Abstract
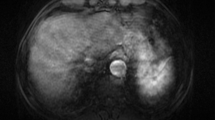
Hepatocellular carcinoma (HCC) is a unique malignancy that can be diagnosed and treated based on non-invasive imaging criteria without histological confirmation in cirrhotic patients, which opens the possibility, although rare, of false-positive diagnosis of the tumor. This brief review illustrates benign and non-HCC malignant lesions arising in cirrhotic liver that could have been erroneously diagnosed as HCC based on imaging criteria: focal nodular hyperplasia–like nodules, serum amyloid A–positive nodules, dysplastic nodules, spontaneously regressing lesions, combined hepatocellular-cholangiocarcinoma, cholangiocarcinoma, sarcomatoid carcinoma, lymphoepithelioma-like carcinoma, hepatoblastoma, and metastatic adenocarcinoma. To determine the potential differences in clinical courses and post-treatment outcome of HCC diagnosed by imaging alone and those histologically, we suggest the terms HCCi and HCCp to distinguish between lesions that are diagnosed as HCC based on imaging alone from those diagnosed based on pathological examination, respectively.
Key Points
• Benign lesions, such as focal nodular hyperplasia–like nodules, serum amyloid A–positive nodules, dysplastic nodules, and spontaneously regressing lesions, may show imaging findings that mislead to the diagnosis of HCC.
• Non-hepatocellular malignant lesions, such as sarcomatoid carcinoma, lymphoepithelioma-like carcinoma, hepatoblastoma, and metastatic adenocarcinomas, can be erroneously diagnosed as HCC based on imaging findings alone, even in cirrhotic liver.






Similar content being viewed by others
Abbreviations
- APHE:
-
Arterial phase hyperenhancement
- cHCC-CCA:
-
Combined hepatocellular-cholangiocarcinoma
- FNH-LNs:
-
Focal nodular hyperplasia–like nodules
- HCC:
-
Hepatocellular carcinoma
- HCCi:
-
HCC diagnosed by imaging criteria alone
- HCCp:
-
HCC diagnosed on pathologic examination
- LELC:
-
Lymphoepithelioma-like carcinoma
- LI-RADS:
-
Liver reporting and data system
- MF-iCCA:
-
Mass-forming intrahepatic cholangiocarcinoma
- SAA:
-
Serum amyloid A
References
Kudo M, Trevisani F, Abou-Alfa GK, Rimassa L (2016) Hepatocellular carcinoma: therapeutic guidelines and medical treatment. Liver Cancer 6:16–26
Heimbach JK, Kulik LM, Finn RS et al (2018) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67:358–380
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Park HJ, Choi BI, Lee ES, Park SB, Lee JB (2017) How to differentiate borderline hepatic nodules in hepatocarcinogenesis: emphasis on imaging diagnosis. Liver Cancer 6:189–203
Chernyak V, Fowler KJ, Kamaya A et al (2018) Liver Imaging Reporting and Data System (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology 289:816–830
Ronot M, Dioguardi Burgio M, Purcell Y, Pommier R, Brancatelli G, Vilgrain V (2017) Focal lesions in cirrhosis: not always HCC. Eur J Radiol 93:157–168
Galia M, Taibbi A, Marin D et al (2014) Focal lesions in cirrhotic liver: what else beyond hepatocellular carcinoma? Diagn Interv Radiol 20:222–228
Elsayes KM, Chernyak V, Morshid AI et al (2018) Spectrum of pitfalls, pseudolesions, and potential misdiagnoses in cirrhosis. AJR Am J Roentgenol 211:87–96
Cruite I, Tang A, Sirlin CB (2013) Imaging-based diagnostic systems for hepatocellular carcinoma. AJR Am J Roentgenol 201:41–55
Tang A, Bashir MR, Corwin MT et al (2018) Evidence supporting LI-RADS major features for CT- and MR imaging-based diagnosis of hepatocellular carcinoma: a systematic review. Radiology 286:29–48
Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB (2018) Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol (NY) 43:13–25
Lee YH, Kim SH, Cho MY, Shim KY, Kim MS (2007) Focal nodular hyperplasia-like nodules in alcoholic liver cirrhosis: radiologic-pathologic correlation. AJR Am J Roentgenol 188:W459–W463
Marin D, Galluzzo A, Plessier A, Brancatelli G, Valla D, Vilgrain V (2011) Focal nodular hyperplasia-like lesions in patients with cavernous transformation of the portal vein: prevalence, MR findings and natural history. Eur Radiol 21:2074–2082
