, Mohmmad Ahmad Al-Slehat15, Zaynab Roze4, Maram A. Sadeq16, Fathia Mokhtar5, Noora Mahdi Babiker5, Rami Abd Al-Ati5, Huda Adel Alhoudairi1, Mohammed Omran Attayeb17, Abdulrhman Abdulhadi18, Abdulghani Arja19, Abdulkareem Muhammad Wardeh20, Dana Nabil Alakhrass21, Souad Alkanj22
1Faculty of Medicine, Sabha University, Sabha, Libya
2Faculty of Medicine, University of Algiers 1, Algeria
3Faculty of Medicine, Damascus University, Damascus, Syria
4Faculty of Medicine, University of Baghdad, Baghdad, Iraq
5Faculty of Medicine and Health Sciences, Merowe University of Technology—Abdulatif Alhamad, Merowe, Sudan
6Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
7College of Medicine, Hadhramout University, Mukalla, Yemen
8Faculty of Medicine, Tanta University, Tanta, Egypt
9Faculty of Medicine, Alexandria University, Alexandria, Egypt
10Faculty of Medicine, Ain Shams University, Cairo, Egypt
11Faculty of Medicine of Blida, University of Blida 1 Saad Dahleb, Blida, Algeria
12Faculty of Medicine, Thamar University, Dhamar, Yemen
13Faculty of Medicine, Jordan University, Amman, Jordan
14Faculty of Medicine, Hashemite University, 13133, Zarqa, Jordan
15Faculty of Medicine, Al Balqa Applied University, As-Salt, Jordan
16Al-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq
17Faculty of Medicine, Tripoli University, Tripoli, Libya
18Faculty of Medicine, Alsham Private University, Damascus, Syria
19Faculty of Medicine, Aleppo University, Aleppo, Syria
20Faculty of Medicine, Tishreen University, Lattakia, Syria
21Faculty of Medicine, Al-Baath University, Homs, Syria
22Faculty of Medicine, Zagazig University, Zagazig 44519, Egypt
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Consortia
Contributions
Ahmed Hafez Allam contributed to the conception and design of the work, data collection (national leader), data analysis, interpretation, drafting and critical revision of the manuscript.
Nael Kamel Eltewacy contributed to the conception and design of the work.
Yasmeen Jamal Alabdallat contributed to data collection (national leader) and manuscript writing.
Tarek A. Owais performed the data analysis.
Saif Salman revised and edited the manuscript and the study protocol.
Mahmoud A. Ebada supervised the team, revised, and edited the manuscript.
EARG Group collected the data:
National leaders:
Hajar Alkokhiya Aldare, Mohammed Amir Rais, Moath Salem, Jaafar D. Al-Dabagh, Monzer Abdulatif Alhassan, Marah M Hanjul, Tayba Abdulrahman Mugibel.
Collaborators:
Sara Hamada Motawea, Mirna Hussein, Omar Saeed Anas, Nacer Mohamed Amine, Moath Ahmed Almekhlafi, Muna Ali Mugibel, Eman Salem Barhoom, Haroun Neiroukh, Raghad Shweiki, Mohammad Khalaf Balaw, Mohmmad Ahmad Al-Slehat, Zaynab Roze, Maram A. Sadeq, Fathia Mokhtar, Noora Mahdi Babiker, Rami Abd Al-Ati, Huda Adel Alhoudairi, Mohammed Omran Attayeb, Abdulrhman Abdulhadi, Abdulghani Arja, Abdulkareem Muhammad Wardeh, Dana Nabil Alakhrass, Souad Alkanj.
All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ahmed Hafez Allam.
Conflict of interest
The authors declare no conflict of interest or competing interests.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written consent was obtained from the participants after a detailed explanation of the study before filling out the questionnaire.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• Multi-center study
• Cross-sectional study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Allam, A.H., Eltewacy, N.K., Alabdallat, Y.J. et al. Knowledge, attitude, and perception of Arab medical students towards artificial intelligence in medicine and radiology: A multi-national cross-sectional study. Eur Radiol 34, 1–14 (2024). https://doi.org/10.1007/s00330-023-10509-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10509-2