Abstract
Objectives
To comprehensively evaluate the pelvic magnetic resonance imaging (MRI) findings of Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome and summarize the typical and atypical characteristics.
Methods
A retrospective analysis of 201 consecutive MRKH patients was carried out. Pelvic MRI was reviewed by two experienced gynecological radiologists in consensus. Characteristics including the morphology, signal pattern and volumes of the uterine rudiments, location and volume of the ovaries, and the degree of vaginal dysgenesis were evaluated. Other noted abnormalities were also recorded.
Results
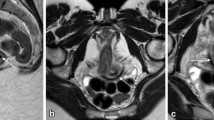
Morphologically, the majority (95%) of patients displayed bilateral uterine rudiments combined with a fibrous band. The minority of patients showed no (3.5%) or unilateral (1.5%) uterine rudiments. A total of 385 uterine rudiments were detected which showed four types of signal patterns: one-layer differentiation (325, 84.4%), two-layer differentiation (27, 7%), three-layer differentiation without subsequent alteration (23, 6.0%), and three-layer differentiation with hematometra and/or ipsilateral hematosalpinx (10, 2.6%). The median volumes of these four types of uterine rudiments were 2.6 ml (1.69–3.81 ml), 3.19 ml (2.67–4.51 ml), 6.05 ml (3.37–12.44 ml), and 31.97 ml (19.2–38.7 ml), respectively. The mean ovarian volume was 6.49 ± 3.91 ml. Abnormally located ovaries were detected in 63 (31.3%) patients. The distal vagina was discernable in 25.1% of patients.
Conclusion
MRKH patients typically display bilateral uterine rudiments combined with a fibrous band and normally located ovaries. The uterine rudiments are generally small with only one-layer differentiation, a subset of which might be large and exhibited other atypical presentations, including two- or three-layer differentiation or even hematometra. Abnormally located ovaries are not rare.
Key Points
• Morphologically, MRKH patients typically displayed bilateral uterine rudiments combined with a fibrous band.
• Typically, the uterine rudiments (84.4%) were small and displayed only one-layer differentiation.
• About 15.6% of rudiments showed atypical characteristics including two- or three-layer differentiation, even complicated with hematometra or hematosalpinx.





Similar content being viewed by others
Abbreviations
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging.
- MRKH:
-
Mayer-Rokitansky-Küster-Hauser
- TE:
-
Echo time
- TR:
-
Repetition time
References
Patnaik SS, Brazile B, Dandolu V, Ryan PL, Liao J (2015) Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome: a historical perspective. Gene 555:33–40
Londra L, Chuong FS, Kolp L (2015) Mayer-Rokitansky-Kuster-Hauser syndrome: a review. Int J Womens Health 7:865–870
Robbins JB, Broadwell C, Chow LC, Parry JP, Sadowski EA (2015) Mullerian duct anomalies: embryological development, classification, and MRI assessment. J Magn Reson Imaging 41:1–12
Pizzo A, Lagana AS, Sturlese E et al (2013) Mayer-Rokitansky-Kuster-Hauser syndrome: embryology, genetics and clinical and surgical treatment. ISRN Obstet Gynecol 2013:628717
Bombard DS, Mousa SA (2014) Mayer-Rokitansky-Kuster-Hauser syndrome: complications, diagnosis and possible treatment options: a review. Gynecol Endocrinol 30:618–623
Choussein S, Nasioudis D, Schizas D, Economopoulos KP (2017) Mullerian dysgenesis: a critical review of the literature. Arch Gynecol Obstet 295:1369–1381
Herlin M, Hojland AT, Petersen MB (2014) Familial occurrence of Mayer-Rokitansky-Kuster-Hauser syndrome: a case report and review of the literature. Am J Med Genet A 164A:2276–2286
Rall K, Eisenbeis S, Henninger V et al (2015) Typical and atypical associated findings in a group of 346 patients with Mayer-Rokitansky-Kuester-Hauser syndrome. J Pediatr Adolesc Gynecol 28:362–368
Oppelt PG, Lermann J, Strick R et al (2012) Malformations in a cohort of 284 women with Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH). Reprod Biol Endocrinol 10:57. https://doi.org/10.1186/1477-7827-10-57
Oppelt P, Renner SP, Kellermann A et al (2006) Clinical aspects of Mayer-Rokitansky-Kuester-Hauser syndrome: recommendations for clinical diagnosis and staging. Hum Reprod 21:792–797
