Abstract
Objectives
The aim of this study is to investigate the correlation of survival outcomes with imaging biomarkers from multiparametric magnetic resonance imaging (MRI) in patients with brain metastases from breast cancer (BMBC).
Methods
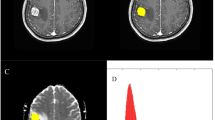
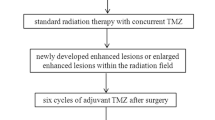
This study was approved by the institutional review board. Twenty-two patients with BMBC who underwent treatment involving bevacizumab on day 1, etoposide on days 2-4, and cisplatin on day 2 in 21-day cycles were prospectively enrolled for a phase II study. Three brain MRIs were performed: before the treatment, on day 1, and on day 21. Eight imaging biomarkers were derived from dynamic contrast-enhanced MRI (Peak, IAUC60, Ktrans, kep, ve), diffusion-weighted imaging [apparent diffusion coefficient (ADC)], and MR spectroscopy (choline/N-acetylaspartate and choline/creatine ratios). The relative changes (Δ) in these biomarkers were correlated with the central nervous system (CNS)-specific progression-free survival (PFS) and overall survival (OS) using the Kaplan-Meier and Cox proportional hazard models.
Results
There were no significant differences in the survival outcomes as per the changes in the biomarkers on day 1. On day 21, those with a low ΔKtrans (p = 0.024) or ΔADC (p = 0.053) reduction had shorter CNS-specific PFS; further, those with a low ΔPeak (p = 0.012) or ΔIAUC60 (p = 0.04) reduction had shorter OS compared with those with high reductions. In multivariate analyses, ΔKtrans and ΔPeak were independent prognostic factors for CNS-specific PFS and OS, respectively, after controlling for age, size, hormone receptors, and performance status.
Conclusions
Multiparametric MRI may help predict the survival outcomes in patients with BMBC.
Key Points
• Decreased angiogenesis after chemotherapy on day 21 indicated good survival outcome.
• ΔK trans was an independent prognostic factors for CNS-specific PFS.
• ΔPeak was an independent prognostic factors for OS.
• Multiparametric MRI helps clinicians to assess patients with BMBC.
• High-risk patients may benefit from more intensive follow-up or treatment strategies.




Similar content being viewed by others
Abbreviations
- 1H-MRS:
-
Proton magnetic resonance spectroscopy
- ADC:
-
Apparent diffusion coefficient
- Cho:
-
Choline
- CNS:
-
Central nerve system
- Cre:
-
Creatine
- DCE-MRI:
-
Dynamic contrast-enhanced magnetic resonance imaging
- DWI:
-
Diffusion-weighted imaging
- ECOG:
-
Eastern Cooperative Oncology Group
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- IAUC60 :
-
Initial area under curve for the first 60 s
- k ep :
-
Reflux constant
- K trans :
-
Volume transfer constant
- NAA:
-
N-acetylaspartate
- OS:
-
Overall survival
- Peak:
-
(maximal signal – baseline signal)/baseline signal
- PFS:
-
Progression-free survival
- PR:
-
Progesterone receptor
- ROI:
-
Region of interest
- v e :
-
Extravascular extracellular volume fraction
References
Ferlay J, Soerjomataram I, Ervik M et al (2014) GLOBOCAN 2012 v1.1, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available from: http://globocan.iarc.fr, accessed on 24/11/2017.