Choi JY, Lee HC, Yim JH et al (2011) Focal nodular hyperplasia or focal nodular hyperplasia-like lesions of the liver: a special emphasis on diagnosis. J Gastroenterol Hepatol 26:1004–1009
Kim JW, Lee CH, Kim SB et al (2017) Washout appearance in Gd-EOB-DTPA-enhanced MR imaging: a differentiating feature between hepatocellular carcinoma with paradoxical uptake on the hepatobiliary phase and focal nodular hyperplasia-like nodules. J Magn Reson Imaging 45:1599–1608
Libbrecht L, Cassiman D, Verslype C et al (2006) Clinicopathological features of focal nodular hyperplasia-like nodules in 130 cirrhotic explant livers. Am J Gastroenterol 101:2341–2346
Kim MJ, Rhee HJ, Jeong HT (2012) Hyperintense lesions on gadoxetate disodium-enhanced hepatobiliary phase imaging. AJR Am J Roentgenol 199:W575–W586
Sasaki M, Yoneda N, Sawai Y et al (2015) Clinicopathological characteristics of serum amyloid A-positive hepatocellular neoplasms/nodules arising in alcoholic cirrhosis. Histopathology 66:836–845
Kim SR, Kondo F, Otono Y et al (2014) Serum amyloid A and C-reactive protein positive nodule in alcoholic liver cirrhosis, hard to make definite diagnosis. Hepatol Res 44:584–590
Lim JH, Cho JM, Kim EY, Park CK (2000) Dysplastic nodules in liver cirrhosis: evaluation of hemodynamics with CT during arterial portography and CT hepatic arteriography. Radiology 214:869–874
Chou CT, Chou JM, Chang TA et al (2013) Differentiation between dysplastic nodule and early-stage hepatocellular carcinoma: the utility of conventional MR imaging. World J Gastroenterol 19:7433–7439
Lim JH, Kim MJ, Park CK, Kang SS, Lee WJ, Lim HK (2004) Dysplastic nodules in liver cirrhosis: detection with triple phase helical dynamic CT. Br J Radiol 77:911–916
Inchingolo R, De Gaetano AM, Curione D et al (2015) Role of diffusion-weighted imaging, apparent diffusion coefficient and correlation with hepatobiliary phase findings in the differentiation of hepatocellular carcinoma from dysplastic nodules in cirrhotic liver. Eur Radiol 25:1087–1096
Sersté T, Barrau V, Ozenne V et al (2012) Accuracy and disagreement of computed tomography and magnetic resonance imaging for the diagnosis of small hepatocellular carcinoma and dysplastic nodules: role of biopsy. Hepatology 55:800–806
Choi MH, Choi JI, Lee YJ, Park MY, Rha SE, Lall C (2016) MRI of small hepatocellular carcinoma: typical features are less frequent below a size cutoff of 1.5 cm. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.16.16414:1-8
Rhee H, Kim MJ, Park MS, Kim KA (2012) Differentiation of early hepatocellular carcinoma from benign hepatocellular nodules on gadoxetic acid-enhanced MRI. Br J Radiol 85:e837–e844
Kim TK, Lee KH, Jang HJ et al (2011) Analysis of gadobenate dimeglumine-enhanced MR findings for characterizing small (1-2-cm) hepatic nodules in patients at high risk for hepatocellular carcinoma. Radiology 259:730–738
Renzulli M, Biselli M, Brocchi S et al (2018) New hallmark of hepatocellular carcinoma, early hepatocellular carcinoma and high-grade dysplastic nodules on Gd-EOB-DTPA MRI in patients with cirrhosis: a new diagnostic algorithm. Gut 67:1674–1682
Byrnes V, Shi H, Kiryu S, Rofsky NM, Afdhal NH (2007) The clinical outcome of small (<20 mm) arterially enhancing nodules on MRI in the cirrhotic liver. Am J Gastroenterol 102:1654–1659
Park CJ, An C, Park S, Choi JY, Kim MJ (2018) Management of subcentimetre arterially enhancing and hepatobiliary hypointense lesions on gadoxetic acid-enhanced MRI in patients at risk for HCC. Eur Radiol 28:1476–1484
Kim JE, Kim SH, Lee SJ, Rhim H (2011) Hypervascular hepatocellular carcinoma 1 cm or smaller in patients with chronic liver disease: characterization with gadoxetic acid-enhanced MRI that includes diffusion-weighted imaging. AJR Am J Roentgenol 196:W758–W765
Lee SC, Chung HW, Chung JB et al (2002) Total necrosis of hepatocellular carcinoma due to spontaneous occlusion of feeding artery. Yonsei Med J 43:123–127
