Abstract
Objectives
To determine if three-dimensional (3D) radiomic features of contrast-enhanced CT (CECT) images improve prediction of rapid abdominal aortic aneurysm (AAA) growth.
Methods
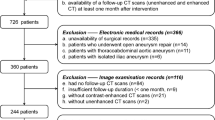
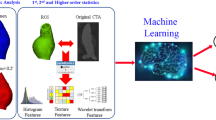
This longitudinal cohort study retrospectively analyzed 195 consecutive patients (mean age, 72.4 years ± 9.1) with a baseline CECT and a subsequent CT or MR at least 6 months later. 3D radiomic features were measured for 3 regions of the AAA, viz. the vessel lumen only; the intraluminal thrombus (ILT) and aortic wall only; and the entire AAA sac (lumen, ILT, and wall). Multiple machine learning (ML) models to predict rapid growth, defined as the upper tercile of observed growth (> 0.25 cm/year), were developed using data from 60% of the patients. Diagnostic accuracy was evaluated using the area under the receiver operating characteristic curve (AUC) in the remaining 40% of patients.
Results
The median AAA maximum diameter was 3.9 cm (interquartile range [IQR], 3.3–4.4 cm) at baseline and 4.4 cm (IQR, 3.7–5.4 cm) at the mean follow-up time of 3.2 ± 2.4 years (range, 0.5–9 years). A logistic regression model using 7 radiomic features of the ILT and wall had the highest AUC (0.83; 95% confidence interval [CI], 0.73–0.88) in the development cohort. In the independent test cohort, this model had a statistically significantly higher AUC than a model including maximum diameter, AAA volume, and relevant clinical factors (AUC = 0.78, 95% CI, 0.67–0.87 vs AUC = 0.69, 95% CI, 0.57–0.79; p = 0.04).
Conclusion
A radiomics-based method focused on the ILT and wall improved prediction of rapid AAA growth from CECT imaging.
Key Points
• Radiomic analysis of 195 abdominal CECT revealed that an ML-based model that included textural features of intraluminal thrombus (if present) and aortic wall improved prediction of rapid AAA progression compared to maximum diameter.
• Predictive accuracy was higher when radiomic features were obtained from the thrombus and wall as opposed to the entire AAA sac (including lumen), or the lumen alone.
• Logistic regression of selected radiomic features yielded similar accuracy to predict rapid AAA progression as random forests or support vector machines.






Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- AAA:
-
Abdominal aortic aneurysm
- AUC:
-
Area under the receiver operating characteristic curve
- CECT:
-
Contrast-enhanced CT
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- ICC:
-
Intraclass correlation coefficient
- ILT:
-
Intraluminal thrombus
- IQR:
-
Interquartile range
- LR:
-
Logistic regression
- LSSPM:
-
Level set shape prior method
- ML:
-
Machine learning
- MR:
-
Magnetic resonance
- PCA:
-
Principal component analysis
- RBLOW:
-
Region between lumen and outer wall
- RF:
-
Random forest
- RFE:
-
Recursive feature elimination
- RIL:
-
Region within lumen
- ROI:
-
Region of interest
- ROW:
-
Region within outer wall
- SVM:
-
Support vector machine
References
LeFevre ML (2014) Screening for abdominal aortic aneurysm: US Preventive Services Task Force recommendation statement. Ann Intern Med 161:281–290
Li X, Zhao G, Zhang J, Duan Z, Xin S (2013) Prevalence and trends of the abdominal aortic aneurysms epidemic in general population–a meta-analysis. PLoS One 8:e81260
Soden PA, Zettervall SL, Ultee KH et al (2016) Outcomes for symptomatic abdominal aortic aneurysms in the American College of Surgeons National Surgical Quality Improvement Program. J Vasc Surg 64:297–305
Powell JT, Brown LC, Forbes JF et al (2007) Final 12-year follow-up of surgery versus surveillance in the UK Small Aneurysm Trial. Br J Surg 94:702–708