Arvold ND, Oh KS, Niemierko A et al (2012) Brain metastases after breast-conserving therapy and systemic therapy: incidence and characteristics by biologic subtype. Breast Cancer Res Treat 136:153–160
Matsuo S, Watanabe J, Mitsuya K, Hayashi N, Nakasu Y, Hayashi M (2017) Brain metastasis in patients with metastatic breast cancer in the real world: a single-institution, retrospective review of 12-year follow-up. Breast Cancer Res Treat 162:169–179
Brufsky AM, Mayer M, Rugo HS et al (2011) Central nervous system metastases in patients with HER2-positive metastatic breast cancer: incidence, treatment, and survival in patients from registHER. Clin Cancer Res 17:4834–4843
O'Connor JP, Jackson A, Parker GJ, Roberts C, Jayson GC (2012) Dynamic contrast-enhanced MRI in clinical trials of antivascular therapies. Nat Rev Clin Oncol 9:167–177
Lu YS, Chen TW, Lin CH et al (2015) Bevacizumab preconditioning followed by Etoposide and Cisplatin is highly effective in treating brain metastases of breast cancer progressing from whole-brain radiotherapy. Clin Cancer Res 21:1851–1858
Chen BB, Lu YS, Lin CH et al (2016) A pilot study to determine the timing and effect of bevacizumab on vascular normalization of metastatic brain tumors in breast cancer. BMC Cancer 16:466
Al-Okaili RN, Krejza J, Woo JH et al (2007) Intraaxial brain masses: MR imaging-based diagnostic strategy--initial experience. Radiology 243:539–550
Usinskiene J, Ulyte A, Bjornerud A et al (2016) Optimal differentiation of high- and low-grade glioma and metastasis: a meta-analysis of perfusion, diffusion, and spectroscopy metrics. Neuroradiology 58:339–350
Messiou C, Orton M, Ang JE et al (2012) Advanced solid tumors treated with cediranib: comparison of dynamic contrast-enhanced MR imaging and CT as markers of vascular activity. Radiology 265:426–436
Ellingson BM, Kim E, Woodworth DC et al (2015) Diffusion MRI quality control and functional diffusion map results in ACRIN 6677/RTOG 0625: a multicenter, randomized, phase II trial of bevacizumab and chemotherapy in recurrent glioblastoma. Int J Oncol 46:1883–1892
Boonzaier NR, Larkin TJ, Matys T, van der Hoorn A, Yan JL, Price SJ (2017) Multiparametric MR imaging of diffusion and perfusion in contrast-enhancing and nonenhancing components in patients with glioblastoma. Radiology 284:180–190
Oz G, Alger JR, Barker PB et al (2014) Clinical proton MR spectroscopy in central nervous system disorders. Radiology 270:658–679
Padhani AR, Miles KA (2010) Multiparametric imaging of tumor response to therapy. Radiology 256:348–364
Tofts PS, Brix G, Buckley DL et al (1999) Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging 10:223–232
Vuori K, Kankaanranta L, Hakkinen AM et al (2004) Low-grade gliomas and focal cortical developmental malformations: differentiation with proton MR spectroscopy. Radiology 230:703–708
Jung SC, Yeom JA, Kim JH et al (2014) Glioma: Application of histogram analysis of pharmacokinetic parameters from T1-weighted dynamic contrast-enhanced MR imaging to tumor grading. AJNR Am J Neuroradiol 35:1103–1110
Jung BC, Arevalo-Perez J, Lyo JK et al (2016) Comparison of glioblastomas and brain metastases using dynamic contrast-enhanced perfusion MRI. J Neuroimaging 26:240–246
Jalali S, Chung C, Foltz W et al (2014) MRI biomarkers identify the differential response of glioblastoma multiforme to anti-angiogenic therapy. Neuro Oncol 16:868–879
Gossmann A, Helbich TH, Kuriyama N et al (2002) Dynamic contrast-enhanced magnetic resonance imaging as a surrogate marker of tumor response to anti-angiogenic therapy in a xenograft model of glioblastoma multiforme. J Magn Reson Imaging 15:233–240
Hawighorst H, Knopp MV, Debus J et al (1998) Pharmacokinetic MRI for assessment of malignant glioma response to stereotactic radiotherapy: initial results. J Magn Reson Imaging 8:783–788
Chung WJ, Kim HS, Kim N, Choi CG, Kim SJ (2013) Recurrent glioblastoma: optimum area under the curve method derived from dynamic contrast-enhanced T1-weighted perfusion MR imaging. Radiology 269:561–568
Chen BB, Hsu CY, Yu CW et al (2011) Dynamic contrast-enhanced MR imaging measurement of vertebral bone marrow perfusion may be indicator of outcome of acute myeloid leukemia patients in remission. Radiology 258:821–831
Chen BB, Hsu CY, Yu CW et al (2017) Early perfusion changes within 1 week of systemic treatment measured by dynamic contrast-enhanced MRI may predict survival in patients with advanced hepatocellular carcinoma. Eur Radiol 27:3069–3079
Chen BB, Hsu CY, Yu CW et al (2016) Dynamic contrast-enhanced MR imaging of advanced hepatocellular carcinoma: comparison with the liver parenchyma and correlation with the survival of patients receiving systemic therapy. Radiology 281:454–464