Del Poggio P, Mattiello M, Gilardoni L, Jamoletti C, Colombo S, Zabbialini G (2009) The mysterious case of spontaneous disappearance of hepatocellular carcinoma. Dig Liver Dis 41:e21–e25
Matsuoka S, Tamura A, Moriyama M et al (2015) Pathological evidence of the cause of spontaneous regression in a case of resected hepatocellular carcinoma. Intern Med 54:25–30
Bhardwaj N, Li M, Price T, Maddern GJ (2014) Spontaneous regression of a biopsy confirmed hepatocellular carcinoma. BMJ Case Rep 2014
Brunt E, Aishima S, Clavien PA et al (2018) cHCC-CCA: consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentiation. Hepatology 68:113–126
Fraum TJ, Tsai R, Rohe E et al (2018) Differentiation of hepatocellular carcinoma from other hepatic malignancies in patients at risk: diagnostic performance of the Liver Imaging Reporting and Data System version 2014. Radiology 286:158–172
Kim YY, An C, Kim S, Kim MJ (2018) Diagnostic accuracy of prospective application of the Liver Imaging Reporting and Data System (LI-RADS) in gadoxetate-enhanced MRI. Eur Radiol 28:2038–2046
Potretzke TA, Tan BR, Doyle MB, Brunt EM, Heiken JP, Fowler KJ (2016) Imaging features of biphenotypic primary liver carcinoma (hepatocholangiocarcinoma) and the potential to mimic hepatocellular carcinoma: LI-RADS analysis of CT and MRI features in 61 cases. AJR Am J Roentgenol 207:25–31
Lee HS, Kim MJ, An C (2018) How to utilize LR-M features of the LI-RADS to improve the diagnosis of combined hepatocellular-cholangiocarcinoma on gadoxetate-enhanced MRI? Eur Radiol. https://doi.org/10.1007/s00330-018-5893-1
Jeon SK, Joo I, Lee DH et al (2018) Combined hepatocellular cholangiocarcinoma: LI-RADS v2017 categorisation for differential diagnosis and prognostication on gadoxetic acid-enhanced MR imaging. Eur Radiol. https://doi.org/10.1007/s00330-018-5605-x
Rogers JE, Bolonesi RM, Rashid A et al (2017) Systemic therapy for unresectable, mixed hepatocellular-cholangiocarcinoma: treatment of a rare malignancy. J Gastrointest Oncol 8:347–351
Lunsford KE, Court C, Seok Lee Y et al (2018) Propensity-matched analysis of patients with mixed hepatocellular-cholangiocarcinoma and hepatocellular carcinoma undergoing liver transplantation. Liver Transpl 24:1384–1397
Choi SH, Lee SS, Kim SY et al (2017) Intrahepatic cholangiocarcinoma in patients with cirrhosis: differentiation from hepatocellular carcinoma by using gadoxetic acid-enhanced MR imaging and dynamic CT. Radiology 282:771–781
Huang B, Wu L, Lu XY et al (2016) Small intrahepatic cholangiocarcinoma and hepatocellular carcinoma in cirrhotic livers may share similar enhancement patterns at multiphase dynamic MR imaging. Radiology 281:150–157
Chung YE, Kim MJ, Park YN et al (2009) Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 29:683–700
Xu J, Igarashi S, Sasaki M et al (2012) Intrahepatic cholangiocarcinomas in cirrhosis are hypervascular in comparison with those in normal livers. Liver Int 32:1156–1164
Sheng RF, Zeng MS, Rao SX, Ji Y, Chen LL (2014) MRI of small intrahepatic mass-forming cholangiocarcinoma and atypical small hepatocellular carcinoma (≤3 cm) with cirrhosis and chronic viral hepatitis: a comparative study. Clin Imaging 38:265–272
Kim SA, Lee JM, Lee KB et al (2011) Intrahepatic mass-forming cholangiocarcinomas: enhancement patterns at multiphasic CT, with special emphasis on arterial enhancement pattern--correlation with clinicopathologic findings. Radiology 260:148–157
Jeong HT, Kim MJ, Chung YE, Choi JY, Park YN, Kim KW (2013) Gadoxetate disodium-enhanced MRI of mass-forming intrahepatic cholangiocarcinomas: imaging-histologic correlation. AJR Am J Roentgenol 201:W603–W611
Fujita N, Asayama Y, Nishie A et al (2017) Mass-forming intrahepatic cholangiocarcinoma: enhancement patterns in the arterial phase of dynamic hepatic CT - correlation with clinicopathological findings. Eur Radiol 27:498–506
Nanashima A, Abo T, Murakami G et al (2013) Intrahepatic cholangiocarcinoma: relationship between tumor imaging enhancement by measuring attenuation and clinicopathologic characteristics. Abdom Imaging 38:785–792