Castro-Ferreira R, Lachat M, Schneider PA, Freitas A, Leite-Moreira A, Sampaio SM (2019) Disparities in contemporary treatment rates of abdominal aortic aneurysms across western countries. Eur J Vasc Endovasc Surg 58:200–205
Dua A, Kuy S, Lee CJ, Upchurch GR Jr, Desai SS (2014) Epidemiology of aortic aneurysm repair in the United States from 2000 to 2010. J Vasc Surg 59:1512–1517
Brox AC, Filion KB, Zhang X et al (2003) In-hospital cost of abdominal aortic aneurysm repair in Canada and the United States. Arch Intern Med 163:2500–2504
Suckow BD, Goodney PP, Columbo JA et al (2018) National trends in open surgical, endovascular, and branched-fenestrated endovascular aortic aneurysm repair in Medicare patients. J Vasc Surg 67:1690–1697.e1
Bath J, Hartwig J, Dombrovskiy VY, Vogel TR (2020) Trends in management and outcomes of vascular emergencies in the nationwide inpatient sample. Vasa 49:99–105
Chaikof EL, Dalman RL, Eskandari MK et al (2018) The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg 67:2-77.e72
Chaikof EL, Blankensteijn J, Harris P, White G, Zarins C, Bernhard V (2002) Ad hoc committee for standardized reporting practices in vascular surgery of the Society for Vascular Surgery/American Association for Vascular Surgery. Reporting standards for endovascular aortic aneurysm repair. J Vasc Surg 35:1048–1060
Ahmad M, Mistry R, Hodson J, Bradbury AW (2017) How quickly do asymptomatic infrarenal abdominal aortic aneurysms grow and what factors affect aneurysm growth rates? Analysis of a single centre surveillance cohort database. Eur J Vasc Endovasc Surg 54:597–603
Brady AR, Thompson SG, Fowkes FG, Greenhalgh RM, Powell JT, Participants UKSAT (2004) Abdominal aortic aneurysm expansion: risk factors and time intervals for surveillance. Circulation 110:16–21
Lee R, Jarchi D, Perera R et al (2018) Applied machine learning for the prediction of growth of abdominal aortic aneurysm in humans. EJVES Short Rep 39:24–28
Mitsouras D, Leach JR (2020) Expanding the radiologistʼs arsenal against abdominal aortic aneurysms, a versatile adversary. Radiology 295:730–732
Lao J, Chen Y, Li ZC et al (2017) A deep learning-based radiomics model for prediction of survival in glioblastoma multiforme. Sci Rep 7:10353
Aerts HJ, Velazquez ER, Leijenaar RT et al (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5:4006
Rogers W, Thulasi Seetha S, Refaee TA et al (2020) Radiomics: from qualitative to quantitative imaging. Br J Radiol 93:20190948
Bibault J-E, Xing L, Giraud P et al (2020) Radiomics: a primer for the radiation oncologist. Cancer Radiother 24:403–410
Kolossváry M, Karády J, Szilveszter B et al (2017) Radiomic features are superior to conventional quantitative computed tomographic metrics to identify coronary plaques with napkin-ring sign. Circ Cardiovasc Imaging 10:e006843
Kolossváry M, Kellermayer M, Merkely B, Maurovich-Horvat P (2018) Cardiac computed tomography radiomics. J Thorac Imaging 33:26–34
Larue RT, Defraene G, De Ruysscher D, Lambin P, Van Elmpt W (2017) Quantitative radiomics studies for tissue characterization: a review of technology and methodological procedures. Br J Radiol 90:20160665
Zhu C, Tian B, Leach JR et al (2017) Non-contrast 3D black blood MRI for abdominal aortic aneurysm surveillance: comparison with CT angiography. Eur Radiol 27:1787–1794
Wang Y, Tian B, Xiong F et al (2021) Computer-aided quantification of non-contrast 3D black blood MRI as an efficient alternative to reference standard manual CT angiography measurements of abdominal aortic aneurysms. Eur J Radiol 134:109396