Piludu F, Marzi S, Pace A et al (2015) Early biomarkers from dynamic contrast-enhanced magnetic resonance imaging to predict the response to antiangiogenic therapy in high-grade gliomas. Neuroradiology 57:1269–1280
O'Connor JP, Aboagye EO, Adams JE et al (2017) Imaging biomarker roadmap for cancer studies. Nat Rev Clin Oncol 14:169–186
Panebianco V, Iacovelli R, Barchetti F et al (2013) Dynamic contrast-enhanced magnetic resonance imaging in the early evaluation of anti-angiogenic therapy in metastatic renal cell carcinoma. Anticancer Res 33:5663–5666
Thoeny HC, Ross BD (2010) Predicting and monitoring cancer treatment response with diffusion-weighted MRI. J Magn Reson Imaging 32:2–16
Chang K, Zhang B, Guo X et al (2016) Multimodal imaging patterns predict survival in recurrent glioblastoma patients treated with bevacizumab. Neuro Oncol 18:1680–1687
Pope WB, Kim HJ, Huo J et al (2009) Recurrent glioblastoma multiforme: ADC histogram analysis predicts response to bevacizumab treatment. Radiology 252:182–189
Nguyen HS, Milbach N, Hurrell SL et al (2016) Progressing bevacizumab-induced diffusion restriction is associated with coagulative necrosis surrounded by viable tumor and decreased overall survival in patients with recurrent glioblastoma. AJNR Am J Neuroradiol 37:2201–2208
Zakaria R, Das K, Radon M et al (2014) Diffusion-weighted MRI characteristics of the cerebral metastasis to brain boundary predicts patient outcomes. BMC Med Imaging 14:26
Berghoff AS, Spanberger T, Ilhan-Mutlu A et al (2013) Preoperative diffusion-weighted imaging of single brain metastases correlates with patient survival times. PLoS One 8:e55464
Lee CC, Wintermark M, Xu Z, Yen CP, Schlesinger D, Sheehan JP (2014) Application of diffusion-weighted magnetic resonance imaging to predict the intracranial metastatic tumor response to Gamma Knife radiosurgery. J Neurooncol 118:351–361
Mardor Y, Roth Y, Lidar Z et al (2001) Monitoring response to convection-enhanced taxol delivery in brain tumor patients using diffusion-weighted magnetic resonance imaging. Cancer Res 61:4971–4973
Provenzale JM, Mukundan S, Barboriak DP (2006) Diffusion-weighted and perfusion MR imaging for brain tumor characterization and assessment of treatment response. Radiology 239:632–649
Garcia-Figueiras R, Baleato-Gonzalez S, Padhani AR et al (2016) Proton magnetic resonance spectroscopy in oncology: the fingerprints of cancer? Diagn Interv Radiol 22:75–89
Kugel H, Heindel W, Ernestus RI, Bunke J, du Mesnil R, Friedmann G (1992) Human brain tumors: spectral patterns detected with localized H-1 MR spectroscopy. Radiology 183:701–709
Kim H, Catana C, Ratai EM et al (2011) Serial magnetic resonance spectroscopy reveals a direct metabolic effect of cediranib in glioblastoma. Cancer Res 71:3745–3752
Li Y, Lupo JM, Parvataneni R et al (2013) Survival analysis in patients with newly diagnosed glioblastoma using pre- and postradiotherapy MR spectroscopic imaging. Neuro Oncol 15:607–617
Clarke JL, Molinaro AM, Phillips JJ et al (2014) A single-institution phase II trial of radiation, temozolomide, erlotinib, and bevacizumab for initial treatment of glioblastoma. Neuro Oncol 16:984–990
Pirzkall A, McGue C, Saraswathy S et al (2009) Tumor regrowth between surgery and initiation of adjuvant therapy in patients with newly diagnosed glioblastoma. Neuro Oncol 11:842–852
Park I, Tamai G, Lee MC et al (2007) Patterns of recurrence analysis in newly diagnosed glioblastoma multiforme after three-dimensional conformal radiation therapy with respect to pre-radiation therapy magnetic resonance spectroscopic findings. Int J Radiat Oncol Biol Phys 69:381–389
Nelson SJ, Li Y, Lupo JM, Olson M et al (2016) Serial analysis of 3D H-1 MRSI for patients with newly diagnosed GBM treated with combination therapy that includes bevacizumab. J Neurooncol 130:171–179
Funding
This study has received funding by the National Taiwan University (NTU-ICRP-103R7557 to Y.S.L.), Ministry of Science and Technology, Taiwan (MOST 103-2314-B-002-170-MY3 to Y.S.L.)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Tiffany Ting-Fang Shih.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Fu-Chang Hu, Sc.D., kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
All study subjects or cohorts have been previously reported.
This study is based on our previous works (Clin Cancer Res. 2015 Apr 15;21(8):1851-8; BMC Cancer. 2016 Jul 13;16:466. NCT01281696).
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Chen, BB., Lu, YS., Yu, CW. et al. Imaging biomarkers from multiparametric magnetic resonance imaging are associated with survival outcomes in patients with brain metastases from breast cancer. Eur Radiol 28, 4860–4870 (2018). https://doi.org/10.1007/s00330-018-5448-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5448-5