Aherne EA, Pak LM, Goldman DA et al (2018) Intrahepatic cholangiocarcinoma: can imaging phenotypes predict survival and tumor genetics? Abdom Radiol (NY). https://doi.org/10.1007/s00261-018-1505-4
Torbenson MS (2017) Morphologic subtypes of hepatocellular carcinoma. Gastroenterol Clin North Am 46:365–391
Gu KW, Kim YK, Min JH, Ha SY, Jeong WK (2017) Imaging features of hepatic sarcomatous carcinoma on computed tomography and gadoxetic acid-enhanced magnetic resonance imaging. Abdom Radiol (NY) 42:1424–1433
Pua U, Low SC, Tan YM, Lim KH (2009) Combined hepatocellular and cholangiocarcinoma with sarcomatoid transformation: radiologic-pathologic correlation of a case. Hepatol Int 3:587–592
Koo HR, Park MS, Kim MJ et al (2008) Radiological and clinical features of sarcomatoid hepatocellular carcinoma in 11 cases. J Comput Assist Tomogr 32:745–749
Honda H, Hayashi T, Yoshida K et al (1996) Hepatocellular carcinoma with sarcomatous change: characteristic findings of two-phased incremental CT. Abdom Imaging 21:37–40
Liao SH, Su TH, Jeng YM et al (2018) Clinical manifestations and outcomes of patients with sarcomatoid hepatocellular carcinoma. Hepatology. https://doi.org/10.1002/hep.30162
Labgaa I, Stueck A, Ward SC (2017) Lymphoepithelioma-like carcinoma in liver. Am J Pathol 187:1438–1444
Chan AW, Tong JH, Pan Y et al (2015) Lymphoepithelioma-like hepatocellular carcinoma: an uncommon variant of hepatocellular carcinoma with favorable outcome. Am J Surg Pathol 39:304–312
Cacciato Insilla A, Faviana P, Pollina LE et al (2015) Lymphoepithelioma-like hepatocellular carcinoma: case report and review of the literature. World J Gastroenterol 21:10468–10474
Kim YC, Park MS, Chung YE et al (2010) MRI findings of uncommon non-hepatocyte origin primary liver tumours with pathological correlation. Br J Radiol 83:1080–1086
Liao TC, Liu CA, Chiu NC, Yeh YC, Chiou YY (2015) Lymphoepithelioma-like cholangiocarcinoma: a mimic of hepatocellular carcinoma on imaging features. World J Gastroenterol 21:4089–4095
Lee H, Yoon JH, Kim H et al (2017) False positive diagnosis of hepatocellular carcinoma in liver resection patients. J Korean Med Sci 32:315–320
Rougemont AL, McLin VA, Toso C, Wildhaber BE (2012) Adult hepatoblastoma: learning from children. J Hepatol 56:1392–1403
Sharma D, Subbarao G, Saxena R (2017) Hepatoblastoma. Semin Diagn Pathol 34:192–200
Roth CG, Mitchell DG (2014) Hepatocellular carcinoma and other hepatic malignancies: MR imaging. Radiol Clin N Am 52:683–707
Tan Y, Xiao EH (2013) Rare hepatic malignant tumors: dynamic CT, MRI, and clinicopathologic features: with analysis of 54 cases and review of the literature. Abdom Imaging 38:511–526
An C, Park S, Choi YJ (2013) Diffusion-weighted MRI in intrahepatic bile duct adenoma arising from the cirrhotic liver. Korean J Radiol 14:769–775
Chen CB, Chou CT, Hsueh C, Lee KW, Chen YL (2013) Hepatic inflammatory pseudotumor mimicking hepatocellular carcinoma. J Chin Med Assoc 76:299–301
Kim JW, Shin SS, Heo SH, Lim HS, Hur YH, Kim JH (2013) Hepatic abscess mimicking hepatocellular carcinoma in a patient with alcoholic liver disease. Clin Mol Hepatol 19:431–434
Kleiner DE (2018) Hepatocellular carcinoma: liver biopsy in the balance. Hepatology 68:13–15
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Myeong-Jin Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Not applicable
Informed consent
Written informed consent was not required.
Ethical approval
Institutional Review Board approval was not required for this review.
Methodology
• Illustrative Review
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 4160 kb)
Rights and permissions
About this article
Cite this article
Kim, MJ., Lee, S. & An, C. Problematic lesions in cirrhotic liver mimicking hepatocellular carcinoma. Eur Radiol 29, 5101–5110 (2019). https://doi.org/10.1007/s00330-019-06030-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06030-0