Sybert VP, McCauley E (2004) Turner’s Syndrome. N Engl J Med 351:1227–1238
Rousset P, Raudrant D, Peyron N, Buy JN, Valette PJ, Hoeffel C (2013) Ultrasonography and MRI features of the Mayer-Rokitansky-Kuster-Hauser syndrome. Clin Radiol 68:945–952
Rall K, Barresi G, Wallwiener D, Brucker SY, Staebler A (2013) Uterine rudiments in patients with Mayer-Rokitansky-Kuster-Hauser syndrome consist of typical uterine tissue types with predominantly basalis-like endometrium. Fertil Steril 99:1392–1399
Yoo RE, Cho JY, Kim SY, Kim SH (2015) A systematic approach to the magnetic resonance imaging-based differential diagnosis of congenital Mullerian duct anomalies and their mimics. Abdom Imaging 40:192–206
Wang Y, Lu J, Zhu L et al (2018) Increased incidence of abnormally located ovary in patients with Mayer–Rokitansky–Küster–Hauser syndrome: a retrospective analysis with magnetic resonance imaging. Abdom Radiol (NY) 43:3142–3146
Allen JW, Cardall S, Kittijarukhajorn M, Siegel CL (2012) Incidence of ovarian maldescent in women with mullerian duct anomalies: evaluation by MRI. AJR Am J Roentgenol 198:W381–W385
Trinidad C, Tardaguila F, Fernandez GC, Martinez C, Chavarri E, Rivas I (2004) Ovarian maldescent. Eur Radiol 14:805–808
Hall-Craggs MA, Williams CE, Pattison SH, Kirkham AP, Creighton SM (2013) Mayer-Rokitansky-Kuster-Hauser syndrome: diagnosis with MR imaging. Radiology 269:787–792
Pompili G, Munari A, Franceschelli G et al (2009) Magnetic resonance imaging in the preoperative assessment of Mayer-Rokitansky-Kuster-Hauser syndrome. Radiol Med 114:811–826
Yoo RE, Cho JY, Kim SY, Kim SH (2013) Magnetic resonance evaluation of Mullerian remnants in Mayer-Rokitansky-Kuster-Hauser syndrome. Korean J Radiol 14:233–239
Wang Y, Lu J, Zhu L et al (2017) Evaluation of Mayer-Rokitansky-Kuster-Hauser syndrome with magnetic resonance imaging: three patterns of uterine remnants and related anatomical features and clinical settings. Eur Radiol 27:5215–5224
Gould SW, Epelman M (2015) Magnetic resonance imaging of developmental anomalies of the uterus and the vagina in pediatric patients. Semin Ultrasound CT MR 36:332–347
Brix N, Ernst A, Lauridsen LLB et al (2019) Timing of puberty in boys and girls: a population-based study. Paediatr Perinat Epidemiol 33:70–78
Preibsch H, Rall K, Wietek BM et al (2014) Clinical value of magnetic resonance imaging in patients with Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome: diagnosis of associated malformations, uterine rudiments and intrauterine endometrium. Eur Radiol 24:1621–1627
Ludwig KS (1998) The Mayer-Rokitansky-Küster syndrome. An analysis of its morphology and embryology. Part I: morphology. Arch Gynecol Obstet 262:1–26
Ludwig KS (1998) The Mayer-Rokitansky-Küster syndrome. An analysis of its morphology and embryology. Part II: embryology. Arch Gynecol Obstet 262:27–42
Dietrich JE, Hertweck SP, Bond S (2007) Undescended ovaries: a clinical review. J Pediatr Adolesc Gynecol 20:57–60
Nisolle M, Donnez J (1997) Peritoneal endometriosis, ovarian endometriosis, and adenomytic nodules of the rectovaginal septum are three different entities. Fertil Steril 68:585–596
Sharara FI, McClamrock HD (1999) The effect of aging on ovarian volume measurements in infertile women. Obstet Gynecol 94:57–60
Marsh CA, Will MA, Smorgick N, Quint EH, Hussain H, Smith YR (2013) Uterine remnants and pelvic pain in females with Mayer-Rokitansky-Küster-Hauser syndrome. J Pediatr Adolesc Gynecol 26:199–202
Funding
The study was funded by the National Public Welfare Basic Scientific Research Program of the Chinese Academy of Medical Sciences (2019PT320008 and 2018PT32003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Zheng-Yu Jin.
Conflict of interest
All authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., He, YL., Yuan, L. et al. Typical and atypical pelvic MRI characteristics of Mayer-Rokitansky-Küster-Hauser syndrome: a comprehensive analysis of 201 patients. Eur Radiol 30, 4014–4022 (2020). https://doi.org/10.1007/s00330-020-06681-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06681-4