Raghunath S, Ulloa Cerna AE, Jing L et al (2020) Prediction of mortality from 12-lead electrocardiogram voltage data using a deep neural network. Nat Med 26:886–891
Wang Y, Zhang Y, Xuan W et al (2019) Fully automatic segmentation of 4D MRI for cardiac functional measurements. Med Phys 46:180–189
Wang Y, Kao E, Zhang Y et al (2019) Shape-appearance constrained segmentation and separation of vein and artery in pulsatile tinnitus patients based on MR angiography and flow MRI. Magn Reson Imaging 61:187–195
Van Griethuysen JJ, Fedorov A, Parmar C et al (2017) Computational radiomics system to decode the radiographic phenotype. Can Res 77:e104–e107
Aghayev A, Giannopoulos AA, Gronsbell J et al (2018) Common first-pass CT angiography findings associated with rapid growth rate in abdominal aorta aneurysms between 3 and 5 cm in largest diameter. AJR Am J Roentgenol 210:431–437
Reeps C, Pelisek J, Seidl S et al (2009) Inflammatory infiltrates and neovessels are relevant sources of MMPs in abdominal aortic aneurysm wall. Pathobiology 76:243–252
Zhu A, Leach JR, Zhu C et al (2023) Dynamic contrast-enhanced MRI in abdominal aortic aneurysms as a potential marker for disease progression. J Magn Reson Imaging. https://doi.org/10.1002/jmri.28640
Yang R, Wu J, Sun L et al (2020) Radiomics of small renal masses on multiphasic CT: accuracy of machine learning–based classification models for the differentiation of renal cell carcinoma and angiomyolipoma without visible fat. Eur Radiol 30:1254–1263
Patro S, Sahu KK (2015) Normalization: a preprocessing stage. arXiv preprint arXiv:150306462
Pearson K (1901) LIII. On lines and planes of closest fit to systems of points in space. The London, Edinburgh, and Dublin Philosophical Magazine and Journal of Science 2:559–572
Guyon I, Weston J, Barnhill S, Vapnik V (2002) Gene selection for cancer classification using support vector machines. Mach Learn 46:389–422
Liaw A, Wiener M (2002) Classification and regression by randomForest. R news 2:18–22
Cortes C, Vapnik V (1995) Support-vector networks. Machine Learn 20:273–297
Zhu C, Leach JR, Tian B et al (2019) Evaluation of the distribution and progression of intraluminal thrombus in abdominal aortic aneurysms using high-resolution MRI. J Magn Reson Imaging 50:994–1001
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Meyrignac O, Bal L, Zadro C et al (2020) Combining volumetric and wall shear stress analysis from CT to assess risk of abdominal aortic aneurysm progression. Radiology 295:722–729
Olson SL, Panthofer AM, Blackwelder W et al (2022) Role of volume in small abdominal aortic aneurysm surveillance. J Vasc Surg 75:1260–1267.e3
Zhu C, Leach JR, Wang Y, Gasper W, Saloner D, Hope MD (2020) Intraluminal thrombus predicts rapid growth of abdominal aortic aneurysms. Radiology 294:707–713
Buijs RV, Willems TP, Tio RA et al (2013) Calcification as a risk factor for rupture of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 46:542–548
Behr-Rasmussen C, Grøndal N, Bramsen MB, Thomsen MD, Lindholt JS (2014) Mural thrombus and the progression of abdominal aortic aneurysms: a large population-based prospective cohort study. Eur J Vasc Endovasc Surg 48:301–307
Koole D, Zandvoort HJ, Schoneveld A et al (2013) Intraluminal abdominal aortic aneurysm thrombus is associated with disruption of wall integrity. J Vasc Surg 57:77–83
The MA3RS Study Investigators, Newby D, Forsythe R et al (2017) Aortic wall inflammation predicts abdominal aortic aneurysm expansion, rupture, and need for surgical repair. Circulation 136:787–797
Syed MBJ, Fletcher AJ, Dweck MR, Forsythe R, Newby DE (2019) Imaging aortic wall inflammation. Trends Cardiovasc Med 29:440–448
Gasser TC (2016) Biomechanical rupture risk assessment: a consistent and objective decision-making tool for abdominal aortic aneurysm patients. Aorta (Stamford) 4:42–60
Groeneveld ME, Meekel JP, Rubinstein SM et al (2018) Systematic review of circulating, biomechanical, and genetic markers for the prediction of abdominal aortic aneurysm growth and rupture. J Am Heart Assoc 30;7(13):e007791
RESCAN Collaborators, Bown MJ, Sweeting MJ, Brown LC, Powell JT, Thompson SG (2013) Surveillance intervals for small abdominal aortic aneurysms: a meta-analysis. JAMA 309:806–813
Olson SL, Wijesinha MA, Panthofer AM et al (2021) Evaluating growth patterns of abdominal aortic aneurysm diameter with serial computed tomography surveillance. JAMA Surg 156:363–370
Sweeting MJ, Thompson SG, Brown LC, Powell JT, collaborators R (2012) Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br J Surg 99:655–665
Brown PM, Zelt DT, Sobolev B (2003) The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg 37:280–284
Thompson AR, Cooper JA, Ashton HA, Hafez H (2010) Growth rates of small abdominal aortic aneurysms correlate with clinical events. Br J Surg 97:37–44
Chun KC, Schmidt AS, Bains S et al (2016) Surveillance outcomes of small abdominal aortic aneurysms identified from a large screening program. J Vasc Surg 63:55–61
Mell MW, Baker LC, Dalman RL, Hlatky MA (2014) Gaps in preoperative surveillance and rupture of abdominal aortic aneurysms among Medicare beneficiaries. J Vasc Surg 59:583–588
Tomee SM, Bastiaannet E, Schermerhorn ML, Golledge J, Hamming JF, Lindeman JH (2017) The consequences of real life practice of early abdominal aortic aneurysm repair: a cost-benefit analysis. Eur J Vasc Endovasc Surg 54:28–33
Ding N, Hao Y, Wang Z et al (2020) CT texture analysis predicts abdominal aortic aneurysm post-endovascular aortic aneurysm repair progression. Sci Rep 10:12268
Jones JE, Atkins MD, Brewster DC et al (2007) Persistent type 2 endoleak after endovascular repair of abdominal aortic aneurysm is associated with adverse late outcomes. J Vasc Surg 46:1–8
Sakuta A, Kimura F, Aoka Y, Aomi S, Hagiwara N, Kasanuki H (2007) Delayed enhancement on computed tomography in abdominal aortic aneurysm wall. Heart Vessels 22:79–87
Parmar C, Grossmann P, Bussink J, Lambin P, Aerts H (2015) Machine learning methods for quantitative radiomic biomarkers. Sci Rep 5:13087
Xue C, Yuan J, Lo GG et al (2021) Radiomics feature reliability assessed by intraclass correlation coefficient: a systematic review. Quant Imaging Med Surg 11:4431
Funding
This research was supported by the Veterans Affairs Office of Research and Development grant number I01-CX002071, National Institutes of Health grant number R01-HL114118, and American Heart Association award number AHA19POST34450257.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dimitrios Mitsouras.
Conflict of interest
Fei Xiong is currently an employee of Siemens Medical Solutions USA, Inc. This research work was completed during her graduate study at USCF; there is no relevance to her current role.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in
Zhu C, Leach JR, Wang Y, Gasper W, Saloner D, Hope MD. Intraluminal thrombus predicts rapid growth of abdominal aortic aneurysms. Radiology. 2020;294(3):707-13.
Methodology
• retrospective
• experimental
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Xiong, F., Leach, J. et al. Contrast-enhanced CT radiomics improves the prediction of abdominal aortic aneurysm progression. Eur Radiol 33, 3444–3454 (2023). https://doi.org/10.1007/s00330-023-09490-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09490-7